Guest Post: Diabetes Glastonbury
Diabetes Glastonbury
Read Rob’s post from day one and two
If you don’t know, Glastonbury is a gigantic music festival in the UK. Over 5 days it deatures 2,000 different acts on 90 different stages. A town with the population of Buffalo NY is built in the Somerset countryside and lasts for just a couple of weeks before the fields are handed back to the dairy cows. You can’t make a plan because things distract you as you try to carry it out, you always want to be in two places at once, there’s mega-walking to do (I racked up 50,000 steps over 3 days) and the very best things (Jennifer Mahammadi’s talk on day 2 for me) are a complete surprise.
Glastonbury tickets 2020: Deadlines, sale dates and everything you need ...
Okay, so maybe it’s not exactly like Glastonbury
Happily, like the Sunday of Glastonbury, Day 3 of the Diabetes UK Professional conference are a bit more relaxed. The opening session was about early onset Type 2 diabetes. Not really my thing, but Professor Helen Murphy spoke of the importance of preparing women with diabetes for pregnancy. A lot of us worry about that for ourselves and our daughters and it surprised me that I hadn’t come across this idea. Here’s the message: If you’re planning to get pregnant (i) take 5mg of foli acid daily (ii) get your HbA1c down as low as you can, ideally below 43 (6.1%) (iii) check with your primary care doctor about medications that aren’t great during pregnancy such as blood pressure control tablets or statins. These things massively improve the odds of a successful pregnancy, to roughly the same level as the general population.
HbA1c<43 = Best chance of healthy baby. And get some folic acid.
Later on we heard about the future of CGM use in diabetes care. Personally, I found it a bit frustrating in several ways. The medics still aren’t getting just how revolutionary Dexcom and Libre have been for us. The HbA1c U shaped mortality study was referenced a lot. In a nutshell this massive 10 year study in China found that mortality increased when HbA1c fell below 5.7% and it also increased when HbA1c was over 6.7%. The study impresses because of it’s 10 year duration and the 35,000+ patients who were part of it.
But in referring to it the medics are overlooking a pretty gigantic factor: In 2012 Dexcom released the G4. In 2015 Abbott release Libre. These devices had had an utterly dramatic impact on the lives of those of us with Type 1. They make the Chinese study unhelpful at best and actively misleading at worst. Despite at least 2 people with Type 1 setting out to the conference just how much difference these things can make, the message still isn’t getting through. In terms of mortality below HbA1c <5.7, it’s akin to relying on a study performed before insulin was discovered in 1922.
It’s scary that the sexiness of big science seems far more important to some doctors than the value of providing treatment to individual patients. Hey ho. Rant over.
Median HbA1c down from 73 to 61 in 13 years – Well done HCPs! (And patients? Maybe?)
The final session of the day was presented by Professor May Ng, Dr Tom Crabtree and Dr Clare Hambling. Tom spoke on the success of the NHS England pilot to see the effect of closed loops on HbA1c in practice, May of the reduction in HbA1c among children using these systems and Clare on how they might be rolled out in practice. An idea she trailed was that of a national (international) helpline expert in all the different systems. Doctors sign up to practice medicine rather than IT but my own experience of AID is that it’s the techy side that’s the bigger problem, not the medicine. Comfortingly May also identified that whilst the UK is doing really well on diabetes care Sweden is doing even better. She didn’t mention the U shaped mortality study…
Complications: HbA1c really, really matters
So, that’s it from me at this year’s Glastonbury Diabetes Professionals Conference. It was an incredible privilege to be amongst these impressive HCPs. Their brilliance and commitment to the cause was beyond question. There’s going to be a lot of patients getting better care next week as the connections and ideas exchanged this week feed back into front line practice.
BOB
Rob (Bob Dee) Darbyshire
Guest Post: Grande Challenges!
Grande Challenges!
I thought Day 2 of the Diabetes UK Professional Conference might be easier. Maybe get some lunch and not spend so much time on my feet. I was a bit wrong. (Read Day One from Rob)
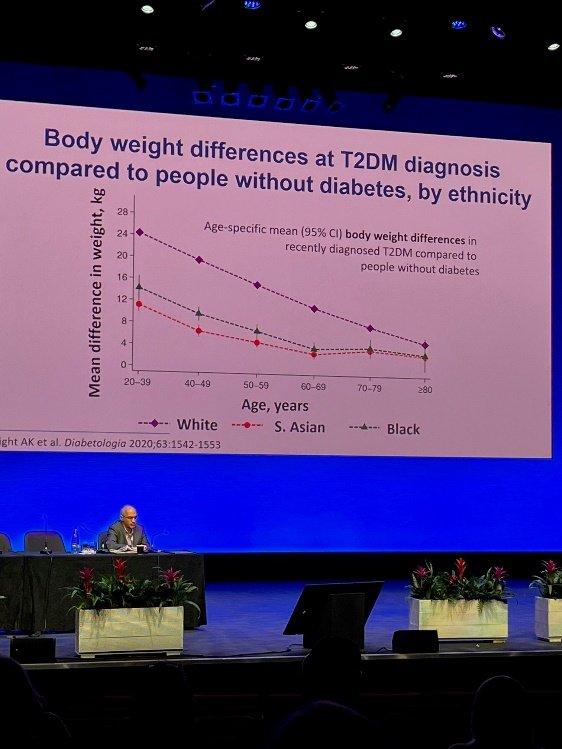
Ethnicity as a risk factor in T2
Today, I was able to spend more time in the presentations (and not just because I needed to sit down) mostly about diabetes causation and – drum roll - a cure. The day opened with an impressive lecture about the genetic links to diabetes. For me the takeaway was that Black and South Asian people develop type 2 when they’re skinnier than white people.
The rest of the morning I spent chatting with the awesome reps at Insulet and Dexcom. I got my hands on a Dexcom G7. It’s a real upgrade on my current Libre 2 because of the volume of real time data I could get out of it without a third party app. It’s small, really small, and much easier to apply than the G6. It may not seem important, but the box footprint is way smaller than the Libre 2 or the G6. This may sound trivial but with 3 Libre 2 users in the house, storage space is a genuine issue if we all get our scripts at the same time. Now I just need to persuade the kids to switch to Dexcom.
Omnipod 5 really is coming to the UK. And from what I heard, it may even be here sooner than we thought. The UK launch is going to be a “soft” one to avoid medics being hassled by all the current Dash and Eros users looking to upgrade. Cost shouldn’t be a barrier in the UK but appropriate staff training might be: HCP’s won’t be handing these out until they’ve been trained to use them.
The G7 is really, really tiny
After lunch we learned of the “Grand Challenge”. The Steve Morgan Foundation has donated an enormous £50 million to the prevention of T1 diabetes, and its cure through the development of robust stem cells that can grow into Beta Cells (without dying too quickly – that’s the barrier right now) and the development of smart insulins... that might be taken orally. As challenges go, “Grand” is an understatement.
Research on prevention seems the most advanced of these three things right now. Anyone who saw the slide I posted for the first day of the conference will recognise the increased risk of Type 1 among those with a family member already diagnosed. So far, as you can hear on Juicebox Podcast Episode #452, they’ve been able to delay the onset of Type 1 by around 2 years through the drug Teplizumab . As for a cure, it is progressing. As the implanted cells live longer and longer in their new homes, they present different problems over time. Slowly but surely, these problems are being overcome. As ever, we can look forward to a cure in ten years time… But real advances are being achieved already.
I finished the formal part of the day listening in to the discussions on eating disorders in diabetes. A shocking 40% of female teenage girls with type 1 in the UK suffer from a degree of diabulimia in which they consciously control their wait by avoiding injections. And it’s complex. We were addressed by the awe inspiring Jennifer Mahammodi. Jennifer was diagnosed at the age of 12. Her mother found it hard to help her manage with the result that there were a series of DKA hospital admissions – and Jennifer learned to associate those admissions with a time of caring and security, until she entered a cycle of almost fortnightly hospital admissions before being placed back into another foster care placement. Ultimately, living alone in social housing at the age of 19 she suffered, alone, a Christmas Day DKA episode so severe she could barely see. Thankfully, the adult care team at King’s College Hospital were able to provide psychological support and get her to a very much better place. It was a deeply moving address: amongst dozens of battle hardened HCPs there were very few dry eyes and it was the only address that I saw receive a standing ovation.
To cap off the day, I was invited to attend the presentation of a research award to Professor Roy Taylor. He’d been quite a presence at the conference putting questions to different panels with incisive intelligence and a dry wit. He pioneered the remission of Type 2 through rapid weight loss. As one of his colleagues pointed out to me, even if the diabetes isn’t remitted, weight loss is still a good idea for most Type 2s.
BOB
Rob (Bob Dee) Darbyshire