#1782 Charlotte Must Hate You - Part 1
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
Jen recounts her T1D diagnosis at age 29 and opens up about the emotional challenges of navigating family dynamics lacking understanding and support.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner (0:00) Friends, we're all back together for the next episode of the Juice Box podcast. (0:04) Welcome.
Jen (0:14) Well alright. (0:15) Well, hey, everybody. (0:16) I'm Jen, and I'm a type one. (0:19) I was diagnosed when I was 29, and I'm now 52.
Scott Benner (0:24) If this is your first time listening to the Juice Box podcast and you'd like to hear more, download Apple Podcasts or Spotify, really any audio app at all. (0:33) Look for the Juice Box podcast and follow or subscribe. (0:36) We put out new content every day that you'll enjoy. (0:40) Wanna learn more about your diabetes management? (0:42) Go to juiceboxpodcast.com up in the menu and look for bold beginnings, the diabetes pro tip series, and much more.
Scott Benner (0:49) This podcast is full of collections and series of information that will help you to live better with insulin. (0:57) How would you like to share a type one diabetes getaway like no other? (1:01) Join me on Juice Cruise 2026. (1:03) You may be asking, what is Juice Cruise? (1:05) It's a week long cruise designed specifically for people and families living with type one diabetes.
Scott Benner (1:10) It's not just a vacation. (1:12) It's a chance to relax, connect, and feel understood in a way that is hard to find elsewhere. (1:17) We're gonna sail out of Miami, and the cruise includes stops in CocoCay, San Juan, Saint Kitts, Nevis aboard the stunning Celebrity Beyond. (1:27) This ship is chosen for its comfort, accessibility, and exceptional amenities. (1:32) You're gonna enjoy a welcoming environment surrounded by others who get life with type one diabetes.
Scott Benner (1:38) I'm gonna host diabetes focused conversations and meetups on the days at sea. (1:42) There's thoughtfully designed spaces, incredible dining, and modern amenities all throughout the celebrity beyond. (1:50) Your kids can be supervised, there's teen programs so everyone gets time to recharge. (1:55) Not just the the kids going on vacation, but maybe you get the kickback a little bit too. (2:00) There's gonna be zero judgment, real connections, and a whole lot of sun and fun on Juice Cruise twenty twenty six.
Scott Benner (2:06) Please come with me. (2:07) You're going to have a terrific time. (2:09) You can learn more or set up your deposit at juiceboxpodcast.com/juicecruise. (2:15) Get ahold of Suzanne at cruise planners. (2:17) She will take care of everything.
Scott Benner (2:19) Link's in the show notes. (2:20) Link's at juiceboxpodcast.com. (2:23) Nothing you hear on the juice box podcast should be considered advice, medical or otherwise. (2:27) Always consult a physician before making any changes to your health care plan. (2:33) This episode of the Juice Box podcast is sponsored by US Med, usmed.com/juicebox, or call (888) 721-1514.
Scott Benner (2:44) Get your supplies the same way we do from US Med. (2:48) Today's episode is also sponsored by Omnipod five. (2:52) Omnipod five is a tube free automated insulin delivery system that's been shown to significantly improve a one c and time and range for people with type one diabetes when they've switched from daily injections. (3:04) Learn more and get started today at omnipod.com/juicebox. (3:08) At my link, you can get a free starter kit right now.
Scott Benner (3:11) Terms and conditions apply. (3:12) Eligibility may vary. (3:14) Full terms and conditions can be found at omnipod.com/juicebox.
Jen (3:18) Well alright. (3:19) Well, hey, everybody. (3:20) I'm Jen, and I'm a type one. (3:23) I was diagnosed when I was 29, and I'm now 52. (3:28) And so I'm pretty sure that was twenty three years ago Wow.
Jen (3:30) If I'm doing my math right. (3:31) Yes. (3:32) So
Scott Benner (3:33) It sounds right to me.
Jen (3:34) Here today.
Scott Benner (3:34) Because if I get 29, I add 10, I get 39. (3:37) Then I add 10 more, I get 49. (3:39) Then I start counting by ones. (3:40) So I get 20, and then I go 5051, 52. (3:44) That's three.
Scott Benner (3:44) I add the 20 and the three together, I get 23.
Jen (3:46) Yay. (3:47) Okay.
Scott Benner (3:47) It's that easy. (3:49) People might have thought because of your southern accent, you couldn't add, but that would just be a rude, rude misconception.
Jen (3:54) Wouldn't that be so rude? (3:55) I know. (3:56) Mhmm. (3:56) I know. (3:57) I am worried about the accent, but you tell me if you don't understand something I'm saying.
Scott Benner (4:01) You think I'm not gonna understand something you're saying?
Jen (4:03) Well, it may be something well, I wanted to say this to you. (4:07) You know, when you say very, like very Mhmm. (4:10) You you use a u. (4:11) You're like very. (4:12) And then I just think it's really cute.
Jen (4:14) I just want you to you to know that.
Scott Benner (4:15) Well, thank you. (4:16) I don't
Jen (4:16) You're very welcome.
Scott Benner (4:17) I have no idea what I'm doing.
Jen (4:19) I do. (4:20) But, like, you always say very, like, v u r y instead of very.
Scott Benner (4:24) You sound you sound like I'm checking into a hotel on my way to visit somebody in the South.
Jen (4:29) Exactly.
Scott Benner (4:30) I want you to tell me that there's a warm cookie in my room right now.
Jen (4:34) For sure.
Scott Benner (4:36) Born and raised there? (4:38) You?
Jen (4:39) Yeah. (4:39) I'm in yeah. (4:40) I live in Charlotte, North Carolina. (4:41) And so I was I grew up in a small town outside of Charlotte. (4:45) So
Scott Benner (4:46) You were born there? (4:47) Yes. (4:48) Are you guys tired of our people coming and overtaking your state?
Jen (4:52) Tired of it. (4:52) It's ridiculous. (4:54) Yes. (4:54) I'm so tired of it.
Scott Benner (4:56) Can I tell you? (4:56) No kidding. (4:57) People I've known, like, my whole, like, adult life, like, kids played softball with my daughter and baseball with my son and they're just fantastic people. (5:07) And one day, a for sale sign goes up in the yard. (5:10) And I stopped by and I go, what what what's happening?
Scott Benner (5:13) You know, I'm I'm like, if you leave, what does that mean? (5:16) I I gotta go. (5:17) You know? (5:18) And there's a note where their last kid they have four kids. (5:22) Their last one is playing softball in North Carolina.
Scott Benner (5:25) And they're like, we're just gonna move there and go to softball games for a couple of years until she graduates because she's been down there for a little while already.
Jen (5:33) Mhmm.
Scott Benner (5:33) And, then we think we're gonna stay.
Jen (5:35) Wow.
Scott Benner (5:36) And I said, it seems kinda quick. (5:39) They said, not just quick. (5:40) We have to move into an apartment. (5:41) We don't have a place to live.
Jen (5:44) That's funny.
Scott Benner (5:45) I go, where are you gonna move to? (5:46) Like, you know, you must you know the area, obviously. (5:48) No. (5:49) No. (5:49) We have a friend that moved there, said this one area is pretty nice.
Scott Benner (5:52) We're just gonna go there, rent an apartment, then we'll look around and find a house later.
Jen (5:55) Wow.
Scott Benner (5:55) And I was like, the people of North Carolina must hate you.
Jen (5:59) Wait. (5:59) Yeah. (5:59) Well, it's it's like Charlotte doesn't look the same at all. (6:03) Like, ten year and just in the last ten years, it's changed so much. (6:06) So
Scott Benner (6:07) I wouldn't imagine. (6:08) Yeah. (6:08) Well okay. (6:09) Well, I don't know what to do. (6:10) I can't I mean, I can command everyone to come back, but I don't think they're gonna listen.
Jen (6:14) I don't think so either. (6:16) It's okay. (6:17) It's okay.
Scott Benner (6:17) In fairness, I was looking at a house in Tennessee the other day. (6:20) So What? (6:22) Yeah. (6:23) It's a very reasonable tax situation in Tennessee. (6:25) I don't know if you're under
Jen (6:26) It is fair better, but it's definitely humid here. (6:28) I know I don't like humidity. (6:29) So
Scott Benner (6:30) But I gotta decide what do I like better, humidity or money? (6:33) You know? (6:34) Or
Jen (6:34) snow. (6:35) Mhmm. (6:36) Yeah.
Scott Benner (6:36) Anyway, I'm seriously considering it. (6:38) There's no there's no income tax in Tennessee.
Jen (6:42) Oh, I didn't know that.
Scott Benner (6:43) Uh-huh. (6:44) No. (6:44) Think about how much money you make, and then think about how much money you pay in income tax to the state, and then decide what would that be like if it was yours.
Jen (6:51) Yeah. (6:52) So when you're sitting in the humidity in July, you go, I'm saving money.
Scott Benner (6:55) You know, like that money and and turn the air conditioner on with it. (6:58) That's what I was gonna do. (6:59) Anyway
Jen (7:00) alright. (7:01) I love it. (7:02) Okay.
Scott Benner (7:02) 20 not you know, is a an interesting age. (7:06) You would think you felt probably pretty settled. (7:08) Had you had other health issues leading up to that, or was it just like a bell rang and you had diabetes?
Jen (7:14) Yeah. (7:15) I had really no issues before then. (7:18) I had no seasonal allergies. (7:20) Started about age 18.
Scott Benner (7:22) Mhmm.
Jen (7:22) So what? (7:23) Eleven years of that? (7:24) That's really it. (7:26) And so I remember when, like, the weekend before I was diagnosed, I was I felt sick, but I didn't have a fever. (7:36) You know?
Jen (7:36) I was like, I'm I'm not sick, but I'm sick. (7:39) And it was Memorial weekend, I remember. (7:42) And I remember I had a chance to go out on a boat. (7:45) Yeah. (7:46) And I didn't feel like going on a boat.
Jen (7:47) I'm like, something's wrong with me. (7:48) And and I was like, no. (7:50) I just don't have the energy. (7:51) And back in the day, in 2002, we still had Blockbuster. (7:55) So I thought, you know what?
Jen (7:56) I'm gonna go to Blockbuster. (7:57) I'm gonna rent some movies, you know, and because I'm so old. (8:00) You know? (8:01) And I remember driving, and all of a sudden, I couldn't see. (8:05) I couldn't read the street sign.
Jen (8:06) Like, it was blurry. (8:07) And I went, oh my god. (8:08) This is weird. (8:09) And and I also, like, on that little excursion, I remember I went to Target just to grab grab a couple things. (8:17) And I've always been really healthy, never drank sodas, anything like that.
Jen (8:21) And I look in the aisle, and there's a Mountain Dew code red. (8:25) And I went, oh my god. (8:27) I've gotta have this thing. (8:28) And I never had anything like that before. (8:31) So I'm, like, in the car in the parking lot.
Jen (8:33) I'm down on this Mountain Dew. (8:35) And that weekend, I had a whole gallon of milk by myself. (8:37) I had a whole thing of orange juice by myself. (8:40) I lived with my sister at the time, so it was just me and her. (8:43) And and so, I mean, I'm drinking all this, you know, just the normal stuff.
Jen (8:47) And I remember about three weeks prior to this, I was losing weight. (8:51) I'm like, dang. (8:52) I'm starting to look good. (8:53) Like, you know, like, I could see my muscles, you know, and all this stuff. (8:56) And I had just started playing tennis in May, you know, April, May, and I thought, wow.
Jen (9:00) Tennis. (9:01) Where has it been my whole life? (9:02) This is what I should have been doing this whole time.
Scott Benner (9:05) The missing ingredient.
Jen (9:06) Missing ingredient is tennis. (9:08) Tennis and
Scott Benner (9:08) Mountain Dew.
Jen (9:10) And Mountain Dew. (9:11) And so, anyway, so I remember, you know, I lost the weight. (9:15) I'm eating really, you know, a lot. (9:16) I'm like, this is great. (9:18) Tennis you know, again, tennis is a thing.
Jen (9:20) And and so then I'm back to the weekend. (9:23) I'm drinking all this, you know, using the bathroom all the time, the whole thing. (9:26) And then I I don't know. (9:29) I had this this suspicion when I put it all together. (9:32) I didn't know anyone's any anyone with diabetes.
Jen (9:35) And I thought, do I have diabetes? (9:37) And I'm like, why would I think that? (9:39) And then I remembered I have a friend who grew up with a type one, and I remember her talking about her years ago. (9:45) And I thought, So I called my friend, and she I talked to her about it. (9:50) She goes, it does sound very interesting.
Jen (9:52) You know? (9:53) I think you need to talk to my friend Gina who lived in Charlotte where I live. (9:57) And so I was like, okay. (9:59) So the next morning, I went to this stranger's house and, you know, I don't know, ten minutes down the road, and she had texted me and said, don't eat anything. (10:09) Don't you know, like, just come over to my house.
Jen (10:11) And it was, like, 08:30 in the morning. (10:12) I'm like, okay. (10:13) So I go over to her house. (10:14) It was a Monday morning, and she checks my blood sugar. (10:18) And I think it was, like, upper three hundreds, 400.
Jen (10:21) I don't know. (10:21) And it was I was fasting. (10:23) And she looked at me, and I still remember. (10:26) She looked at me. (10:27) She looked down and she looked at me.
Jen (10:28) She said, I'm sorry to say, but you've got type one diabetes. (10:33) And I went, what? (10:34) And, you know, I didn't even know what it meant, obviously. (10:37) And she said, uh-huh. (10:38) And I'm going to I want you to leave your car here at my house, and I'm gonna take you to the ER.
Jen (10:43) And I'm with the ER. (10:45) And she goes, mhmm. (10:46) And she said, I can smell your I know I know you don't understand this, but your breath is fruity. (10:51) And so that's telling me you need to go to the hospital. (10:55) Right?
Jen (10:55) I'm like, what? (10:56) And, I mean, I was on my way. (10:57) I was a a server. (10:59) I was a waitress at the time. (11:00) I'm like, I'm on my way to work.
Jen (11:01) I gotta shift to work. (11:02) Shoot. (11:02) I gotta lunch to work. (11:03) And she's like, no. (11:04) No.
Jen (11:04) No. (11:04) You're not going into work. (11:06) So that's how it started, how I ended up in the hospital in the ER. (11:11) And I remember, you know, in the ER, the doctors I'm sure they were residents. (11:16) This is a teaching hospital, but they came in and they I remember them saying, you're too skinny to be a type two.
Jen (11:24) I mean, oh, yeah. (11:25) Type two, but you're too old to be type one. (11:28) And I'm like, okay. (11:29) Cool. (11:29) You know?
Jen (11:30) And then finally, I they, you know, they finally said I don't know what they did to test it, obviously. (11:37) I don't I didn't understand anything back then, but they did finally decide I was a type one. (11:41) I had to spend the night, the whole thing. (11:44) And so part of the reason I wanted to come on this podcast, one, because I love this podcast. (11:48) And when I signed up months ago, you were, like, looking for people, and that's, you know, that's really I was like, oh, well, I have a story.
Jen (11:54) I can tell it. (11:55) But I feel like being an adult, single, you're I'm old enough to kind of, you know, be on my own, but I was clueless. (12:04) There was hardly any support for me. (12:07) I was in the hospital. (12:08) I was in for a day.
Jen (12:10) I remember they came in with the orange and the syringe and made sure I could do that. (12:15) And the doc I think the endo came in and talked to me and said, these are the pins you're gonna take home. (12:21) And all I remember is, you know I I just remember going, I don't know what to eat. (12:26) You know, like, I was so afraid to go home.
Scott Benner (12:29) Yeah.
Jen (12:29) But I did. (12:30) I went home, obviously. (12:32) And like I said, I was waiting tables, no insurance. (12:37) It was not good, but that's how it started out. (12:40) So it was very, very scary
Scott Benner (12:42) Wow.
Jen (12:43) To try to manage.
Scott Benner (12:44) Did that stranger stay with you in the hospital, or did they go, okay. (12:47) Well, goodbye.
Jen (12:48) Oh, yeah. (12:49) That's a good point. (12:49) She did stay with me.
Scott Benner (12:50) Very nice.
Jen (12:51) Yeah. (12:52) Until
Scott Benner (12:53) Your sister.
Jen (12:53) My family got there. (12:54) Yeah. (12:55) I've got three sisters. (12:56) They showed up. (12:57) My mom, my dad, they all showed up.
Jen (12:59) You know, everybody showed up in the ER, and they were very supportive and were with me. (13:03) And then Gina, the lady who helped me, she obviously left because, you know, she's like, I think you're good now. (13:10) You know?
Scott Benner (13:10) I I was just testing your blood sugar for a friend. (13:13) I didn't I
Jen (13:14) wasn't really planning on being in the ER all day.
Scott Benner (13:17) I wasn't looking for all this, but I am gonna go to I am gonna head over to the the Red Lobster and pick up a shift. (13:22) So Exactly. (13:23) Right? (13:24) I I they're looking for people.
Jen (13:25) Oh my god.
Scott Benner (13:26) Wow. (13:26) That's and that does that feel like it just happened, or does it feel like a million years ago?
Jen (13:31) Both. (13:32) It feels like a different lifetime. (13:34) You know? (13:35) Like, I I don't know. (13:36) It just feels almost like a dream back then, but I can remember every second of it at the same time.
Jen (13:42) I remember I remember being in the hospital, and my you know, it's sort of like our pattern. (13:48) My sisters and I, we laugh a lot, which is a great thing, obviously. (13:52) And I remember the doctors coming in going, y'all were, like, the happiest people. (13:55) Like, you're the happiest type one I've ever met. (13:57) You know?
Jen (13:57) Like, because we were just laughing and, you know, just they were trying to keep me upbeat. (14:02) And I think I was in shock, and, of course, my blood sugars are high, I'm not thinking clearly. (14:07) Yeah. (14:07) And I didn't really know what anything meant, but I do remember that. (14:11) You know, there was just a lot of laughter, laughter, a lot of
Scott Benner (14:13) Support.
Jen (14:14) You know, oh, dear. (14:15) How are we gonna handle this? (14:16) There was support, but I think that's all they knew to do, which was great.
Scott Benner (14:19) What what is it? (14:20) Both your parents are they together at that point?
Jen (14:23) They they divorced when I was 13, 14.
Scott Benner (14:27) Which one comes to the hospital?
Jen (14:29) They both came.
Scott Benner (14:30) They both did. (14:30) Yeah. (14:31) But it must have been fun.
Jen (14:32) Yeah. (14:33) Well, they actually get along fine. (14:34) You know? (14:35) They yep. (14:36) There's they're very civil.
Jen (14:37) We still do holidays together, believe it or not. (14:39) But yeah. (14:41) So they were fine. (14:42) Yep. (14:42) And and everything.
Scott Benner (14:45) Do you ever have any conversations with them? (14:46) Like, either of them, honestly. (14:48) Like, you're 29. (14:49) You're, you know, pretty you know? (14:51) Like you said, it it's interesting.
Scott Benner (14:52) Like, you're grown, but in your mind, you're like, I'm I'm not that grown. (14:56) I don't know a lot still.
Jen (14:57) Right.
Scott Benner (14:58) You know? (14:58) But do your parents feel like, did they slip back into being parents? (15:03) Or do they just go like, well, good luck. (15:05) Let us know how it goes? (15:06) Or do they feel like, gosh, do you need help?
Scott Benner (15:09) Like, what can we do something? (15:12) Today's episode is brought to you by Omnipod. (15:15) We talk a lot about ways to lower your a one c on this podcast. (15:19) Did you know that the Omnipod five was shown to lower a one c? (15:23) That's right.
Scott Benner (15:24) Omnipod five is a tube free automated insulin delivery system, and it was shown to significantly improve a one c and time and range for people with type one diabetes when they switched from daily injections. (15:36) My daughter is about to turn 21 years old, and she has been wearing an Omnipod every day since she was four. (15:42) It has been a friend to our family, and I think it could be a friend to yours. (15:46) If you're ready to try Omnipod five for yourself or your family, use my link now to get started. (15:53) Omnipod.com/juicebox.
Scott Benner (15:55) Get that free Omnipod five starter kit today. (15:58) Terms and conditions apply. (16:00) Eligibility may vary. (16:01) Full terms and conditions can be found at omnipod.com/juicebox. (16:07) You've probably heard me talk about US Med and how simple it is to reorder with US Med using their email system.
Scott Benner (16:13) But did you know that if you don't see the email and you're set up for this, you have to set it up. (16:18) They don't just randomly call you. (16:19) But I'm set up to be called if I don't respond to the email because I don't trust myself, a 100%. (16:25) So one time, I didn't respond to the email and the phone rings at the house. (16:30) It's like, ring, you know how
Jen (16:31) it works.
Scott Benner (16:31) And I picked it up. (16:32) I was like, hello? (16:33) And it was just the recording. (16:34) It was like, US Med, doesn't actually sound like that, but you know what I'm saying. (16:37) It said, hey, you're, I don't remember exactly what it says, but it's basically like, hey, your order's ready.
Scott Benner (16:42) You want us to send it? (16:43) Push this button if you want us to send it. (16:45) Or if you'd like to wait, I think it it lets you put it off, a couple of weeks or push this button for that. (16:50) That's pretty much it. (16:51) I push the button to send it, and a few days later, box right at my door.
Scott Benner (16:56) That's it. (16:56) Usmed.com/juicebox or call (888) 721-1514. (17:01) Get your free benefits checked now and get started with USmed. (17:05) Dexcom, Omnipod, Tandem, Freestyle, they've got all your favorites. (17:11) Even that new islet pump.
Scott Benner (17:13) Check them out now at usmed.com/juicebox or by calling (888) 721-1514. (17:22) There are links in the show notes of your podcast player and links at juiceboxpodcast.com to US Med and to all of the sponsors.
Jen (17:29) They did not. (17:30) They I love my parents. (17:32) They're young parents. (17:33) They're only twenty years older than me. (17:34) So and I'm the oldest, so I've always been very responsible.
Jen (17:37) Mhmm. (17:38) So they're kinda like, oh, good. (17:39) It's Jen got diabetes. (17:41) You're not the other three. (17:42) Yeah.
Jen (17:42) She'll be fine.
Scott Benner (17:43) And, god, it wasn't that one. (17:45) Oh my god.
Jen (17:46) Wasn't that one.
Scott Benner (17:46) Yeah. (17:47) Yeah. (17:47) Get in trouble.
Jen (17:48) Yeah. (17:48) So I had been my own parents since I was, like, 12 or 10 or whatever. (17:53) So I see. (17:53) No. (17:54) They and they so they love me, but they still even twenty three years later, that's part of what I wanted to mention on this too.
Jen (18:01) I don't wanna bounce around too much.
Scott Benner (18:02) But You're fine.
Jen (18:03) Part of my the hard part of this is feeling even though I have this community and I'm on the Facebook group and the whole thing, I still feel very alone within my family. (18:14) Mhmm. (18:15) You know? (18:15) And, like, one sister's gluten free and has been for about the same amount of time as me, you know, the twenty years or whatever. (18:22) And they're all they're knocking over the door to make her a gluten free, you know, meal or dessert or whatever.
Jen (18:29) And for me, they're not doing anything. (18:31) Even when I was new into this, you know, not knowing what I was doing or how to use insulin. (18:35) Yeah. (18:36) You know? (18:36) So that hurts a little bit.
Jen (18:37) I'm like, her stomach just hurts. (18:39) I could die. (18:40) You know? (18:40) So
Scott Benner (18:41) Do you think are they they just feel like you have the sugars? (18:45) Is it, like, oversimplified?
Jen (18:47) They're not that ignorant. (18:48) No. (18:49) They know. (18:49) But I think it's just, unfortunately, I've always been so responsible. (18:54) Oh.
Jen (18:54) And I will admit, I, you know, I I like I mean, I like people thinking I'm responsible, so that's part of it. (19:01) I don't ask for help a lot, and and it's hard for me to admit when I need help. (19:06) And so I that I'm part of the problem, and I do admit that. (19:11) And I know that about my personality.
Scott Benner (19:12) It's partially that they think, oh, Jen's got this. (19:17) She's always got it. (19:18) But it's also because they probably learned to be okay with that because you kept them at arm's length at times?
Jen (19:23) Yes.
Scott Benner (19:24) Okay.
Jen (19:24) For sure. (19:25) Yeah. (19:25) Yeah. (19:25) Yeah. (19:25) For sure.
Jen (19:26) And I didn't want to burden anybody, you know, because it's it's like, being type one, it's sort of like your whole life, but you don't wanna make it your whole life. (19:35) You know? (19:36) Because it's not. (19:36) It is and it's not. (19:38) And so it's it's like, I don't know in the beginning, and still, I don't wanna over talk about it, but sometimes I do wanna talk about it because it's a you know, I go through stuff.
Jen (19:49) And then when I try to talk about it or, like, the other day over the holiday, I had to change I wear the Omnipod Dash, and I use the Trio system. (19:59) And so I I my sugars were going up, and I'm like, oh, shoot. (20:03) I I I this is about the end of this pod. (20:05) I probably need to go ahead and change it. (20:06) So we're all sitting around playing games, and I just pull out my pod and my insulin and the whole thing.
Jen (20:13) And my nine year old nephew is looking and, you know, wondering kinda what I'm doing. (20:19) And I've shown him before, but I was trying to explain it to him. (20:21) This is my insulin pump and the insulin and blah blah blah. (20:26) And he was listening a little bit, but the rest of the family, I don't know. (20:29) They just sort of go, whatever.
Jen (20:31) It's no big deal. (20:33) And and I had some family members that aren't my immediate family were there, and I said, yeah, guys. (20:39) I could if I don't have this insulin, I could die in a day or two. (20:42) Know, I was just trying to be and they were just like,
Scott Benner (20:44) Okay. (20:44) Fascinating.
Jen (20:45) And fat no. (20:46) They just kept going. (20:47) And I'm like, seriously? (20:48) And I just had the big the next day, I just cried and cried and cried to my wife. (20:54) And I was like, I know I sound like a big baby, but it just hurts sometimes when something is, I don't know, so important and yet it's also in the background.
Jen (21:05) And it I don't know. (21:05) So I have this weird relationship with diabetes and my family. (21:09) And so I
Scott Benner (21:10) you know? (21:11) Let's pick let's pick through it a a second. (21:13) So Yeah. (21:13) Yeah. (21:13) You have a weird relationship with diabetes, which means
Jen (21:16) Yes.
Scott Benner (21:16) You don't want it to be anything people think about, but it would be nice if somebody thought about it once in a while.
Jen (21:23) Ridiculous. (21:23) Right? (21:24) But yes.
Scott Benner (21:24) No. (21:24) I I I understand what you're saying. (21:26) You don't wanna be begging for it, but it would be nice if once in a while they looked over you. (21:30) I so I'll share. (21:33) Right?
Scott Benner (21:34) The other day
Jen (21:36) Mhmm. (21:36) Mhmm.
Scott Benner (21:37) I I don't know. (21:39) Jen, listen. (21:40) I don't get high. (21:42) I don't drink. (21:43) I don't cheat.
Scott Benner (21:44) I don't hit people. (21:45) Like, all the stuff that happen I hear people's lives every day. (21:49) Like, I get up, I do the thing I'm supposed to do, I save money, I plan for the future, I put people before me. (21:56) I'm in the middle of doing something. (21:58) Arden says to me, hey, can you come here?
Scott Benner (22:00) I drop what I'm doing. (22:01) I go with her. (22:02) My son says to me last night, I gotta go to the airport for my job. (22:05) I said, when do you gotta leave? (22:07) He said, 05:30AM.
Scott Benner (22:09) No problem. (22:09) Went to bed early, got up at five, was there waiting for him at 05:30, got in the car, drove him an hour to the airport, drove an hour back. (22:17) I'm gonna go back and pick him up again tomorrow night. (22:19) I don't think twice about it. (22:20) Wow.
Scott Benner (22:21) I don't expect them to say thank you. (22:23) I don't want them to say thank you. (22:25) I believe that I am being myself in this situation. (22:29) However, I look at the rest of the world once in a while, and I think, you're all pretty lucky. (22:35) This is who I am.
Scott Benner (22:36) I I don't need you to tell me. (22:37) I don't even want you to tell me, but goddamn, no one ever says it. (22:41) Is that how you feel? (22:42) Is that how you feel? (22:43) Yes.
Jen (22:43) Yes. (22:43) It's exactly how I feel. (22:44) Yeah. (22:44) And, you know, I your kids are so lucky. (22:48) Those They're
Scott Benner (22:49) so Yeah. (22:50) Goddamn right. (22:51) Well, I hope they're listening.
Jen (22:52) Oh, I do too. (22:54) Shame on them for not listening. (22:55) Yeah.
Scott Benner (22:56) I need the downloads. (22:57) What's their problem?
Jen (22:57) Seriously, dudes. (22:58) Come on. (22:59) But yeah. (23:00) So, like, when I first started listening, my friend Kelly, she was on your podcast, talked about Afrezza Mhmm. (23:05) About a year ago.
Jen (23:06) But, anyway, she told me about you about two years ago. (23:09) I never even once thought about listening to a diabetes podcast. (23:12) I don't know why, but I didn't. (23:13) And now I'm obsessed. (23:14) But I started she said, the pro series a thousand to a 25 or whatever.
Jen (23:18) I'm like, okay. (23:19) And so I did it. (23:20) But at the time when I listened, I was on Afrezza. (23:24) And, you know, you know, you're not big on Afrezza. (23:27) And so like, well, this has nothing to do with me.
Jen (23:29) He's talking about prebolasane and having to worry about insulin being in your system when you exercise, and that had that's not how it is with Afrezza.
Scott Benner (23:36) Right.
Jen (23:36) And so I'm like, ugh. (23:38) And I tried, but I just I I couldn't get a whole lot out of it. (23:42) And and so I was a little bit resentful that there was nothing else besides normal insulin. (23:47) And then I heard how good you what a good parent you are. (23:51) And I'm like, dang it.
Jen (23:53) Like because we're, the same age. (23:54) You're, like, a year older than me. (23:56) And I'm like, I want him to I don't want you to be my dad, but I want you to have a dad like you. (24:00) You know? (24:00) And I'm like, wow.
Jen (24:01) Those kids have no idea what this man does for him, for them.
Scott Benner (24:06) Jen, my point is is that I and I mean this genuinely. (24:09) I'm not looking for anybody to say thank you.
Jen (24:11) Not. (24:12) I know you're not. (24:12) I I understand that. (24:14) I know that's not why you do it. (24:15) But every once in a while
Scott Benner (24:17) Right.
Jen (24:17) Thank you, dad. (24:19) Thanks.
Scott Benner (24:19) And I'm not gonna say it doesn't every like, I wasn't where was I with Cole recently? (24:24) And he Cole said something that made me realize he's didn't say it, say it, but what he was saying was, man, I recognize that making that podcast as big as it is is pretty extraordinary. (24:38) Like, he kind of gave me that for a half because he didn't use all the words, but he get like, he gave it to me. (24:42) And I was like, oh, he's proud of me, And that's nice. (24:44) You know what I mean?
Scott Benner (24:45) Like or he recognizes what hard work does or being diligent, you know, whatever. (24:50) Mhmm. (24:51) But, yeah, I don't know I don't know. (24:53) Like so my point is this, is that I think I feel like I understand what you're saying, which is I do my thing. (25:01) I take care of my diabetes.
Scott Benner (25:02) I don't want it to be my whole life. (25:04) I am not even looking for you to mention it, but, man, there are moments when how come you can't see how much I need you to say you're doing a great job? (25:15) Or, wow. (25:15) That is really something, Jen. (25:17) We're all over yucking it up playing Yahtzee, and you're strapping your man made, you know, pancreas on.
Scott Benner (25:23) So my question to you is, so you've ever said that to anybody? (25:26) Mm-mm. (25:27) Like, how would they know? (25:29) If you're projecting strength all the time and I got it, I got it, I got it, why would they think you needed, like, the that a boy?
Jen (25:36) Yeah. (25:36) I knew you're gonna ask that. (25:38) But well okay. (25:39) So indirectly because, you know, I'm southern. (25:41) We we're indirect.
Jen (25:42) I, you know, I have the supplies out. (25:44) And so it's sort of like to me, I'm like, hey. (25:48) I'm showing it to you. (25:49) I'm not in a bathroom. (25:51) You know what I mean?
Jen (25:52) Like, I'm not over here, like, hiding this. (25:54) And so I feel like Mhmm. (25:58) That is a perfect time for just just for them to ask to have some curiosity. (26:02) That's all I'm ask you know, like, to ask about it.
Scott Benner (26:05) What's southern passive aggressiveness called? (26:07) Does it have a name?
Jen (26:09) I don't know. (26:10) What it called
Scott Benner (26:11) What is it called when you guys go, oh, bless your heart?
Jen (26:14) Bless their heart.
Scott Benner (26:15) Yeah. (26:15) What is that? (26:15) What what is that? (26:16) That's
Jen (26:17) That's just us being very sarcastic. (26:19) Okay. (26:19) Like, we're saying bless your I don't really say that, but bless your heart, and we're really judging you at the same you know, we're really judging you, but we're saying, well, bless them.
Scott Benner (26:27) Yeah. (26:27) Look at this idiot. (26:28) Is that what that means?
Jen (26:29) This idiot. (26:29) Yeah. (26:30) It means, oh my god. (26:31) They are so ridiculous. (26:32) Yes.
Jen (26:33) Yes. (26:34) So I understand. (26:36) I I I guess okay. (26:37) This is what I have done. (26:38) K?
Scott Benner (26:38) Go ahead.
Jen (26:39) Okay. (26:39) Okay. (26:39) One sister who's two years younger than me, I have asked her to follow me. (26:43) Okay? (26:44) Like, she and my wife follow me.
Scott Benner (26:46) Okay.
Jen (26:46) And she started doing that because my wife used to, you know, leave for two weeks for work, and I'd be by myself. (26:52) Mhmm. (26:53) And they were worried about me, and so my sister Jill would would follow me. (26:58) And it it you know, and so every once in while, she'll text me and say, hey. (27:03) You're heading straight down.
Jen (27:04) Are you good? (27:05) You know? (27:05) And so That's beautiful. (27:06) I do like that. (27:07) I really do appreciate that.
Jen (27:09) She's probably the one family member that's really made some sort of effort about it. (27:15) But if I really start not complaining, but talking about the hard parts of it, she will will shut me down. (27:23) Like, oh my god. (27:24) You're complaining. (27:25) Or Mhmm.
Jen (27:26) You know what? (27:26) I don't know how to explain it, but it's it's like they want me to be responsible. (27:31) They want me to be okay. (27:32) And when I'm not okay,
Scott Benner (27:34) prefer if you shut up and kept it to yourself.
Jen (27:36) Yes. (27:36) Yes. (27:37) They don't know how to handle that because this is the dynamic. (27:39) Jen's okay all the time.
Scott Benner (27:41) Does she have any health issues?
Jen (27:43) She's the one that has the, gluten intolerance, but that's it.
Scott Benner (27:47) Do you ever do you let her talk about that with you? (27:49) Like, if she starts complaining about that, do you go, oh, come on. (27:51) Your stomach just hurts, do you
Jen (27:53) Of course, I listen to her. (27:54) Yes. (27:55) I listen. (27:55) I I give what I wanna receive. (27:57) So yes.
Jen (27:58) And I listen to her recipes that she bakes and all the things, and I try her stuff and say, wow. (28:03) Can't even tell it's gluten free. (28:05) Yes. (28:06) Mhmm. (28:06) Very, very, very supportive.
Jen (28:08) And I'll talk to her about, wow. (28:09) It must be hard when you travel, if it's just salads or you know, like, I try to I do. (28:14) I just try to do do that. (28:16) And you're right. (28:16) I could literally just say to my family, hey, guys.
Jen (28:21) Every once in a while, if you wanna ask about my diabetes, that would be great with me. (28:26) You know, I I guess I could say that. (28:28) I feel like that is so vulnerable for me to do, but I feel like I could and see I think I'm so afraid to do it.
Scott Benner (28:35) What do you think could go wrong?
Jen (28:37) Well, they could just be the same and just go, what?
Scott Benner (28:40) Just go, I'm not I'm not interested. (28:42) I won't be asking you. (28:44) Yeah.
Jen (28:44) I'm just not gonna ask you. (28:45) Then I'm really good at them for sure. (28:47) They don't care. (28:48) So right now, I can still pretend that they I know they care. (28:51) I don't know how to explain it, but I just like, when you like, when I hear the parents talk about staying up all night and checking their kids' blood sugar and looking at their sugars all day.
Jen (29:03) I'm like, if I had someone doing that for me, OMG. (29:06) That would be amazing.
Scott Benner (29:08) Well And And if that was happening for you from the beginning, you wouldn't know, and then you would just take it for granted. (29:12) I know.
Jen (29:13) I know. (29:14) Yeah. (29:14) But I'm just saying, it just I've had it one time. (29:16) I played pickleball, and I was in a pickleball tournament. (29:19) And my wife said, I'm gonna give me your phone.
Jen (29:22) I'm gonna handle your diabetes. (29:23) And I went, oh my god. (29:25) That would be amazing. (29:26) And it was the most amazing thing. (29:28) She'd come over, take two sips of this, or, hey.
Jen (29:30) You need this much insulin. (29:31) And I was I was like, this is so wonderful.
Scott Benner (29:34) You're like a fighter. (29:35) Every every couple of minutes you head into the corner and somebody just wets you down and squirts something in your mouth, and, like, go go and go do it again.
Jen (29:42) I was like, yeah. (29:43) I got this. (29:43) Yeah. (29:44) So totally. (29:44) I felt like rocky.
Jen (29:45) I was like, yeah. (29:46) It's dope. (29:47) But, yeah, it was so nice to have that.
Scott Benner (29:49) I bet.
Jen (29:50) So, anyway, I'm not trying to complain about it. (29:52) I'm just saying I think as adults who get diagnosed are sometimes the forgotten ones by the medical community because we are adults.
Scott Benner (30:02) But maybe by everybody else too.
Jen (30:05) Yeah. (30:05) By everybody Right. (30:07) For me. (30:07) Yeah. (30:07) So, anyway, that's
Scott Benner (30:09) No. (30:09) That's interesting. (30:09) It really is. (30:10) And I mean, you've and you've listen. (30:11) You're talking about this to it's not like it happened to you yesterday.
Scott Benner (30:14) You're twenty three years removed from being diagnosed, and it's still it's still impactful for you.
Jen (30:19) I know. (30:20) That
Scott Benner (30:21) Do you think that you could let it go if something happened? (30:26) Like, what if I snuck over to your mom and I was like, yo. (30:28) Call Jen and ask her about her diabetes. (30:30) And, like and and she did it. (30:32) Do you think you'd just be like, okay.
Scott Benner (30:34) Well, that part's over now and you'd move on? (30:36) Are you stuck in a spot? (30:38) Like, can you give it away even though they're not helping you take it away? (30:42) Does that make sense?
Jen (30:43) I'm gonna have to let it go if that is answering your question. (30:46) I know that I can't Yeah. (30:48) Convince them or make them do something that they don't wanna do. (30:52) And I know that they love me even though they don't ask about it. (30:55) You know, like, it's that weird dynamic.
Jen (30:58) I know. (30:59) And I guess I just wanted to share that when I have a bad day emotionally, it has a lot to do with that. (31:07) You know, just this having to deal with something nonstop Mhmm. (31:11) And people not ever asking about it. (31:15) Sometimes it's just hard.
Scott Benner (31:16) How long how long have you been married?
Jen (31:18) We've been married for eleven years.
Scott Benner (31:20) K. (31:20) So do you get any of that from her on the diabetes?
Jen (31:24) I do. (31:25) I yeah. (31:25) Oh, yeah. (31:26) Yeah. (31:26) She's definitely more supportive.
Jen (31:28) But what's funny and she told me not to tell you, but I'm gonna tell you anyway, is when we met, she she's still a physician assistant. (31:35) She's still a PA. (31:36) She worked in the ER when I met her. (31:38) And so I assumed she knew everything about type one. (31:42) And I'm showing her my Medtronic, whatever I had, you know, And and and she was clueless.
Jen (31:48) She had she knew nothing. (31:50) And now I know they don't know a whole lot about it, but she was so clueless. (31:54) And I had I've I felt a little resentful, like, I'm having to teach you, like, carbs and fats and proteins and all the things, and she didn't know. (32:03) And and so now, I mean, almost once a week, she'll say, wish I could take this from you. (32:08) You know?
Jen (32:09) And I'm like, no. (32:10) You're ADHD. (32:10) This would be worse if you had this. (32:12) But I'm like, don't take it from me. (32:13) But, you know, it's yeah, she definitely is very supportive.
Jen (32:17) But like we were saying before we started recording, she she just started I've always wanted her to listen to this podcast and just have a little bit better understanding. (32:27) Because every once in while, she'll give a, like, hey, babe. (32:29) Do you need to da da da? (32:31) I'm like, no. (32:32) You know, that's not what I need.
Jen (32:33) Right. (32:33) That's backwards.
Scott Benner (32:34) You know?
Jen (32:35) Oh my god. (32:35) And so I get frustrated with her. (32:37) And so she knew I was gonna be on this today speaking with you. (32:42) And so she's been listening to the podcast. (32:44) You know?
Jen (32:44) She's like, tell him I'm not a podcaster, but I've been listening for, like, the last week. (32:48) And I was like, okay. (32:49) I'll tell him.
Scott Benner (32:50) Well, because of that, because she's trying, I won't ask if you met at softball.
Jen (32:54) We did not. (32:55) You little booger. (32:56) We did listen. (32:57) We both played softball in high school, but no.
Scott Benner (32:59) I know you did, but that's not my point. (33:01) Of course. (33:02) Right?
Jen (33:03) I love to generalize too. (33:05) No. (33:05) We met in choir,
Scott Benner (33:07) and Uh-huh.
Jen (33:08) That's where we met. (33:09) Isn't that cute? (33:09) Yeah. (33:09) Was, like, community choir, and that's where we met. (33:12) So
Scott Benner (33:12) Oh, that's really lovely. (33:13) You're just out trying to meet people and have a good time, and you met each other.
Jen (33:16) Totally. (33:17) I was. (33:17) Yeah. (33:18) I was just I'm not really a great singer, but I grew up in choir. (33:20) So I was like, yeah.
Jen (33:21) I'll go join a choir. (33:22) I need to get out. (33:23) And she's actually really good. (33:24) She was like a voice major in college. (33:26) And before she switched to medicine, and so I told the director because I was overwhelmed, I said, I need to sit beside a strong alto.
Jen (33:34) Do you have anybody? (33:36) And he went, I do. (33:37) And her name's Jen as well. (33:38) So that's funny. (33:39) She's like he's like, yeah.
Jen (33:40) Jen. (33:40) And I'm like, okay. (33:42) And and so we sat I mean, like, the next day or whatever, next week, she sat beside me, and we I was like, oh my gosh. (33:50) She can sing. (33:51) And if I if you can sing beside me, I can match it.
Jen (33:54) You know, I can't really read the music, but I can hear it and match it. (33:57) And we had so much fun. (33:58) I'm like, oh my god. (33:58) This is so cool. (34:00) That's awesome.
Jen (34:00) And that's kinda how it started.
Scott Benner (34:02) That's nice.
Jen (34:02) Do you
Scott Benner (34:02) think that person was setting you up, or do you think they actually thought they they could cover your voice for you?
Jen (34:07) I think it was a little bit of both because he kinda raised his eyebrows like, oh, you could sit beside Jen. (34:12) Like that, I'm thinking, what's Jen? (34:14) You know? (34:14) But, anyway yeah. (34:16) Yeah.
Jen (34:17) Yep. (34:17) Yep.
Scott Benner (34:17) People love matchmaking. (34:18) They love it.
Jen (34:19) I know. (34:20) I do. (34:20) I know they do.
Scott Benner (34:21) Yeah. (34:21) Yeah. (34:22) Yeah.
Jen (34:22) Like But, you know, you haven't asked me, and I have written it down
Scott Benner (34:26) What?
Jen (34:26) About does anybody have autoimmune in your family?
Scott Benner (34:29) I mean, I'm waiting for it, but I also wanna ask about the Afrezza, but let let's do that thing first.
Jen (34:34) There's a lot to talk about, Scott. (34:35) You know, my my goal is to have a part one and part two, just so you know. (34:39) I told Kelly, if I get a part two, I've made it.
Scott Benner (34:43) Rob right now is like, listen. (34:44) It's the beginning of the year. (34:45) Just stop talking around an hour. (34:47) Would you please?
Jen (34:49) Don't make me work more. (34:50) I'm kidding. (34:50) You you yeah.
Scott Benner (34:51) I'll Well, no. (34:52) And you said your sister had celiac, so I was gonna get around to, like, ask him what else was going on.
Jen (34:57) Yes. (34:57) Well, yeah, sooner talk about that, and then we'll do Afrezza. (35:00) So so I didn't know any of this when I was diagnosed. (35:04) Obviously, I was clueless about type one or diabetes or autoimmune. (35:09) But listen to your podcast and and learning about that, I'm like, oh, yeah.
Jen (35:13) So I did ask my mom, and she's like, oh, yeah. (35:15) We had we I have or had two great aunts who had MS and then another great aunt who had type one, but she got it late in life. (35:25) Like, she was, like, 50 or 60 when she got that. (35:28) And then on my dad's side, RA, my dad has rheumatoid arthritis. (35:34) His mom had it, and his sister has it.
Jen (35:37) And then I have three second cousins once removed who have type one diabetes, all on my dad's side. (35:45) And they're all female, and they're all firstborn.
Scott Benner (35:48) Wait. (35:48) Wait. (35:48) There's type one on your mom and your dad's side?
Jen (35:51) Yeah. (35:52) Ain't that crazy?
Scott Benner (35:53) Yeah. (35:53) It's crazy that only you got it.
Jen (35:55) It's crazy that only know. (35:56) I keep I know. (35:58) A really bad part of me it's such a bad part of me. (36:01) Mhmm. (36:01) Wishes my one of my sisters would get it for, like, just for no.
Jen (36:05) Listen.
Scott Benner (36:05) Listen. (36:06) Just
Jen (36:06) for a week. (36:07) No. (36:07) Listen. (36:07) Just for a week.
Scott Benner (36:08) Okay.
Jen (36:08) Just for a week, and then they'd have some empathy, and then they'd take it away again. (36:12) That is a really horrible part of me, but just to have some empathy. (36:16) But
Scott Benner (36:16) What
Jen (36:16) They're not. (36:17) They're they're fine. (36:18) But I did wanna ask you
Scott Benner (36:19) Hold hold on. (36:19) Wait. (36:20) Wait. (36:20) Give me one second. (36:21) Give me one second.
Scott Benner (36:22) Yeah. (36:22) Hold that thought. (36:24) Okay. (36:24) What if instead of wishing that they could have diabetes for a week, what if you did day of diabetes with them? (36:30) What if you said to them, I really wish you understood this more.
Scott Benner (36:34) I know that sometimes you feel like I might be complaining, and that breaks my heart because I just I need somebody to talk to about it. (36:40) I don't have anybody to understand. (36:42) I was wondering if you could spend twenty four hours understanding better what diabetes is. (36:48) Like, what if I texted you every time I had to think about diabetes for one day?
Jen (36:55) Oh my gosh. (36:55) Okay. (36:56) Yeah. (36:56) I could do that.
Scott Benner (36:57) See, and I explained to you, like, hey. (36:58) Right now, I'm, you know, counting carbs up for a meal that I'm gonna eat twenty minutes from now. (37:04) Or I just changed my pod. (37:06) It took fifteen minutes. (37:09) You know, I had to like, here's what I did.
Scott Benner (37:12) I stopped what I was doing. (37:13) I was in the middle of working. (37:14) I stopped what I was doing. (37:15) I went to the refrigerator. (37:15) I got my insulin.
Scott Benner (37:16) I got the pump out. (37:17) I opened up the pump. (37:18) I put the needle together. (37:19) The needle, you know, drew out the insulin. (37:22) I tapped the bubbles out of it, filled the pod, primed the pod, you know, put it on, inserted it.
Scott Benner (37:28) I looked to see that, oh gosh, you know, my blood sugar is already one thirty. (37:31) The new pod is probably gonna go up. (37:33) Do I need the bolus right now? (37:34) How much? (37:34) I don't wanna get low.
Scott Benner (37:35) I have to go back to like, like, what if you like, what if they had that information?
Jen (37:40) Mhmm.
Scott Benner (37:40) And, like, just for the maybe you'd even write it down, not and and share it with them later instead of the, you know, texting it to them. (37:47) But just so you could just say to them, like, I would love for you to understand what it's like. (37:52) I don't want you to feel bad. (37:53) I'm not looking for Mhmm. (37:54) Sympathy.
Scott Benner (37:55) I can't really explain it to you, but there are times that I feel strong and that I don't want anybody to worry about me, but there are other times I wish someone understood what I was going through. (38:08) Don't you know what it's like to wish somebody understood what you were going through? (38:11) And then please tell me what's in your life that I don't understand that I could understand better. (38:17) Like, it might be an it might be a nice bonding thing for your sisters. (38:20) You know?
Jen (38:21) I know. (38:21) That sounds really nice.
Scott Benner (38:22) Don't do your mom.
Jen (38:23) Put it that way.
Scott Benner (38:24) She little
Jen (38:24) Oh, definitely not doing my mom. (38:25) Yeah. (38:25) Yeah.
Scott Benner (38:26) Yeah. (38:26) Yeah. (38:26) That that's that's that's different. (38:28) Just Yeah. (38:28) Yeah.
Scott Benner (38:29) Yeah. (38:29) She gets the coast to the end now. (38:31) Exactly.
Jen (38:33) Yeah. (38:33) We'll give her a pass.
Scott Benner (38:34) Yeah. (38:34) I remember the time I looked at my mom, and I said to my brother, it's like, it's time to stop teaching mom things. (38:39) Let's just let her go. (38:41) Whatever she thinks Exactly. (38:42) Is good enough.
Scott Benner (38:43) Like, don't let her be. (38:44) But
Jen (38:45) Oh, no.
Scott Benner (38:45) I don't know. (38:46) Like, does that sound crazy?
Jen (38:48) No. (38:48) It does not sound crazy.
Scott Benner (38:49) Interesting. (38:50) I wonder if you'll
Jen (38:50) do it. (38:50) Really helpful. (38:51) I knew you'd help me with this. (38:53) I was like, he's gonna help you.
Scott Benner (38:54) I mean, I'm pretty thoughtful.
Jen (38:55) You're very thoughtful. (38:56) You could have been a therapist for sure.
Scott Benner (38:58) Did you hear that cutting edge breakdown of did you meet in softball? (39:01) It's amazing.
Jen (39:04) I love it.
Scott Benner (39:07) So okay. (39:07) So I'm sorry. (39:08) I cut you off. (39:09) What were you gonna say?
Jen (39:10) I don't remember.
Scott Benner (39:11) I do you have ADHD?
Jen (39:13) I don't dude. (39:14) No.
Scott Benner (39:15) You jump around a little bit, so I stopped you to see if you'd remember what you were gonna say.
Jen (39:19) You are a booger. (39:20) No. (39:20) I don't have ADHD.
Scott Benner (39:22) Okay.
Jen (39:23) I don't. (39:24) I just have a long story. (39:25) Did you I've lived a long life.
Scott Benner (39:27) Did you think I was disagreeing with you when I said okay? (39:31) You're like, I don't.
Jen (39:33) Yeah. (39:33) Like, I'm feeling offended. (39:35) I'm I'm okay. (39:36) Your,
Scott Benner (39:38) spouse does. (39:39) Your wife does.
Jen (39:40) Yes. (39:41) She does.
Scott Benner (39:41) Is that a diagnosed thing, or is it just a thing she says?
Jen (39:45) No. (39:45) It's for sure diagnosed and treated.
Scott Benner (39:47) Because the because the whole world's running around saying they have ADHD. (39:50) Don't know if you noticed too. (39:51) People like to say they're autistic now too. (39:53) I know. (39:54) I know.
Jen (39:54) Yeah. (39:54) They're on the spectrum.
Scott Benner (39:55) I don't think you are. (39:56) I I I and I think people with autism would be offended if they heard you.
Jen (40:01) Right. (40:01) Yeah. (40:02) For sure. (40:02) But no. (40:03) No.
Jen (40:03) She definitely has all the the symptoms, signs, unfortunate parts of ADHD.
Scott Benner (40:10) Okay.
Jen (40:10) So yeah. (40:12) Yep.
Scott Benner (40:12) What are the unfortunate parts?
Jen (40:14) Oh, well, she is very, very hard on herself. (40:20) She always has no time, so she's always behind. (40:25) She is, like, hard for her to finish things. (40:28) So, like, just some like, a funny example, we get Amazon packages and show up in the package, but do you think she puts the package you know, like, there's the box is there, and I've I've, you know, I've it up, and I put it in the recycling. (40:41) You know, like, she those little things, it's not a big deal, but that'll happen.
Jen (40:44) But her biggest thing is, like like I said, she's a PA, and she's really good with her patients. (40:50) She's so good and empathetic and really good provider, but that's not what the medical industry wants. (40:56) Right? (40:56) They want you to be quick and hurry. (40:59) So she gets kinda penalized for being slow.
Scott Benner (41:03) Stop the right word. (41:04) People and
Jen (41:05) Yeah. (41:05) Yeah. (41:05) Yeah. (41:06) And I do again, I've already said this. (41:08) I know my part.
Jen (41:08) I'm responsible. (41:09) I've always been that way. (41:11) And so I have to be really careful to not manage her, to not mother her. (41:16) You know, like, it's that dynamic that can happen in that relationship.
Scott Benner (41:20) Mhmm.
Jen (41:21) Because it it but there'll be times where I'll be like, Okay. (41:24) Because she'll be like, hey. (41:26) You know, I think we should paint the garage, and and then we're gonna, you know, clean it out, and then we're gonna da da da da. (41:33) I'm like, no. (41:33) No.
Jen (41:33) No. (41:33) No. (41:34) No. (41:34) You know, we're gonna do this one thing.
Scott Benner (41:36) Go throw the box away. (41:38) Let's see you throw a box away before I paint something.
Jen (41:40) Box away before we clean out the whole garage. (41:42) And so I'm there to help kinda help to prioritize and to
Scott Benner (41:48) Mhmm.
Jen (41:49) Put things in a certain you know, the the the first step is this and now this and that because she will start spiraling is what they call it. (41:55) And she's spiraling very emotional, very reactive. (41:59) And so and so, like, if I'm, like, if I'm low, you know, and I'm like, oh, I gotta you know? (42:04) And and she'll kinda pick up on my crazy frantic energy if it's a bad low, like I'm dropping quick. (42:12) And she's there to help me, but I'm like, I need you to be calm.
Jen (42:16) You know what mean? (42:16) Like, I don't need you to get up, you know, emotional with me. (42:20) That doesn't make me feel better. (42:21) So Yeah. (42:22) That's kinda what so there's a lot of good about ADHD, but in her profession, it's hard to be ADHD in the medical field Okay.
Jen (42:30) From what I've seen.
Scott Benner (42:31) Yep. (42:31) So I'm looking at your notes for the first time.
Jen (42:34) Oh, yeah. (42:34) Do you
Scott Benner (42:35) think coming out how wait. (42:37) I don't understand what you're saying here.
Jen (42:39) Do you think Okay. (42:39) Okay. (42:39) Okay.
Scott Benner (42:39) Go ahead.
Jen (42:40) So when I was first diagnosed, you know, they always said they would say, did you have the flu? (42:44) Did you have mono? (42:45) Were you sick?
Scott Benner (42:46) Anything stressful.
Jen (42:47) Prior, and I wasn't. (42:49) And the only thing I had was, yeah, the only thing I had was those seasonal allergies. (42:53) Right? (42:53) And I'm like, well, I have allergies, but that's it. (42:55) It's only the thing I go to the doctor for.
Jen (42:57) And so as within that first year of diagnosis, I was doing a lot of self reflection because a part of me is like, did I cause this? (43:04) Before I understood diabetes, you know, and type one. (43:07) And and I was I was like because stress well, oh, I know what I was stressed about.
Scott Benner (43:12) Yeah.
Jen (43:12) I was I didn't honestly didn't know I was attracted to women in my late twenties. (43:19) And I remember in that you know, the year before diagnosis, I had a so called best friend, and she was. (43:25) We're just best friend, platonic, no big deal. (43:27) But between you and me and a lot of people, I, you know, I had I was like, I really, really like her. (43:35) You know?
Jen (43:36) Like, it's like, I just like to be around her. (43:38) I like to you know, I just wanna talk to her all the time. (43:40) That was it. (43:41) Nothing physical. (43:43) It was just more like this emotional thing.
Jen (43:46) And then she so called broke up with me, and we stopped being friends. (43:50) And it was like a real breakup. (43:51) And I'm like, what is wrong with me? (43:54) Why does this feel like a real breakup? (43:55) Because at the time I was dating men, I've been engaged to men, you know, the whole thing.
Jen (44:00) And so it was such a stressful event that I have no idea if that is what triggered me to finally turn this gene on and, you know, get type one, but there was nothing else really going on in my life. (44:14) You know what I mean?
Scott Benner (44:15) How long? (44:17) My gosh. (44:18) So you so you dated men for the fur like, maybe you still do. (44:22) I have no idea what you do. (44:23) But, like No.
Jen (44:23) I don't. (44:24) I don't. (44:24) Don't. (44:24) But yeah. (44:24) So I yeah.
Jen (44:25) So, like, I remember I mean, in high school, I was, you know, I was athletic. (44:30) I played sports. (44:31) I had made good grades. (44:32) I was a good kid kind of thing. (44:33) Mhmm.
Jen (44:34) And I was like, well, I should be interested in boys so I have something to talk to my girlfriends about. (44:39) You know? (44:40) Like like, that's what they do, so I guess I should like boys too. (44:43) But I didn't know that that was weird or different. (44:45) Now, you know, I was like, I guess I should like boys.
Jen (44:48) And they kinda got on my nerves, but I'm athletic, so we'd pass softball or football. (44:52) And, yeah, we'd play sports, and I liked that part of it. (44:56) But I didn't like the other part of of dating. (45:00) And so but I didn't think much about it. (45:03) And but, yeah, I mean, if you guys wanna know how to get a ring on your finger, I can definitely teach you how to get a ring on your finger.
Jen (45:11) It's basically don't care about the guy, don't wanna see him for a week or two, don't have sex with him, and he wants to marry you. (45:19) So Treat
Scott Benner (45:20) boys poorly and they chase you around?
Jen (45:22) And I me I'm not trying to sound horrible, but I just wasn't that interested in them. (45:26) You know? (45:27) And I didn't understand that I wasn't. (45:29) Yeah. (45:30) And I remember when I came out, finally, my sister Jill, she said, oh my god.
Jen (45:35) I'm so glad you're gay because I thought there was something wrong with me that I like boys so much. (45:40) We So anyway.
Scott Benner (45:41) We we we did you did you did you do the have you done the deed with the boys? (45:56) This episode was too good to cut anything out of, but too long to make just one episode. (46:01) So this is part one. (46:02) Make sure you go find part two right now. (46:04) It's gonna be the next episode in your feet.
Scott Benner (46:09) US Med sponsored this episode of the Juice Box podcast. (46:13) Check them out at usmed.com/juicebox or by calling (888) 721-1514. (46:21) Get your free benefits check, and get started today with US Med. (46:27) The podcast is also sponsored today by Omnipod five. (46:31) Omnipod five is a tube free automated insulin delivery system that's been shown to significantly improve a one c and time and range for people with type one diabetes when they've switched from daily injections.
Scott Benner (46:42) Learn more and get started today at omnipod.com/juicebox. (46:46) At my link, you can get a free starter kit right now. (46:49) Terms and conditions apply. (46:50) Eligibility may vary. (46:52) Full terms and conditions can be found at omnipod.com/juicebox.
Scott Benner (46:58) Thank you so much for listening. (47:00) I'll be back very soon with another episode of the juice box podcast. (47:03) If you're not already subscribed or following the podcast in your favorite audio app, like Spotify or Apple Podcasts, please do that now. (47:11) Seriously, just to hit follow or subscribe will really help the show. (47:16) If you go a little further in Apple Podcasts and set it up so that it downloads all new episodes, I'll be your best friend.
Scott Benner (47:22) And if you leave a five star review, oh, I'll probably send you a Christmas card. (47:27) Would you like a Christmas card? (47:34) If you're looking for community around type one diabetes, check out the Juice Box Podcast private Facebook group. (47:41) Juice Box Podcast, type one diabetes. (47:44) But everybody is welcome.
Scott Benner (47:45) Type one, type two, gestational, loved ones, it doesn't matter to me. (47:50) If you're impacted by diabetes and you're looking for support, comfort, or community, check out Juice Box podcast, type one diabetes on Facebook. (48:00) If you'd like to hear about diabetes management in easy to take in bits, check out the small sips. (48:06) That's the series on the Juice Box podcast that listeners are talking about like it's a cheat code. (48:11) These are perfect little bursts of clarity, one person said.
Scott Benner (48:14) I finally understood things I've heard a 100 times. (48:18) Short, simple, and somehow exactly what I needed. (48:20) People say small sips feels like someone pulling up a chair, sliding a cup across the table, and giving you one clean idea at a time. (48:29) Nothing overwhelming, no fire hose of information, just steady helpful nudges that actually stick. (48:34) People listen in their car, on walks, or rather actually bolus ing anytime that they need a quick shot of perspective.
Scott Benner (48:41) And the reviews, they all say the same thing. (48:44) Small sips makes diabetes make sense. (48:47) Search for the Juice Box podcast, small sips, wherever you get audio. (48:52) If you have a podcast and you need a fantastic editor, you want Rob from Wrong Way Recording. (48:58) Listen.
Scott Benner (48:59) Truth be told, I'm, like, 20% smarter when Rob edits me. (49:03) He takes out all the, like, gaps of time and when I go, and stuff like that. (49:08) And it just I don't know, man. (49:10) Like, I listen back and I'm like, why do I sound smarter? (49:12) And then I remember because I did one smart thing.
Scott Benner (49:15) I hired Rob at wrongwayrecording.com.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#1781 Body Grief: Hopelessness, Hope & Self Care
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
We continue through the Body Grief process with two deeply connected stages: Hopelessness and Hope, and how they eventually open the door to Body Trust.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner (0:0) Here we are back together again, friends, for another episode of the Juice Box podcast. (0:15) Body grief is the sense of loss and mourning that comes with living in an ever changing body. (0:21) And in this new series with myself and Erica Forsyth, we're gonna talk all about it. (0:27) How would you like to share a type one diabetes getaway like no other? (0:31) Join me on Juice Cruise 2026.
Scott Benner (0:33) You may be asking, what is Juice Cruise? (0:35) It's a week long cruise designed specifically for people and families living with type one diabetes. (0:40) It's not just a vacation. (0:42) It's a chance to relax, connect, and feel understood in a way that is hard to find elsewhere. (0:47) We're gonna sail out of Miami, and the cruise includes stops in CocoCay, San Juan, Saint Kitts, Nevis aboard the stunning Celebrity Beyond.
Scott Benner (0:57) This ship is chosen for its comfort, accessibility, and exceptional amenities. (1:02) You're gonna enjoy a welcoming environment surrounded by others who get life with type one diabetes. (1:08) I'm gonna host diabetes focused conversations and meetups on the days at sea. (1:12) There's thoughtfully designed spaces, incredible dining, and modern amenities all throughout the celebrity beyond. (1:20) Your kids can be supervised, and there's teen programs so everyone gets time to recharge.
Scott Benner (1:26) Not just the the kids going on vacation, but maybe you get the kickback a little bit too. (1:30) There's gonna be zero judgment, real connections, and a whole lot of sun and fun on Juice Cruise twenty twenty six. (1:36) Please come with me. (1:37) You're going to have a terrific time. (1:39) You can learn more or set up your deposit at juiceboxpodcast.com/juicecruise.
Scott Benner (1:45) Get ahold of Suzanne at cruise planners. (1:47) She will take care of everything. (1:49) Link's in the show notes. (1:50) Link's at juice box podcast dot com. (1:53) I created the diabetes variable series because I know that in type one diabetes management, the little things aren't that little, and they really add up.
Scott Benner (2:02) In this series, we'll break down everyday factors like stress, sleep, exercise, and those other variables that impact your day more than you might think. (2:10) Jenny Smith and I are gonna get straight to the point with practical advice that you can trust. (2:15) So check out the diabetes variable series in your podcast player or at juiceboxpodcast.com. (2:21) Nothing you hear on the juice box podcast should be considered advice, medical or otherwise. (2:26) Always consult a physician before making any changes to your health care plan.
Scott Benner (2:33) The episode you're about to listen to was sponsored by Touched by Type one. (2:38) Go check them out right now on Facebook, Instagram, and, of course, at touchedbytype1.org. (2:44) Check out that programs tab when you get to the website to see all the great things that they're doing for people living with type one diabetes. (2:52) Touched by type1.org. (2:54) Today's episode is also sponsored by Eversense three sixty five, the only one year wear CGM.
Scott Benner (3:02) That's one insertion and one CGM a year. (3:05) One CGM, one year. (3:08) Not every ten or fourteen days. (3:10) Ever since cgm.com/juicebox. (3:14) The podcast is also sponsored today by the Tandem MOBI system, which is powered by Tandem's newest algorithm, Control IQ Plus technology.
Scott Benner (3:23) Tandem MOBI has a predictive algorithm that helps prevent highs and lows and is now available for ages two and up. (3:29) Learn more and get started today at tandemdiabetes.com/juicebox. (3:35) Erica, I appreciate you coming back. (3:36) We were gonna try to finish up the body grief series today. (3:39) Is that right?
Erika Forsyth (3:40) That's the plan. (3:42) Yes.
Scott Benner (3:42) Look at us. (3:45) How do you wanna handle this? (3:46) Do wanna do you wanna just give a little overview of what you think what got us to this point and then how we're gonna finish up, or do you just wanna jump in? (3:55) What do you think?
Erika Forsyth (3:56) I think let's do a quick recap in light of this perhaps being our final episode of the series.
Scott Benner (4:03) Okay.
Erika Forsyth (4:03) So we we're kind of reviewing the body grief stages, and this these are as defined by Jane Mattingly from her book. (4:12) This is body grief. (4:13) And body grief is, you know, the experience or, the sense of loss or mourning that comes with living in a body. (4:21) Right? (4:21) So the having that feeling that you wish you could go back to the way your body used to function, the way your body used to look, and the sense of loss that accompanies that that longing.
Erika Forsyth (4:33) And so the stages that she defines, there are seven of them, and so far, we've reviewed five or discussed five. (4:41) The first one's dismissal, which sounds like, I'm fine. (4:45) Everything's fine. (4:46) The second one is shock, though that might sound like you're feeling overwhelmed and feeling like you just can't keep going. (4:54) You can't function.
Erika Forsyth (4:56) Apology is the third stage. (4:59) It's kind of sounding like I'm I'm sorry for being me. (5:02) I'm sorry for the way I'm presenting. (5:04) I'm sorry for my illness. (5:05) The fourth stage is fault, and that sounds like why me?
Erika Forsyth (5:10) Why did this happen? (5:12) Could I done anything differently? (5:14) And the fifth stage is fight, which sounds like I'm gonna beat this thing. (5:20) And so we've discussed all of those in previous episodes. (5:24) And so today, I thought we could discuss the stage six, which is combined hopelessness and hope together.
Erika Forsyth (5:32) And then the the final stage, is body trust, which ultimately, we're discussing it as the final stage and even naming it as such, but, really, it's something that we want to practice and integrate as you work through the different stages.
Scott Benner (5:46) Okay.
Erika Forsyth (5:46) So how does that sound?
Scott Benner (5:47) I'm incredibly interested. (5:49) I have, enjoyed this conversation a lot so far and have seen a number of comments online recently about how people feel just about you being on the podcast in general and and how valuable they find these conversations. (6:02) So, honestly, I'm excited to finish this one up and then figure out what we're gonna talk about next.
Erika Forsyth (6:07) Yes. (6:07) Yes. (6:08) Great. (6:08) Well, thank you. (6:09) I appreciate that.
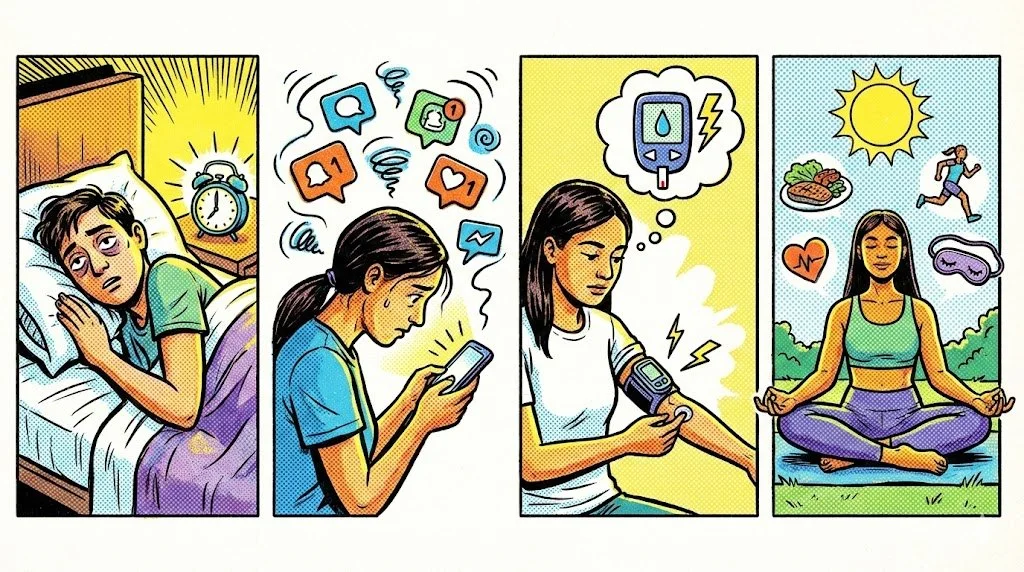
Erika Forsyth (6:10) So so the stage six, hopelessness and hope. (6:13) So, again, these are these are tool these are definitions and tools that Jane, the author, uses, and then we're trying to kind of apply them and discuss them through the lens of living with diabetes. (6:22) Mhmm. (6:23) So when when you're in hopelessness, this one is probably very clear and obvious. (6:28) It sounds like, you know, what is the point of all this?
Erika Forsyth (6:31) You're feeling devastated. (6:34) It's also a very natural place to be. (6:35) We all experience hopelessness at some point. (6:39) It often feels like it hits when there's just no way out. (6:42) Like, you can't excuse yourself.
Erika Forsyth (6:44) You can't dismiss it. (6:46) You are out of kind of the the wimey stage, and you're that might even lead to that feeling of hopelessness. (6:52) You might be feeling like you are forgotten. (6:55) Right? (6:56) Like, you get you get diagnosed or you go through and do challenge within your life with diabetes, and people are are still living their lives.
Erika Forsyth (7:04) And you might feel like you're gonna be left behind. (7:07) If you are in hopelessness, this might feel or sound a little bit like, you know, depression that you're feeling really lethargic. (7:16) You have really intense fatigue. (7:18) You might be sleeping more. (7:20) You are canceling plans.
Erika Forsyth (7:22) And then that isolation as a result of those other feelings and behaviors, that can lead to even more thoughts of just a feeling left behind, a feeling stuck, a feeling like no one really understands what what you're going through. (7:37) And then, ultimately, you stop using the coping skills, right, that you know would help you Right. (7:42) Kind of move out of this space, but you you feel like you just can't.
Scott Benner (7:46) That feels that's maybe the part where you give in and just throw in the towel.
Erika Forsyth (7:51) Yes. (7:51) Yes.
Scott Benner (7:52) So in the beginning, you experienced some sort of a change in your body's ability to do what you expect to do, and you can feel like, okay. (8:04) This this vessel is not doing what was promised here. (8:08) Mhmm. (8:08) And then it this drift, if you're not supporting yourself correctly, this drift can get worse and worse and worse until you finally just throw in the towel and you go, oh, I I I give up. (8:17) Like, I'm gonna I'm gonna feel like this forever.
Scott Benner (8:20) I have a failed body. (8:21) It's not gonna do what I need to do instead of reframing. (8:24) Because I don't find that to be I'm not saying everybody's situation is exactly the same, but for the most part, type one diabetes is not gonna leave you in a situation where your body can't keep up with your activities and your the other things you wanna do. (8:37) There's obviously more steps to take sometimes, and some people have greater struggles than others. (8:42) But I have also seen people who I think are just bowled over by this thing, which I would have probably called depression at first.
Scott Benner (8:50) But now that you've outlined it like this, it really does feel more focused on on this this letdown that you've experienced.
Erika Forsyth (8:57) And and they can they can commingle. (9:00) Right? (9:00) I mean, hopelessness is a a symptom of depression.
Scott Benner (9:04) Mhmm.
Erika Forsyth (9:04) So and and, also, this might sound like burnout. (9:08) Right? (9:09) Like, you might get to this place where you just feel like you can't keep doing what you need to do to take care of yourself. (9:16) And, yes, this might you might experience it's really normal to experience feeling of hopelessness, whether it's with diabetes or any other change in your body. (9:25) Like, even if we were to simplify it with a cold and you had all these plans and then you had to cancel them.
Erika Forsyth (9:33) And when you have that letdown, right, when you feel like you just you can't do anything and your body is is shifting and you're like, gosh. (9:41) Why couldn't it be like it was yesterday?
Scott Benner (9:43) Right.
Erika Forsyth (9:43) So it can be very small, this feeling of hopelessness, but also can be become bigger given many different factors. (9:53) But I think just naming it is really helpful too to notice, oh my gosh. (9:57) Okay. (9:57) I'm I'm having these thoughts and feelings. (9:59) I'm canceling plans.
Erika Forsyth (10:01) I'm feeling isolated. (10:02) I feel like no one really is getting this. (10:04) Oh, I'm I'm in this hopelessness stage. (10:07) And to name it and normalize it. (10:09) And then we're gonna talk about, you know, kind of the flip side of it, which is hope.
Scott Benner (10:13) I think that the thing that I like most about this conversation is that you can see that this exists outside of diabetes Mhmm. (10:21) Or outside of chronic illness at all. (10:23) Like, the people can experience this for, you know, I don't know, pain that won't go away or even a body style change. (10:30) I wouldn't call it body grief, but I've had trouble, like, adjusting to just not weighing as much. (10:36) It it it has been odd at times and and impactful.
Scott Benner (10:40) And so, like, understanding that this feeling can can come from a lot of different places, but that you might be experiencing it out there listening because of type one. (10:50) I find that just I don't know. (10:51) I find that distinction incredibly important. (10:54) Mhmm. (10:55) I I don't wanna
Erika Forsyth (10:55) stop you, but Yes. (10:56) And I think that's, you know, part of why I think this this book, a, I think, has has been successful to a lot of different types of people. (11:05) Right? (11:05) She's she's it is a universal experience of loss that we that we all have, whether it's with a chronic illness or a change in body style or body type or, yeah, the chronic pain that just won't go away. (11:19) Yeah.
Erika Forsyth (11:19) And I think having these and having terms helps us contain, oh, this is what's happening.
Scott Benner (11:27) Mhmm.
Erika Forsyth (11:27) This is what I'm experiencing and feeling less alone in it and less, hopefully, less stuck.
Scott Benner (11:31) It would have never occurred to me without this conversation that I had a preconceived expectation of the shell that I'm walking around in. (11:38) And that if it doesn't do the thing that I've come to expect it to do, that that could be a letdown in some way. (11:43) I never I genuinely never would have thought about it if it if it didn't, if it didn't come up like this. (11:47) So, anyway, I'm I'm grateful you brought this to me.
Erika Forsyth (11:50) It's good.
Scott Benner (11:50) Yeah. (11:51) But but go ahead and move on. (11:52) I I apologize
Erika Forsyth (11:52) for Okay.
Scott Benner (11:53) Cutting you off.
Erika Forsyth (11:54) So I think what I appreciate the way that she discusses the fact that hopelessness and hope can go hand in hand, that whenever we are experiencing hopelessness, we are able to kind of hold on. (12:12) Right? (12:12) And the okay. (12:14) Things have gotta change. (12:15) Things are gonna get better.
Erika Forsyth (12:16) And not in a kind of magical thinking kind of way, but trusting that things are gonna shift. (12:24) Now when we when it's hard to get to that space, that's when perhaps you might be experiencing more clinical levels of depression.
Scott Benner (12:31) Okay.
Erika Forsyth (12:33) So I don't wanna kind of say, just just think that things could change and things will get better, and it'll be fine because that's can be really hard to do Mhmm. (12:42) When you're in severe levels of depression. (12:45) She defines kind of hope that is this glue, right, that keeps the body grief process together. (12:51) And so how do you know if you're able to experience? (12:54) What are some signs that you're in hope?
Erika Forsyth (12:56) So it is allowing yourself to consider that things could possibly get better. (13:02) So I'm envisioning, like, you're you're in this position. (13:05) You're feeling like, first of all, how did I get here? (13:07) How did I get diabetes? (13:09) How am I ever going to feel better?
Erika Forsyth (13:11) How am I gonna cope? (13:12) Why did this happen to me? (13:14) I'm feeling so isolated and alone, and I'm not gonna reach out for help. (13:18) So I that was kinda I'm quickly moving through the stages. (13:21) If you are able to say, okay.
Erika Forsyth (13:22) Things are really hard right now, but I'm gonna allow myself the option to consider that things might get better. (13:30) Mhmm. (13:31) Not not that they will. (13:32) Not that, like, you're gonna click your heels or tomorrow's Monday, and it's gonna be great on Monday. (13:37) Everything's gonna reset, but just holding that hope.
Scott Benner (13:40) The it's a possibility. (13:41) Yeah. (13:44) This episode is sponsored by Tandem Diabetes Care. (13:47) And today, I'm gonna tell you about Tandem's newest pumping algorithm. (13:51) The Tandem Mobi system with Control IQ plus technology features auto bolus, which can cover missed meal boluses and help prevent hyperglycemia.
Scott Benner (14:00) It has a dedicated sleep activity setting and is controlled from your personal iPhone. (14:05) Tandem will help you to check your benefits today through my link, tandemdiabetes.com/juicebox. (14:12) This is going to help you to get started with Tandem's smallest pump yet that's powered by its best algorithm ever. (14:19) Control IQ Plus technology helps to keep blood sugars in range by predicting glucose levels thirty minutes ahead, and it adjusts insulin accordingly. (14:27) You can wear the Tandem Mobi in a number of ways.
Scott Benner (14:30) Wear it on body with a patch like adhesive sleeve that is sold separately, clip it discreetly to your clothing, or slip it into your pocket. (14:38) Head now to my link, tandemdiabetes.com/juicebox, to check out your benefits and get started today. (14:47) When you think of a CGM and all the good that it brings in your life, is the first thing you think about, I love that I have to change it all the time? (14:54) I love the warm up period every time I have to change it? (14:57) I love that when I bump into a door frame, sometimes it gets ripped off.
Scott Benner (15:01) I love that the adhesive kinda gets mushy sometimes when I sweat and falls No. (15:05) These are not the things that you love about a CGM. (15:09) Today's episode of the Juice Box podcast is sponsored by the Eversense three sixty five, the only CGM that you only have to put on once a year, and the only CGM that won't give you any of those problems. (15:21) The Eversense three sixty five is the only one year CGM designed to minimize device frustration. (15:28) It has exceptional accuracy for one year with almost no false alarms from compression lows while you're sleeping.
Scott Benner (15:34) You can manage your diabetes instead of your CGM with the Eversense three sixty five. (15:40) Learn more and get started today at eversensecgm.com/juicebox. (15:46) One year, one CGM.
Erika Forsyth (15:48) Yeah. (15:48) It's a possibility. (15:49) Okay. (15:50) So and that's what she calls practicing blind faith. (15:54) So we're not we're not out there kind of chasing the cure, which I know we so desperately want, and we can get kind of stuck in some of those traps.
Erika Forsyth (16:03) But it's about, she just says, trusting the present enough to wanna stick around for what the future holds. (16:10) I love I like that. (16:12) Even when even when you're in your a really moment full of despair and you're feeling really, you know, just crappy emotionally, maybe even physically, say, okay. (16:22) Things it will it will not stay this way forever.
Scott Benner (16:26) Okay. (16:27) Yeah.
Erika Forsyth (16:27) So if that's hard to envision, how can you cultivate more of that hope? (16:34) So here are some four four tools that I think are are pretty helpful, hopefully, will be helpful. (16:39) Asking yourself, k. (16:41) Who am I gonna be in the future? (16:43) Getting to know your future use.
Erika Forsyth (16:44) So this is if you're feeling really stuck and trapped. (16:47) Who am I gonna be in five minutes, in five days, in in one month, in six months? (16:54) Right? (16:54) Asking yourself, what have you been excited about recently? (16:59) What has been bringing you contentment?
Erika Forsyth (17:02) Do you feel supported right now, and who who is supporting you in the future? (17:07) What is bringing you joy? (17:08) So that is a mind exercise because even though you're feeling maybe hopeless right now, you're kind of getting yourself to the place of, like, things might get better because I'm I'm envisioning in five months from now, oh, this thing is bringing me joy, or this person is really supporting me right now. (17:27) Mhmm. (17:27) Does that make sense?
Scott Benner (17:28) Yeah. (17:29) And can it be small just, like, slam dunks that you know are gonna happen to you? (17:34) Like, can I be like, oh my god? (17:35) Stranger Things is coming out. (17:36) I'm gonna be excited when that happens, that kind of stuff.
Erika Forsyth (17:38) Yes.
Scott Benner (17:39) Sam?
Erika Forsyth (17:40) Yes. (17:40) Anchor. (17:41) Yes. (17:41) Anchoring onto something that you know will be exciting and perhaps fulfilling, and it could be very small or very big.
Scott Benner (17:48) Yeah. (17:48) So it's almost cheat. (17:49) Like, put something out in front of yourself like a goal that you know is definitely gonna happen. (17:52) Like, well, I'm I'm gonna be super excited when Wednesday gets here. (17:55) And then when Wednesday comes, be like, woo.
Scott Benner (17:56) We did it. (17:57) Right? (17:57) Yeah. (17:57) No. (17:58) It's just hey.
Scott Benner (17:58) Listen. (17:59) I do that with does everyone not do this? (18:01) Like, I think it keeps me alive to wanna see a movie that's coming out a year from now. (18:06) I always think like, oh, I just wanna watch that movie. (18:08) Then once I see it, I go, oh, I I wanna make it to next summer to see this one.
Scott Benner (18:11) I know that's got no real bearing on my my actual longevity, but I do think it has a bearing on I don't think it's debatable that human beings do better when they have tasks to do and when they have goals. (18:24) And so if you're if you can do goal setting around the body grief thing, that makes complete sense to me. (18:32) And, yeah, it's really awesome. (18:33) It's positive self talk. (18:35) That's what it is, really.
Scott Benner (18:36) Right?
Erika Forsyth (18:37) That this is a form of it for sure. (18:39) Yeah. (18:39) Yeah. (18:39) Just reminding yourself that even though you don't feel great right now, you in five and six months from now, I know I'm gonna be excited because, to use your example, the show is coming out or this new episode. (18:52) So you're you're reminding yourself internally that the way you're thinking and feeling right now is not permanent.
Erika Forsyth (18:57) It's not fixed.
Scott Benner (18:59) Do know small things give me that feeling? (19:01) I actually thought today when I was thinking about, like, the span of time that I've owned a car in the past that I don't remember driving anymore. (19:09) But at the time, it was my car. (19:12) Like, it was important to me. (19:13) It got dirty.
Scott Benner (19:13) I washed it off. (19:14) I kept it clean inside. (19:15) It got me where I was going, and now it's as if it didn't exist. (19:19) And when I think about, like, struggle the same way, I have struggled in the past too, but that struggle that I remember doesn't exist anymore. (19:26) I actually can't even feel it anymore.
Scott Benner (19:28) And that helps me the next time there's a struggle because I think that there'll be a day in my life where I won't remember this and it'll be gone. (19:36) And therefore, it makes it feel very transient, and it doesn't stick to me the same way then. (19:40) I've been doing that my whole life, though. (19:42) So I don't know what that is. (19:44) I'm sure at some point it was coping, but now I just realized it works.
Scott Benner (19:47) But yeah.
Erika Forsyth (19:49) Yeah. (19:49) Let's see. (19:49) Well, it's coping that works Yeah. (19:51) For you.
Scott Benner (19:51) Who cares. (19:52) Right? (19:52) Anyway, I'm sorry. (19:53) Keep going.
Erika Forsyth (19:54) No. (19:54) It's good. (19:54) Yeah. (19:55) Okay. (19:55) So another, you know, another tool to help you cultivate some more hope is reminding yourself of what she calls anchors.
Erika Forsyth (20:03) The people it could be people, but places or things too that bring you meaning and keep you kind of anchored, tethered to the world no matter how bad things may feel or how bad things may get. (20:18) And so you're remembering this is kind of like you could do even guided imagery exercises. (20:26) Right? (20:26) Anchoring yourself to that feeling that you had laying on the beach that one time. (20:32) It doesn't have to always necessarily be the people that you're counting on because sometimes that might lead you to feel if you're feeling lonely or alone and don't have that sense of support right now, that can also maybe take you down a path you don't wanna go down.
Erika Forsyth (20:46) But just remembering those places, people, things that make you feel connected
Scott Benner (20:52) Right.
Erika Forsyth (20:52) To the world. (20:53) Okay. (20:54) The next couple, you know, becoming a a role model. (20:58) You might even have role models that you look to whether it's on, you know, in your personal life, you know, on social media, but also considering, can you be someone else's role model? (21:13) I think this is oftentimes I know teens and young adults who maybe have gone through a challenging time of kind of integrating diabetes into their identity.
Erika Forsyth (21:24) They often then find great healing and joy by looking kind of backwards and seeing who who can I support now who's newly diagnosed is a is a really beautiful way to kinda help cultivate more of that hope? (21:37) Yeah. (21:37) Okay. (21:39) Last two, play, finding moments of play. (21:42) And I think we often think these can be really like, I need to go into the show.
Erika Forsyth (21:46) I need to go on a trip. (21:47) I need to have buy this big thing. (21:49) But just going back down to the small things of, like, playing a card game. (21:53) I know we'd like know, dancing to your favorite song in the kitchen. (21:57) Like, these are really small things that interrupt the spiral of thinking that you're stuck and that the way you feel is permanent.
Erika Forsyth (22:06) And you're thinking about, well, what am I what hand am I gonna play next? (22:09) What card can I play next? (22:10) Right? (22:10) It's just very, very small things that you might be hard to to start. (22:15) But if you can get to that first few minutes of, like, I'm gonna play I'm gonna press play on this music.
Erika Forsyth (22:20) I'm gonna ask this person to play this game and see what happens.
Scott Benner (22:24) Is that a distraction? (22:25) Is that the is that the role it plays? (22:27) Or am I Yes.
Erika Forsyth (22:28) Yeah. (22:28) Absolutely. (22:29) It's a distraction and then gets you to a different place in your mind. (22:32) It interrupts the thought pattern of a feeling of permanency, of hopelessness, and it gets kind of that little dopamine hit. (22:41) And so this is, you know, separate from maybe going you know, I know we often will wanna go to this to scrolling to get those dopamine hits, but this is something different that's really small within your control.
Scott Benner (22:52) Is there can I take a sidebar for a second? (22:54) Maybe you don't do or don't know the answer to my question. (22:57) Maybe my question's ridiculous. (22:58) But is there a, like, a, intellectual scientific understanding of how people get stuck in that loop? (23:06) Because that is really what because you're describing, like, you're caught in a loop, like, get out of it.
Scott Benner (23:10) And so that your brain can focus on other things. (23:13) You know, you start I don't know. (23:14) I broke up with a girl. (23:15) I broke up, and you keep thinking about it, and then it just feels like it gets heavier and heavier and and worse. (23:20) Almost like a centrifuge.
Scott Benner (23:21) You're stuck to the side. (23:22) You can't peel yourself off the wall. (23:24) It's as faster it goes, the more you're stuck. (23:26) Is there an understanding of why that happens to human beings at all, or is that just the thing we know happens and we're not sure why?
Erika Forsyth (23:33) Like, neuro in a neuropsychological way?
Scott Benner (23:37) Is something happening to them, or is this purely brain chemistry?
Erika Forsyth (23:42) I think it's how our brains operate.
Scott Benner (23:43) Yeah.
Erika Forsyth (23:44) And then we gets we get stuck in this way of thinking, and this is if we're we're gonna delve into, you know, cognitive behavioral therapy and and kind of neuroscience, we get stuck in this way of thinking because, like, with the cognitive behavioral triangle, you know, we will do something and then we think a certain way, and then that makes us feel a certain way. (24:05) Or you could start with a thought, and then we get stuck in
Scott Benner (24:08) that It stutters almost, and then it just kick and it kicks over and does it again. (24:11) Yes. (24:12) Yeah. (24:12) Yeah.
Erika Forsyth (24:12) And now neuro like, neurologically neuro kind of in a psychological way, I'm not sure I could explain why, but I think that's a good question for us to explore.
Scott Benner (24:25) How do you get on that off ramp when you feel it coming?
Erika Forsyth (24:29) You know? (24:30) Because That's that's yeah. (24:31) That's another
Scott Benner (24:32) I have a I have a silly example. (24:34) Okay? (24:34) Okay. (24:34) Sorry for everybody. (24:36) I guess I'm announcing here one of my chameleons has passed away.
Erika Forsyth (24:39) And Oh, I'm sorry.
Scott Benner (24:41) She lived a good long time and made it pretty far. (24:44) But I had space and a and a different animal that I had considered, getting for a number of years. (24:50) And yesterday, I went to pick it up, and I've done all of my research. (24:56) I'm completely comfortable on how to take care of it. (24:59) I have the cagings correct.
Scott Benner (25:00) Everything about it is right. (25:02) I have the desire. (25:03) I can afford it. (25:04) Like, the entire thing. (25:05) Like, I there's nothing there.
Scott Benner (25:06) The only thing that exists that is outside of my control is that I've never owned this kind of animal before, and I have some trepidation about that. (25:14) But that's it. (25:15) It it's it's a healthy amount of trepidation. (25:18) And as I was driving to the FedEx location to pick it up, I felt myself getting nervous to the point where I thought, oh my god. (25:27) I shouldn't have done this.
Scott Benner (25:29) And as soon as I had that thought, I stopped myself and I went, oh, shut up, idiot. (25:34) You're just nervous because you don't know what's about to happen. (25:38) You just can't see on the other side of the wall. (25:40) Like, you've got it all thought through. (25:42) You're good to go.
Scott Benner (25:43) You'll know what to do as the things happen. (25:45) But my god, how interesting is that? (25:47) That even on something so small that I prepared so much for that my brain was able to look at me and go, hey. (25:55) You are making a huge mistake right now. (25:57) And I don't know why I was able to go I mean, it's a small example, but, like, what allows you to go, I'll be alright, and keep going and trust yourself versus getting caught in that stutter spiral and then going, oh god.
Scott Benner (26:10) I did the wrong thing. (26:11) I gotta call the guy and take it back and hopefully he'll refund it. (26:14) Like like you know what I mean? (26:15) Like but, you know, why can't you get off that that ramp when when it's the right thing to do? (26:20) I don't know.
Scott Benner (26:21) Sorry.
Erika Forsyth (26:21) Well, so you you probably have had experience of interrupting that thought. (26:27) You know, we have all these different types of cognitive distortions that could be you know, they're they're fear based. (26:32) They're they're all different reasons why we have different distortions, like catastrophic thinking, black and white thinking, magical thinking. (26:40) And so in that moment, you are having some normal, probably, anxiety and fear based from probably your grief.
Scott Benner (26:47) Mhmm.
Erika Forsyth (26:47) I I don't know if we're doing really quick analysis here. (26:51) And and then you were able to interrupt it, and you did some externalizing and names like, oh, this is this is fear talking.
Scott Benner (26:58) Mhmm.
Erika Forsyth (26:59) Right? (26:59) That's what we talk about in the CBT tool is to, like, name and notice when those thoughts are happening, and that takes practice because then you're you're noticing it. (27:08) You know what it sounds like. (27:10) You're naming it, and then you're interrupting it. (27:12) You you chose shut up, stupid.
Erika Forsyth (27:14) Yes. (27:14) Sometimes that works for people. (27:16) Sometimes it doesn't.
Scott Benner (27:17) Right.
Erika Forsyth (27:17) That might cause more kind of conflictual dialogue in people's minds. (27:21) Yeah. (27:21) But it could also be like, oh, you could choose, like, the compassionate way of like, oh, this is this is you feeling nervous. (27:29) This is me feeling nervous, and I think I I've got the tools, and we're gonna give it a go.
Scott Benner (27:33) I will tell I'll give you the end of how I taught after I told myself to shut up, I I actually I gave myself some grace back. (27:39) I can't believe I'm using words like this. (27:41) I've become
Erika Forsyth (27:42) This is good.
Scott Benner (27:42) I've become such a hippie. (27:44) But You become self compassionate. (27:47) I said to myself, this is good. (27:49) There's a thing out in the world that makes me a little nervous. (27:51) That's good.
Scott Benner (27:52) I should keep doing things that make me feel like I don't exactly have control over this. (27:57) Like, that's how I'm gonna grow. (27:58) And, you know, and and I get so I ended up just I basically took the thing I was afraid of and then gave myself credit for it and then just zipped on, didn't think about it again. (28:07) Okay. (28:08) Alright.
Scott Benner (28:08) I I don't know. (28:09) I feel like that story fit here. (28:10) But
Erika Forsyth (28:10) It did. (28:11) No. (28:11) I think it's good because it's, yeah, again, we're noticing those patterns. (28:16) You're naming it, interrupting it, and then you offered but then the tool was the compassionate self talk
Scott Benner (28:22) Mhmm.
Erika Forsyth (28:22) And not the shame. (28:23) Like, oh, you did this again. (28:24) Right? (28:25) Because then that keeps you trapped.
Scott Benner (28:26) Yeah. (28:26) I didn't feel bad for that. (28:28) I just I probably just you know, the shut up stupid part. (28:32) That was just how I was raised. (28:34) Like, you know, if and so I I know I can shut my emotions off if if I get yelled at.
Scott Benner (28:38) So I was like, okay. (28:39) Like, I'll just stop myself for a second. (28:41) Then once I had a clear mind, I recognized why I was nervous. (28:45) And I and then I actually thought and it's funny. (28:48) It's not a feeling for me.
Scott Benner (28:49) I've heard other people say it, that it's good to do things that stretch you, that make you a little nervous. (28:54) Right? (28:54) And I thought, okay. (28:55) Well, I'll just believe those people who say that, and I'll apply that to myself, and I was on my way again. (29:01) So Mhmm.
Scott Benner (29:02) Mhmm. (29:02) My point is is that if you just believe Erica, you should be able to apply it and move on. (29:07) I mean, hopefully, good luck and all. (29:09) But
Erika Forsyth (29:09) yeah. (29:09) Yes. (29:10) Yeah. (29:10) I wanted to say well, I'm sorry for the loss of your chameleon, and I am tempted to ask you which animal that maybe you're you wanna save that for another time. (29:20) I can't see because of your
Scott Benner (29:21) Yeah. (29:21) I'm blurred out in the background. (29:23) Yeah. (29:23) You're fine. (29:23) I'll save that for another time, Erica.
Scott Benner (29:25) Yeah. (29:25) Yeah. (29:25) But I I I gotta get it's not a chameleon. (29:28) It's a different kind of lizard. (29:29) Okay.
Scott Benner (29:30) So Okay. (29:31) Alright. (29:31) That's what I'll say for now.
Erika Forsyth (29:32) Okay. (29:33) Alright. (29:33) And we will wait anxiously to
Scott Benner (29:35) hear more. (29:36) At some point in 2026, I'll Yeah. (29:39) I can't give it all away today. (29:40) Okay?
Erika Forsyth (29:41) Oh, gosh.
Scott Benner (29:43) I'm sorry. (29:43) Go ahead. (29:43) So
Erika Forsyth (29:44) okay. (29:44) So I think we we are gonna actually move into some self compassion and some tools, but I think one last tool in terms of the hopelessness and hope conversation is, you know, if you're able to ask yourself, what what do you need in that moment? (30:00) Is it is it some an actual physical hug from someone? (30:04) Is it a phone call, or do you need a solution? (30:07) Do you need a fix?
Erika Forsyth (30:08) Do you need more support from your endo? (30:12) Do you need more support from how to change your rates? (30:16) You know, just being able to ask yourself, okay. (30:19) I'm really feeling stuck, but what is it that I need? (30:21) And sometimes hard to identify what you need in that moment.
Scott Benner (30:24) Yeah.
Erika Forsyth (30:25) And it might take a couple tries to say, maybe I need this. (30:27) Maybe I need that.
Scott Benner (30:29) Yeah. (30:29) No. (30:29) I I hope I hope everybody finds that answer. (30:31) But okay. (30:32) Move move please move on.
Erika Forsyth (30:33) Okay. (30:33) Yes. (30:33) Let's move on. (30:34) So when you are experiencing hopelessness, believing that someday you will feel hope again, practicing that blind faith, recognizing that I think it's important to recognize that self compassion and gratitude go hand in hand. (30:52) And perhaps I don't know if I've said this quote before in previous episodes, but this is one of my favorites in the book is we cannot hate ourselves into becoming what we will be grateful for someday.
Erika Forsyth (31:05) Right? (31:05) That is shame. (31:06) And we often feel like shame can move us, but it keeps us trapped. (31:11) So switching that and thinking for this diabetes example, if you're looking at your numbers, right, and you're saying, okay. (31:19) My numbers are higher today than I want them to be, or I miss bolus whatever for this meal.
Erika Forsyth (31:25) That's okay. (31:26) I'm allowed to be flawed. (31:28) I'm allowed to be human, and I'm grateful that I have the ability to make a correction now or next time. (31:35) Right? (31:35) So this is obviously, we're gonna we wanna look at patterns, and we need to make shifts.
Erika Forsyth (31:40) But this is you know, if you're noticing that you're experiencing the shame and, like, why why can't I get this? (31:45) Why can't I figure this out? (31:46) Why do I keep messing up? (31:48) Going back to not only the self compassion, but trying to integrate moments of that gratitude too. (31:54) Like, okay.
Erika Forsyth (31:55) I messed up. (31:56) It's okay. (31:57) I'm gonna make I'm gonna make a I'm grateful that I can make this correction now. (32:01) I can do something different next time. (32:03) That leads us to the final stage, body trust, which is a reminder, the definition is in order to trust our bodies, our body needs to trust us to take care of it, be kind to it, and nourish it in all ways.
Erika Forsyth (32:16) So, again, body trust is not this final destination that we're trying to reach, but something that we want to kind of practice and integrate as you're moving through these stages. (32:26) Body trust is something that is innate, but we kind of skip over that. (32:32) Like, we for when we're hungry, we our body gives us this cue, and it growls. (32:37) But oftentimes, instead of, you know, having being able to have a meal and sit down and enjoy it, we'll grab a a bar and run. (32:46) I know that's not always practical to be able to do that, but just we're talking about, like, consistently maybe ignoring
Scott Benner (32:52) Mhmm.
Erika Forsyth (32:52) These cues. (32:53) Maybe you're you're sleepy every afternoon, and we just you know, instead of taking a nap, you drink your third cup of coffee, which I can be certainly guilty of. (33:03) Right? (33:03) So instead of taking a nap, resting, listening to your body, we're kind of pushing through those cues. (33:08) Practicing body trust can be intuitive, but oftentimes we get so consumed by this by societal pressure, by our kind of culture that that your that your body is defective, right, when we're when we're diagnosed with something.
Erika Forsyth (33:27) But it actually we we know it's not. (33:30) And it understanding that we're we wanna be more okay with not being okay because it's really normal. (33:38) Like, I wonder, you know, if we were to take a toll a poll of everyone every day and how many people are like, I'm great. (33:44) I'm fine. (33:45) Or we or more people are like, I'm I'm not okay, but I'm just pretending.
Erika Forsyth (33:49) You know?
Scott Benner (33:49) I always think that, there's got you know, we we people are like, oh, I'd like to be normal. (33:54) Like, you know, I hear people say all the time, like, my kid got diabetes. (33:57) I just want them to be normal. (33:59) Between diabetes and everything else and all the other things that go wrong with people's bodies as they age, I would imagine that people who don't have any issues are probably far fewer than the ones that do. (34:08) Aren't we normal and they're not?
Erika Forsyth (34:10) Yeah. (34:11) Yeah. (34:11) You know? (34:12) And what and, yeah, what is normal? (34:13) You know?
Erika Forsyth (34:14) I think
Scott Benner (34:14) It really does lead you into expectation. (34:17) Like Mhmm. (34:18) You expect your body to be perfect, but, I mean, look around. (34:21) That's not really what happens. (34:22) I mean, I don't know that I know anyone well who I could say they don't have one issue and their system just works perfectly.
Scott Benner (34:31) You know? (34:32) And if even if the ones that do eventually will run into something, and I don't mean like, you know, I don't mean death at the end. (34:37) I mean, along the way, like, body wears out. (34:39) It's a machine. (34:40) You know?
Scott Benner (34:40) It rubs and it rubs and breaks down. (34:43) So okay. (34:44) I'm sorry. (34:45) Anyway, just think of try thinking of maybe you're normal and they're not. (34:47) That's what I was gonna say.
Erika Forsyth (34:50) Yeah. (34:51) As you are trying to integrate this practice of the two way street of, you know, listening to your body and your body trusting you, So trying to listen and respond to your body cues with compassion instead of just, like, ignoring it, having the coffee, pushing through. (35:04) And, again, I know it's not practical all the time, but just trying to integrate some of that.
Scott Benner (35:09) Yeah.
Erika Forsyth (35:10) Okay. (35:11) So how do you build more moments of body trust? (35:16) I know we've talked about self care various times throughout all of our episodes that we've recorded, but I think it I like this perspective and that self care is not about indulgence. (35:28) Even though in our, you know, in our capitalist society, we are often told that buying the thing that you've always wanted or getting the massage or doing the thing that will make you happy. (35:40) That's a form of self care.
Erika Forsyth (35:42) And while, certainly, that is, and it's about you know, you're trying to make yourself feel better, what we wanna kind of shift is that basic self care is is about listening to your body and giving it what it needs and not necessarily always trying to make it feel better. (36:02) Does that does that make sense that shift of, like, we're trying to listen and build trust with our body as opposed to trying to just always and and and in in that process, you might feel better, but we're not doing the thing that's gonna make it feel better in the moment all of the time.
Scott Benner (36:19) Support yourself without expecting perfection afterwards. (36:23) Give it the thing like, I I went to I I got a massage last week. (36:26) I'm not embarrassed, Erica.
Erika Forsyth (36:28) No. (36:28) That's good. (36:29) Massages are great.
Scott Benner (36:30) My hip pointers were really sore, and my lower back is always stiff, and my neck is stiff. (36:35) Right? (36:35) So when I went in, you know, the person asked me, like, what what are my problem areas? (36:40) So my neck's stiff, my neck's stiff, my lower back, and, you know, my hips. (36:44) And I left and she when she got all the pain out of my hips.
Scott Benner (36:47) And she loosened up my neck. (36:49) It isn't great, but it was better. (36:50) And I left thinking, oh, good. (36:52) This was an improvement. (36:53) That's what you're talking about.
Scott Benner (36:54) Like, do something, but, like, I could have left going, like, well, my shoulders aren't completely better and my back still feels a little stiff, so this is a waste of time. (37:02) Like, just is that what you're saying? (37:04) Like, don't expect perfection at the end? (37:05) Just do something for yourself and hopefully, cumulatively, it might help?
Erika Forsyth (37:09) Yes. (37:10) And
Scott Benner (37:10) Oh, I I missed it. (37:12) Go ahead.
Erika Forsyth (37:12) No. (37:12) No. (37:13) I think so getting a massage, buying that sweater you've always wanted, taking that trip that you've always longed to do, that those are all beautiful and great things to do. (37:25) But if you're hanging your hat on that type of what we might label as self indulgence as always trying to make yourself that's what you you do to make yourself feel better, that isn't necessarily building the body trust. (37:38) Yeah.
Erika Forsyth (37:39) Because, a, you can't always maybe afford it. (37:41) You might not have the time. (37:42) And then you realize, wait. (37:44) But I'm still feeling this way, or I'm still kind of questioning why did this happen to me.
Scott Benner (37:50) Don't fall back on big gestures and use them as, a pacifier. (37:54) Is that the idea?
Erika Forsyth (37:55) Yes. (37:56) Yes. (37:56) So I think what maybe we give some examples of, like, building body trust and what basic self care looks like. (38:03) So it's going back to, you know, eating when you're hungry, sleeping when you're tired, crying when you're sad, like, letting yourself connect physically with your body and what it needs. (38:14) Mhmm.
Erika Forsyth (38:14) You know, hygiene, being practicing hygiene self care. (38:19) Maybe it's taking a longer shower. (38:21) And for some people, it might mean brushing your teeth twice a day. (38:24) Sometimes that can be hard to do given whatever stage of grief you might be in. (38:29) Maybe it's, using perfume or lotion that you save for special occasions and use it at the day you're at home.
Erika Forsyth (38:36) Right? (38:37) K. (38:38) Building in time to call your friends. (38:41) Some people for for diabetes, after showers, they like to take a little bit longer before they put their devices on if you're happen to have a, you know, the the naked shower or the whatever. (38:54) You know what I mean?
Scott Benner (38:54) Naked shower is one of my favorite diabetes terms because it must
Erika Forsyth (38:57) sound funny.
Scott Benner (38:57) It must sound ridiculous to everybody else.
Erika Forsyth (38:59) Yeah. (38:59) Yeah.
Scott Benner (39:00) Yeah. (39:00) Yeah.
Erika Forsyth (39:01) Even I yeah. (39:02) It it is a funny thing because we usually are naked when we shower, but we know what that means.
Scott Benner (39:06) Wait. (39:07) You take all your clothes off in the shower? (39:10) I think I'm doing it wrong. (39:11) Okay. (39:12) No.
Erika Forsyth (39:12) So taking taking that just that if you are able to, obviously, making sure you're safe, etcetera, but tending to your body, listening to your body, giving it what it needs, not only basic self care, hygiene, digital hygiene, being mindful of, you know, as we've talked about before, how much time you're spending on social media for people who only have diabetes accounts and they follow only diabetes, you know, groups, influencers, etcetera, I know that can be really encouraging and supportive and you feel like you're a bigger part of this community. (39:46) But I know it also can lead to feeling either envious or you kind of get stuck in this comparison trap. (39:53) And so just being mindful of your digital hygiene practice as well.
Scott Benner (39:57) In all the years we've been doing stuff together, Erica, you finally said something I cannot get behind. (40:01) I need everybody to listen to the podcast and keep following on the podcast. (40:05) I think you may With
Erika Forsyth (40:06) the exception of juice bugs, always follow Yeah.
Scott Benner (40:08) Yeah. (40:08) No. (40:09) But no. (40:09) I you make a great point there, and I've actually I get to watch people have an experience of being group experts in the Facebook page. (40:18) And my feeling about how to manage that a big community like that very much is that it's about sharing information with people, pointing them in the right direction.
Scott Benner (40:28) You know, if people are being, you know, horrible, stopping them, that kind of stuff. (40:32) But mostly, I just I'm live and let live. (40:34) I like to see adults act as adults and figure things out for themselves. (40:38) But I've seen that sometimes you can make somebody, you know, a group expert, for example, and it gives them a pressure that they have to impact the thing. (40:47) And and I can see the anxiety that it puts on them, some of them, when they see something and they think that can't stand like that.
Scott Benner (40:57) It needs to be commented on or changed or stopped or, you know, corrected or whatever. (41:03) And then there are times when they realize they don't they don't have power over it and it is it it causes what I would call consternation with them. (41:11) Like, they can't just walk away from it. (41:13) I've been doing this a long time, and I recognize that, you know, we've got some ways we do things. (41:20) We do them that way.
Scott Benner (41:21) If it doesn't work out, we tried, but it's not on me. (41:26) I can't carry that. (41:27) That's not a wait for me to carry after that. (41:30) I did what I could do. (41:31) If you don't wanna interact with it in a way that's gonna resolve it, I feel bad for you, but I gotta move on.
Scott Benner (41:37) But I see some people can't think it's stuck. (41:39) Like, we you know, I but we can't let them say that. (41:42) It's wrong or, you know, some I'm like, no. (41:45) It's just their people talking. (41:47) Like, you can't you can't make yourself responsible for everything coming out well.
Scott Benner (41:51) And I can see that bigger picture happening to people when they're involved in this too. (41:56) Like, they get that feeling of, like, you feel responsible for what the whole world's saying, and that is just not a reasonable position to put yourself in. (42:03) Mhmm. (42:04) Yeah. (42:04) Mhmm.
Scott Benner (42:04) I appreciate you bringing that up.
Erika Forsyth (42:06) Yeah. (42:06) That's it's just another thing to be mindful of, you know, what Yeah. (42:11) How much time you're spending and how is that impacting how you feel, for whatever it may be.
Scott Benner (42:18) You can get caught up in something too and not see the forest or the trees in those situations. (42:22) And Mhmm. (42:23) And that's that's why I think putting it down once in a while, anything really, and getting some distance from it really does help, you know, refocus your perspective. (42:31) So I'm sorry. (42:32) You
Erika Forsyth (42:32) Yes. (42:33) This is good. (42:34) Okay. (42:34) So a few more examples of, you know, trying to build increase more moments of body trust. (42:40) Obviously, regulating your nervous system with with breathing, with grounding.
Erika Forsyth (42:44) We know that tool, and that can be a very small but significant tool. (42:49) Building trust with others, you know, have offering empathy and compassion towards people, but also reminding yourself that they are human.
Scott Benner (42:59) Mhmm.
Erika Forsyth (43:00) But then also leaning on them. (43:01) Right? (43:01) I think so often, we might be hesitant to reach out for help because we think, well, mate, they've got too much going on. (43:11) How could they ever listen to what I need or what I'm going through? (43:16) And then that keeps you trapped and isolated.
Erika Forsyth (43:19) So it's risky. (43:20) It's risky to build trust in this kind of the healthy codependency with others, but that is a tool to to build some of this body trust. (43:29) And then finally, this is the probably the hardest thing is surrendering, letting go of control, and accepting that life isn't fair all the time. (43:40) And this this is hard because we don't wanna accept that. (43:44) We wanna fight.
Erika Forsyth (43:45) We wanna make sure we are the healthiest possible and pain free and chronic illness free. (43:51) But when more we lean into this and say, okay. (43:55) This is I cannot control what happened. (43:57) This happened to me, or I got diagnosed with this. (44:02) The more we can trust that we don't always have control, we don't always get what we want, but we can practice building that body trust that we have everything we need in our body.
Erika Forsyth (44:14) And that goes right back to then to the basics again of eating when you're hungry, sleeping when you're tired. (44:21) So it's kind of this full circle loop that, hopefully, all of these tools will help you move through these body grace stages. (44:30) Again, body trust is something that we don't it's not like you once you do this all the time, you've, like, arrived. (44:37) Right? (44:37) These are things that we can always practice and integrate as we feel in shock or we're in the apology stage or fight stage or what wherever it might be.
Scott Benner (44:47) Great conversation. (44:48) That's really wonderful. (44:49) I have to ask a question. (44:51) I mean, we're pretty much through and gotten through what you wanted to talk about, and I'm gonna pull the curtain back for some people. (44:57) A few moments ago, Erica's reading, and she's got some notes for herself here.
Scott Benner (45:02) And in under examples of regulate your nervous system, she has three examples. (45:06) She read you two of them and skipped the third one, and I thought
Erika Forsyth (45:09) Oh, yeah.
Scott Benner (45:10) I did. (45:10) That because she doesn't want me to say something stupid, or did she miss it? (45:14) Now
Erika Forsyth (45:17) you want me to say.
Scott Benner (45:17) I yes. (45:18) Did you skip it because she thought dummy's gonna say something dumb if I say self massage? (45:23) No. (45:23) Okay.
Erika Forsyth (45:23) Because when I when I have spoken, you know, I I have spoken on this topic before, and I know I'm pretty sure I've said self massage. (45:32) I don't know. (45:33) I wonder, Scott. (45:34) I wonder if I had said that you might have said something, and that would have made me feel embarrassed.
Scott Benner (45:39) I actually was thinking, like, is she trying to like, is her because I I really looked at your face. (45:45) And when you skipped it, I laughed to see to see if you would acknowledge my laughter, but you didn't. (45:51) So, like, so I So
Erika Forsyth (45:52) I might have done it.
Scott Benner (45:54) Yeah. (45:54) The adult inside of you is like, let's not go down this road with this guy.
Erika Forsyth (45:57) The I am not conscious of what decision I made there, but you're right. (46:02) I mean, I think I skip around a little bit here and there.
Scott Benner (46:05) Yeah. (46:05) Yeah. (46:05) I wanna make sure clear to people. (46:06) Like, Erica's not reading. (46:08) She has, like, an outline for herself that she puts together.
Scott Benner (46:11) And but sometimes when she hits examples that she's laid down for herself, she goes through them. (46:16) And so I listen. (46:18) So people can get the curtain pulled back a little bit. (46:20) I've been trying to do a better job of keeping up with your notes because I think there are times in the past when I'm, like, coming to these realizations and realizing
Erika Forsyth (46:28) to the end too quickly.
Scott Benner (46:30) And then and Erica's like, oh, I was getting to that, man. (46:32) Stop it. (46:32) Yeah. (46:34) It's because I'm unaware of her notes. (46:35) I'm just going through the process with her, and she's giving me moments as I'm listening.
Scott Benner (46:40) But I've been trying to look while you're like, I don't know if you've noticed. (46:43) I haven't been looking at you as much. (46:44) I've been looking at what you're reading. (46:46) Right? (46:47) And, boy, I just was like, you were, like, grounding, deep breathing, and then you went to and you can trust others like, damn.
Scott Benner (46:53) She skipped right over self massage. (46:56) Also, what is self massage? (46:57) Is that me rubbing my own arm or something? (46:59) Is that really helpful?
Erika Forsyth (47:01) Yeah. (47:01) Or, like, people do they can put, you know, pressure points on your forehead.
Scott Benner (47:07) To myself?
Erika Forsyth (47:08) Yeah. (47:09) Alright. (47:10) Yeah. (47:10) Or on your your palms.
Scott Benner (47:12) What do I get married for? (47:13) Why do I have to do this? (47:14) I
Erika Forsyth (47:15) mean, there's all different types.
Scott Benner (47:18) Do you know the one in between your thumb and your pointer finger? (47:20) You press into that web there? (47:22) Yeah. (47:23) Uh-huh. (47:23) That's a good one.
Erika Forsyth (47:24) Yeah. (47:24) That is a good one. (47:25) Yeah. (47:26) All sorts of and those those are some examples.
Scott Benner (47:29) Yes. (47:30) Yes. (47:30) Well, thank you. (47:32) I I hope I hope
Erika Forsyth (47:33) you Oh my gosh. (47:34) I can't believe we're ending on on this, but I kind of can. (47:37) Yeah.
Scott Benner (47:37) I mean, what are we gonna do? (47:38) I'm trying to keep it light. (47:41) Listen. (47:41) We just did a whole series about what happens when people feel like their body abandoned them. (47:45) I was like, if we don't try to lighten this up, my goodness.
Scott Benner (47:48) I hope Jay Mattingly hears this. (47:50) I hope she's, impressed Yes. (47:51) Impressed with our breakdown of of her book. (47:54) And, and and you really do suggest people go out and get the book. (47:58) Right?
Erika Forsyth (47:59) Yes. (47:59) I think it's I mean, it's she covers a lot. (48:01) I mean, this is we're we're covering the basics, but I think it's the first book that I have read that really connects to the experience of not just grief stages that we've talked about a lot over the years, but really apply it to the physical sense of loss that people experience with the diagnosis of diabetes.
Scott Benner (48:23) Listen. (48:23) A bunch of you go get that book, like it, and then leave a nice Amazon review that mentioned you heard it on the podcast. (48:29) Maybe we'll get Jane Mattingly on, and then Erica can keep I'll in invite Erica on and she'll geek out and ask her a bunch of questions.
Erika Forsyth (48:36) Yes. (48:36) I'll sit
Scott Benner (48:36) in the background and just wait for self massage to pop up again. (48:40) Doing my part in this whole thing, which apparently is listening to smart people talk than saying something stupid that dumbs down their conversation.
Erika Forsyth (48:48) Oh my gosh.
Scott Benner (48:49) I was interviewing someone the other day, and she's such a such a bright lady, and she laid this whole thing out. (48:55) And then I kinda, threw a synopsis together, and she goes, well, you really reframed that wonderfully. (48:59) I was like, that's my whole job. (49:01) I was like, I've come to understand that's actually my job. (49:04) So, anyway
Erika Forsyth (49:06) That's a skill.
Scott Benner (49:06) Yeah. (49:07) Appreciate you bringing this to me. (49:08) Do you have any idea? (49:09) Let us let us tease the audience. (49:10) Do you have any idea what you think you and I are gonna do next?
Erika Forsyth (49:13) I know we've talked about it, and we've written it down, but I cannot recall the moment.
Scott Benner (49:20) Or it's like, it's written down somewhere. (49:22) I don't remember what it is. (49:23) And trust me, I don't either. (49:24) That's why I was asking you.
Erika Forsyth (49:27) We have a list somewhere.
Scott Benner (49:31) Let them wonder. (49:32) It's fine. (49:34) These people gotta go. (49:35) They gotta go back to work. (49:36) I mean, there oh, you guys are all just
Erika Forsyth (49:38) sitting teen a a teen series. (49:41) I know we've talked about that.
Scott Benner (49:42) You will find something.
Erika Forsyth (49:43) Don't worry. (49:44) Yeah. (49:44) It'll be Yeah. (49:45) It'll be great.
Scott Benner (49:45) Scotty will come up with something or Erica will. (49:47) Like, this was your baby here, this body grief
Erika Forsyth (49:50) thing.
Scott Benner (49:50) Yes. (49:51) Yeah. (49:51) Yeah. (49:51) Actually, if you ever see Erica out in the wild giving talks, she does a great little, little breakdown of body grief in person you might wanna check out.
Erika Forsyth (49:59) Oh, thank you. (50:00) Of course.
Scott Benner (50:01) Do you have any talking, speaking gigs coming up?
Erika Forsyth (50:03) The only one for sure is next September.
Scott Benner (50:07) Could be by Touch by Type one.
Erika Forsyth (50:08) Touch by Type one. (50:09) Okay. (50:10) Uh-huh.
Scott Benner (50:10) Yes. (50:11) See there too. (50:11) That's the yearly time when Eric and I have dinner together.
Erika Forsyth (50:14) Yes. (50:14) It's lovely. (50:15) The annual conference in Orlando.
Scott Benner (50:17) Nine more months, then we can do it again. (50:19) Yeah. (50:20) Alright.
Erika Forsyth (50:21) Is it really nine months till then?
Scott Benner (50:22) I mean, it's January.
Erika Forsyth (50:23) Oh my gosh. (50:23) Yeah. (50:24) Yeah. (50:24) That's how it works.
Scott Benner (50:25) I isn't it I'm at the age where I'm like, god. (50:26) If I live that long, that'll be amazing. (50:28) I know that's ridiculous, but it's how I feel.
Erika Forsyth (50:30) Yeah. (50:31) I think you're on a good check.
Scott Benner (50:32) Yeah. (50:32) We'll see. (50:33) Thank you so much for doing this. (50:34) Erica foresythe dot com. (50:36) Head over.
Erika Forsyth (50:36) Thank you.
Scott Benner (50:37) Yep.
Erika Forsyth (50:37) Thank you, Scott.
Scott Benner (50:38) Bye.
Erika Forsyth (50:38) Bye.
Scott Benner (50:46) The conversation you just heard was sponsored by Touched by Type One. (50:50) Check them out, please, at touchedbytype1.org on Instagram and Facebook. (50:55) You're gonna love them. (50:56) I love them. (50:57) They're helping so many people at touchedbytype1.org.
Scott Benner (51:01) Today's episode is also sponsored by the new Tandem Mobi system and Control IQ Plus technology. (51:08) Learn more and get started today at tandemdiabetes.com/juicebox. (51:13) Check it out. (51:15) Are you tired of getting a rash from your CGM adhesive? (51:19) Give the Eversense three sixty five a try.
Scott Benner (51:21) Eversense cgm.com/juicebox. (51:25) Beautiful silicone that they use. (51:27) It changes every day. (51:27) Keeps it fresh. (51:29) Not only that, you only have to change the sensor once a year.
Scott Benner (51:32) So, I mean, that's better. (51:36) Okay. (51:36) Well, here we are at the end of the episode. (51:38) You're still with me? (51:39) Thank you.
Scott Benner (51:39) I really do appreciate that. (51:41) What else could you do for me? (51:43) Why don't you tell a friend about the show or leave a five star review? (51:47) Maybe you could make sure you're following or subscribed in your podcast app, go to YouTube and follow me, or Instagram, TikTok. (51:56) Oh, gosh.
Scott Benner (51:56) Here's one. (51:57) Make sure you're following the podcast in the private Facebook group as well as the public Facebook page. (52:03) You don't wanna miss please, do you not know about the private group? (52:07) You have to join the private group. (52:09) As of this recording, it has 74,000 members.
Scott Benner (52:12) They're active talking about diabetes. (52:15) Whatever you need to know, there's a conversation happening in there right now. (52:19) And I'm there all the time. (52:20) Tag me. (52:20) I'll say hi.
Scott Benner (52:26) If this is your first time listening to the Juice Box podcast and you'd like to hear more, download Apple Podcasts or Spotify, really any audio app at all. (52:35) Look for the Juice Box podcast and follow or subscribe. (52:38) We put out new content every day that you'll enjoy. (52:42) Wanna learn more about your diabetes management? (52:44) Go to juiceboxpodcast.com up in the menu and look for bold beginnings, the diabetes pro tip series, and much more.
Scott Benner (52:51) This podcast is full of collections and series of information that will help you to live better with insulin. (52:59) Hey. (52:59) What's up, everybody? (53:00) If you've noticed that the podcast sounds better and you're thinking, like, how does that happen? (53:05) What you're hearing is Rob at Wrong Way Recording doing his magic to these files.
Scott Benner (53:11) So if you want him to do his magic to you, wrongwayrecording.com. (53:15) You got a podcast? (53:16) You want somebody to edit it? (53:18) You want Rob.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#1780 Best Of Juicebox: Type 3c Diabetes
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
I am re-sharing this episode in memory of Lara.
Lara lived with type 3c diabetes after losing her pancreas, spleen, gallbladder, and part of her stomach during surgery for a pancreatic tumor. In this conversation, she shared what that life looked like — the physical challenges, the learning curve, and the strength it took to keep going.
Lara has since passed away. Her mother asked if I would run this episode again in her memory. I am honored to do so.
If you didn’t hear Lara the first time, listen now. If you did, maybe you’ll hear something new. Lara’s story matters.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner (0:0) Hello, friends, and welcome to episode 1,109 of the juice box podcast. (0:13) 46 year old Lara has type three c diabetes. (0:17) She lost her pancreas, spleen, gallbladder, and part of her stomach during a pancreatic tumor surgery. (0:23) Lara found the podcast while she was looking for help with her new diabetes. (0:27) She found episode two seventy nine and has been a listener ever since.
Scott Benner (0:32) Nothing you hear on the juice box podcast should be considered advice, medical or otherwise. (0:37) Always consult a physician before making any changes to your health care plan. (0:44) When you place your first order for a g one with my link, you'll get five free travel packs and a free year supply of vitamin d. (0:52) Drink ag1.com/juicebox. (0:57) Don't forget to save 40% off of your entire order at cozyearth.com.
Scott Benner (1:02) All you have to do is use the offer code juice box at checkout. (1:05) That's juice box at checkout to save 40% at cozyearth.com. (1:11) If you're looking for community around type one diabetes, check out the Juice Box Podcast private Facebook group, Juice Box Podcast, type one diabetes. (1:21) If you're not already subscribed or following in your favorite audio app, please take the time now to do that. (1:26) It really helps the show.
Scott Benner (1:32) This episode of the juice box podcast is sponsored by the continuous glucose monitor that my daughter wears, the Dexcom g seven. (1:40) Dexcom dot com slash juice box. (1:43) Get started today using this link, and you'll not only be doing something great for yourself, you'll be supporting the juice box podcast. (1:50) This show is sponsored today by the glucagon that my daughter carries, Gvoke HypoPen. (1:56) Find out more at gvokeglucagon.com/juicebox.
Lara (2:02) My name is Lara. (2:04) I am Canadian. (2:05) I live in Canada in British Columbia about an hour outside of Vancouver. (2:09) I am 46 years old. (2:12) I'm married and have one daughter who is 17 graduating high school this year, and we couldn't be more excited about that.
Scott Benner (2:20) Nice.
Lara (2:21) And I'm currently in a battle with pancreatic cancer.
Scott Benner (2:25) Not as nice. (2:26) Okay. (2:28) I okay. (2:29) So my first question is, before we started recording, because of the spelling of your name, I said, is it Lara? (2:34) And you said, yes.
Scott Benner (2:35) But then because of your Canadian accent, I thought you said Laura. (2:38) So now I don't know what to do.
Lara (2:40) You know what? (2:41) It's a okay by me. (2:42) I it's pronounced Lara. (2:44) I get Lara, Laura. (2:46) It doesn't bother me whatsoever.
Scott Benner (2:48) But I wanna get it right.
Lara (2:49) It's Lara.
Scott Benner (2:52) I'm leaning on the r too much. (2:54) Right?
Lara (2:54) Lara.
Scott Benner (2:55) Yeah. (2:56) So Lara, did I get it?
Lara (2:57) Yep. (2:58) I got it. (2:58) Got it.
Scott Benner (3:01) Well, I was gonna curse right off the bat and say, shit. (3:04) That sucks. (3:05) But, when did you learn about the cancer?
Lara (3:09) Well, it was March. (3:11) I'm gonna back up a little bit because it all started in March 2021. (3:16) I was two weeks out of moving. (3:18) We had a major move, underway to move to Acreage, in a much larger house. (3:24) And two weeks before our giant move, I ended up in the hospital with pancreatitis, which was unusual for someone of my age.
Lara (3:34) And I spent seven days in the hospital being treated for pancreatitis. (3:39) I'd had all of the CTs, the MRIs. (3:42) Everything came out perfectly clear, clear pancreas. (3:46) They did find in July when I had the secondary scan an abnormality in a bile duct. (3:54) And at that point, they told me that they were going to monitor it, and I might need to have my gallbladder out.
Scott Benner (4:01) Okay. (4:02) So Can can I ask first? (4:04) Let me let me Yep. (4:05) Let me step you through it. (4:07) What are the symptoms that landed you in the hospital initially?
Lara (4:11) I had a terrible, terrible back pain. (4:14) So it was radiating in the middle of the night from my, mid back through my shoulder blades, severe nausea, oily stool, abdominal pain, and just a general feeling of unwell. (4:30) But, actually, by the time I ended up in the hospital, my symptoms had recovered, but my blood work was still showing, high lipase numbers, and inflammation markers were up. (4:45) So the only way to fix that is to put you on IV drip only and no food for seven days.
Scott Benner (4:52) Okay. (4:53) Lipase is, that's just an indicator for the pancreas. (4:57) Is that right?
Lara (4:58) That's right.
Scott Benner (4:59) Yeah. (4:59) By the
Lara (5:00) way Those numbers are high.
Scott Benner (5:01) Oily stools, never something you want. (5:04) I don't care for what reason.
Lara (5:05) No. (5:05) But I was on a keto diet at the time too, so I kinda thought at the same time, maybe that was all related. (5:12) Like, it wasn't something and, initially, I didn't have any pain that started later. (5:17) So I didn't really think much of it, to be honest with you. (5:20) It kind of came and went.
Lara (5:22) Mhmm. (5:22) And in hindsight, really, there the warning signs were there from long ago, and that's kind of what I wanna bring attention to people to be really in tune with their body.
Scott Benner (5:33) If you take insulin or sulfonylureas, you are at risk for your blood sugar going too low. (5:41) You need a safety net when it matters most. (5:44) Be ready with Gvoke HypoPen. (5:47) My daughter carries Gvoke HypoPen everywhere she goes because it's a ready to use rescue pen for treating very low blood sugar in people with diabetes ages two and above that I trust. (5:59) Low blood sugar emergencies can happen unexpectedly, and they demand quick action.
Scott Benner (6:05) Luckily, Gevo Kypopen can be administered in two simple steps, even by yourself in certain situations. (6:12) Show those around you where you store Gevo Kypopen and how to use it. (6:16) They need to know how to use Gevo Kypopen before an emergency situation happens. (6:22) Learn more about why Gvoke HypoPen is in Arden's diabetes toolkit at gvokeglucagon.com/juicebox. (6:30) Gvoke shouldn't be used if you have a tumor in the gland on the top of your kidneys called a pheochromocytoma or if you have a tumor in your pancreas called an insulinoma.
Scott Benner (6:40) Visit gvokeglucagon.com/ risk for safety information. (6:47) Yeah. (6:48) No. (6:48) I'm my my I'm doing a little reading right here. (6:51) So lipase does not, correlate to pain, in case you're wondering.
Scott Benner (6:56) It doesn't. (6:56) It doesn't. (6:57) And it there is a a concern here. (7:00) Is is lipase, attached? (7:03) Does it mean diabetes, you know, for example?
Scott Benner (7:06) Mhmm. (7:07) And it does say that lipase elevation shortly precedes the onset of type one, but that's probably a thing nobody knows when it's happening, I would imagine.
Lara (7:16) That's right.
Scott Benner (7:17) Yeah.
Lara (7:17) And it's not something that they normally test for unless you're having issues. (7:21) So until you're already at the point where you're having some symptoms and some issues, that's when it look when they look for it. (7:29) And it was actually by chance, my doctor thought, oh, I shouldn't even check for this level because he had also had a patient recently just before me with the same issues. (7:39) So and that was her issue.
Scott Benner (7:42) Yeah. (7:42) I was wondering how they got to it so quickly, honestly. (7:45) Plus and I don't mean to be pejorative, but you're in Canada, so you it's a province coin flip whether you get good health care or not. (7:51) Right?
Lara (7:53) Is that ever the truth?
Scott Benner (7:54) And I
Lara (7:55) can tell you some nightmare stories that I've been through recently, actually, about that. (8:01) But in this case, in the very beginning stages, I was treated very well. (8:05) They were on top of it right away. (8:08) I had the proper scans and and everything. (8:11) It seemed to be going along pretty well.
Scott Benner (8:14) Mhmm. (8:15) But it was yeah. (8:17) Yeah. (8:17) So so what was the treat what was the initial treatment?
Lara (8:20) The initial treatment for me was hospitalization, clear fluids. (8:25) After a few days, I was on only IV fluids because they're they put you on digestive rest
Scott Benner (8:33) Mhmm.
Lara (8:34) Is really the only way to get past that. (8:36) And then by the time I left the hospital, I thought I was all good to go. (8:41) We'll check and see if maybe the gallbladder needs out later, but, I felt totally fine.
Scott Benner (8:48) Okay. (8:48) Was the gallbladder showing any indication, or was that just a thing they said we have to watch out for?
Lara (8:54) Gallbladder and pancreatitis go together very often. (8:59) And because they found that abnormality in the bile ducts, they were watching that, and that might have been the trigger where they would have pulled the gallbladder out if that hadn't resolved itself.
Scott Benner (9:10) And my last question is when they when you said they scanned your pancreas, was that ultrasound?
Lara (9:15) It was CT scan.
Scott Benner (9:16) CT. (9:17) Okay. (9:17) Thank you. (9:18) Sorry. (9:19) Go ahead.
Scott Benner (9:19) Keep you you left. (9:20) You thought you were good to go. (9:21) I'm sorry. (9:22) Keep going.
Lara (9:22) And then so they said come back in six months, and so that put it around February, my birthday of 2022. (9:31) And I was feeling fine and well. (9:34) They had scheduled me for a the follow-up CT scan, and I was expecting at the very worst that I would have to have gallbladder surgery. (9:44) No big deal. (9:45) But I got a phone call after that initial scan in February 2022, two days later, to come back in.
Lara (9:53) And I knew at that point that I was in trouble. (9:56) So at the second scan, they found a 1.4 millimeter mass on my pancreas. (10:03) It was very, very small, very, very early. (10:07) It had zero spread. (10:09) There was no indication of any real seriousness at that point.
Lara (10:16) They thought, no big deal. (10:18) We can get in there really quick, get it out without having any spread. (10:22) And I and I didn't have any symptoms. (10:24) They thought this this would be a curable thing for me.
Scott Benner (10:28) For clarity, you said it once, but I wanna make sure I repeat it. (10:31) The pain was gone. (10:32) Right?
Lara (10:32) Pain was gone. (10:33) I was totally fine. (10:34) I was actually very annoyed that I had to go in for this scan, because I had to take time out to do it, and it was a contrast dye one, which I don't really like doing. (10:45) And, I thought to myself, well, I was fine. (10:49) So why am I doing this?
Lara (10:51) But I did my due diligence, and thank God I did because it it was a a bad thing.
Scott Benner (10:57) Before we move forward Mhmm. (11:00) And you tell me about, you know, what they what they decided to do. (11:04) You mentioned this, but I wanna dig into it for a second. (11:06) You said hindsight's, like, I don't know if you used those words, but I thought, like, were there hindsight symptoms? (11:11) Where even for years before, did you have issues that you ignored or stuff that you, like, look back and go, oh, I think this was a thing?
Lara (11:21) The only thing I would say that I should have paid more attention to was the symptoms from the pancreatitis, which was the oily stool. (11:30) And I should have been on top of that, but I with the keto diet, I was I thought maybe I'm just not digesting well, which clearly I wasn't because there was issues there, and it was completely unrelated to the keto diet. (11:46) But it that also could have been something that triggered it as well.
Scott Benner (11:51) How long before and for how long did that occur before you got the lower back pain shooting to your shoulders?
Lara (11:58) I would say several months.
Scott Benner (12:00) Okay.
Lara (12:00) But not continually, off and on, not every day. (12:04) So I I I didn't really think anything of it. (12:07) Mhmm. (12:07) And that was silly on my part.
Scott Benner (12:09) So You know, honestly, Lara, probably not. (12:12) You know what I mean? (12:13) Like, because for every person who can say, I ignored this and it turned into cancer, there's a there's a million people Yeah. (12:21) You know what I mean? (12:22) Who are like, oh, I ignored it.
Scott Benner (12:22) Guess what? (12:23) Everything was fine. (12:24) So I I mean I know.
Lara (12:26) I guess that is the case.
Scott Benner (12:27) Yes. (12:28) Yeah. (12:28) Don't beat yourself up. (12:29) But but at the same time, it's it's great to know what to look for. (12:32) Also, I think it helps highlight that your pancreas has something to do with your digestion, and a lot of people don't know that.
Scott Benner (12:37) So But yeah. (12:39) Huge portion. (12:39) Mhmm. (12:40) Yeah. (12:40) Alright.
Scott Benner (12:41) Yeah. (12:41) Okay. (12:42) So they see this this little mass, and they're gonna try to take it out. (12:46) So what are next steps?
Lara (12:47) So the next steps are PET scan and biopsy. (12:51) I had the referral to a hep hepatobiliary oncologist surgeon who was confident that this was going to be a curable thing for me given that it was so small. (13:05) So PET scan showed, just this very same actually, it showed the same tumor, very small. (13:13) It also lit up my thyroid, which I had a thyroid nodule. (13:17) They said that was gonna be okay.
Lara (13:19) They would do a fine needle biopsy on that, but it would be unrelated to what I was dealing with with pancreatic cancer.
Scott Benner (13:26) Mhmm.
Lara (13:27) The biopsy was done, and it confirmed that we were dealing with invasive ductal adenocarcinoma, which is the worst kind of pancreatic cancer to have.
Scott Benner (13:39) Mhmm.
Lara (13:40) It spreads quickly, and it's quite aggressive. (13:43) But we were still confident that, with the surgery and then six months of chemo after the surgery was done, that I would have the cure that we were looking for. (13:54) So I went in very, very positive and confident that I was in good hands and that things would be a okay. (14:03) And I do wanna say that this was all extra scary for me because ten years ago, we lost my uncle to pancreatic cancer at 57.
Scott Benner (14:12) Really?
Lara (14:14) Yep.
Scott Benner (14:14) Yeah. (14:15) I have to tell you, Lara. (14:16) I don't I don't know if people know this. (14:18) I haven't said this in a while, but when I sit down to record, generally speaking, I don't really know what I'm doing. (14:24) I don't, like, I don't preplan my conversations, and I don't really look at my calendar.
Scott Benner (14:31) So you know how some people really wanna know what the weather is before they go outside? (14:35) More of a wander outside and see what the weather's like person. (14:38) And I and I do that with this too. (14:40) And I just wanna tell you upfront, I don't wanna slow you down. (14:43) But if I pause, I lost my mom to cancer, like, in the last year.
Scott Benner (14:48) And I'm having a more difficult time with this than I thought I would. (14:52) So don't I don't I don't wanna stop you. (14:55) We're definitely having this conversation. (14:57) But at some point, I'm gonna cry today, just so you know. (15:00) Like, let's just put
Lara (15:01) that out. (15:01) And I likely will too, and that's a okay. (15:04) Okay.
Scott Benner (15:04) Okay. (15:04) Good. (15:05) Good. (15:05) As long as we're both expecting it. (15:06) Yes.
Scott Benner (15:06) Yeah. (15:07) You just it just it took me by surprise a second ago, and I was like, I don't feel right. (15:11) Why do I not feel right?
Lara (15:12) It gets you.
Scott Benner (15:14) Everyone's got all the all the hope in the world. (15:17) Did you get a feeling like they really thought that or that they were just being positive? (15:22) The Dexcom g seven is sponsoring this episode of the Juice Box podcast, and it features a lightning fast thirty minute warm up time. (15:30) That's right. (15:30) From the time you put on the Dexcom g seven till the time you're getting readings, thirty minutes.
Scott Benner (15:36) That's pretty great. (15:37) It also has a twelve hour grace period, so you can swap your sensor when it's convenient for you. (15:43) All that on top of it being small, accurate, incredibly wearable, and light, these things, in my opinion, make the Dexcom g seven a no brainer. (15:52) The Dexcom g seven comes with way more than just this. (15:56) Up to 10 people can follow you.
Scott Benner (15:58) You can use it with type one, type two, or gestational diabetes. (16:01) It's covered by all sorts of insurances and, this might be the best part. (16:07) It might be the best part. (16:08) Alerts and alarms that are customizable so that you can be alerted at the levels that make sense to you. (16:15) Dexcom.com/juicebox.
Scott Benner (16:18) Links in the show notes. (16:19) Links at juiceboxpodcast.com to Dexcom and all of the sponsors. (16:23) When you use my links, you're supporting the production of the podcast and helping to keep it free and plentiful.
Lara (16:30) No. (16:30) I really did. (16:31) Because by all stretches of the imagination, this was found by accident. (16:35) It was found so early. (16:37) It was very small, almost at the point where it wouldn't even be something that would be detected.
Lara (16:43) It has to be a certain size before it can be detected on scans.
Scott Benner (16:46) Mhmm.
Lara (16:47) The cells can be caught in PET scan just floating around because they light up. (16:51) Like, they feed it they feed them sugar, and the cancer cells light up like a Christmas tree.
Scott Benner (16:58) Yeah.
Lara (16:58) But the actual tumors need to be big enough to be able to be found. (17:02) So this was just at the point. (17:04) It was so small. (17:06) Surgery. (17:07) There was going to be a distal pancreatectomy, which means they would have taken half of the pancreas and my spleen because those things are connected.
Scott Benner (17:16) Mhmm.
Lara (17:17) And by all searches of the imagination, they told me that the pancreas that was left over was going to take over the insulin production, and I wouldn't be a diabetic. (17:29) I would be fully cured and just had to get through this hard road for, well, six months surgery. (17:36) Well, recovery and then six months of chemo. (17:39) So they started the chemo six months after their full surgery.
Scott Benner (17:42) Right. (17:43) So you thought I'm getting a surgery, not much is gonna change other than I'm not gonna have cancer anymore. (17:48) And That's it. (17:49) Yeah. (17:49) Okay.
Scott Benner (17:50) So when did they tell you that's not what happened? (17:53) Is it, like, right when you woke up or Mhmm. (17:56) How does that go?
Lara (17:57) So my surgery was scheduled for 03/28/2022. (18:02) And on the March 25, I had my last CT scan before going into surgery, and I never saw the results of that. (18:09) And while I was being wheeled into surgery from the little holding room after I'd been laying there crying my eyes out scared as scared could be. (18:20) I met the surgeon for the first time face to face because this was still times where they were doing phone appointments, and I hadn't seen his face even. (18:32) So there he stood with me and told me that the tumor had grown in that six week time frame from one CT scan to the next from 1.4 millimeters to four and a half centimeters, and it had taken over the entire pancreas.
Scott Benner (18:50) Not good with the metric system, but that sounds like a significant increase.
Lara (18:54) Significant is right. (18:57) So it went from one tiny little dot in there to taking over the whole pancreas. (19:03) And at that point, he said there still haven't been any spread, but the likelihood that I was going to lose the entire pancreas was was pretty probable.
Scott Benner (19:14) Yeah. (19:14) For people, who like me who don't know the the metric system, that's about a 40 times gross or growth of of the mass.
Lara (19:24) Yes.
Scott Benner (19:24) Yeah. (19:25) It grew by, like, 40 times its size in six weeks.
Lara (19:29) That's right.
Scott Benner (19:29) Yeah. (19:29) That's
Lara (19:30) aggressive. (19:30) Saying invasive and aggressive
Scott Benner (19:33) Mhmm.
Lara (19:33) That it that it is. (19:35) So the importance of the early detection was astronomically important. (19:41) I I I can't even say because at this point, the surgery could the whole pancreas could still come out. (19:50) The cancer hadn't still spread at that point. (19:52) So there was a silver lining to that, although I was completely unprepared for what what I was going to find when I woke up.
Lara (20:01) So
Scott Benner (20:01) Yeah. (20:02) Yeah. (20:02) Yeah. (20:02) It's like it's like the opposite of Christmas. (20:04) You got two gifts instead of one.
Scott Benner (20:06) And usually, they were like, hey, guess what? (20:08) You have cancer and diabetes. (20:12) It's like you're like, I didn't have either of these things five minutes ago. (20:16) What the hell? (20:17) And and and so you're coming out of a surgery as a type one, basically.
Scott Benner (20:23) But it's type three. (20:24) Right? (20:24) Is it what they call type three c?
Lara (20:25) Type three c.
Scott Benner (20:26) Type three c. (20:27) You come out of surgery as a type a type three c and somebody telling you, hey, there's way more cancer in there than we thought. (20:34) And and that's all out of nowhere from and so for all the crying you did before, how does it No. (20:42) Yeah. (20:42) You do a little more after, I imagine?
Lara (20:44) So the surgery was nine hours when it was supposed to be, like, three and a half. (20:51) So that alone was a huge undertaking. (20:54) And I when I got to the Recovery Room, it was very late, and that's when they told me that I had lost my whole pancreas. (21:03) And I also awoke to nurses in sheer panic because they were unable to control my blood sugar. (21:11) So they kept me in the Recovery Room because they're got me on, in this point, insulin drip, which has to be done with one to one care.
Lara (21:20) And they're worried about DKA at this point. (21:22) And I don't even know what DKA is.
Scott Benner (21:25) You're not even awake, but you definitely don't know what it is. (21:29) Right? (21:29) Also, I take your point about the time, I remember we dropped my mom at, about eight or nine in the morning at the hospital. (21:38) During COVID, we couldn't even go. (21:39) My my, like, 70 at that point, 78 year old mother, I think.
Scott Benner (21:44) I think 78 or 79. (21:45) We basically wheeled her through the front door, gave her a good running push, was like, good luck, and then had to leave. (21:50) You know? (21:51) Like, because they wouldn't even let you come in with her. (21:54) Yep.
Scott Benner (21:55) Was frightening in in and of itself. (21:57) But the doctor said, I'll call like, my number was the one he was gonna call after the surgery was over. (22:03) And I'm not lying to you. (22:05) It was, like, 07:30 at night when he finally called me. (22:08) And he and he called to say, my assistant basically is still closing your mom up, but I'm done now.
Scott Benner (22:17) And I was like, wait. (22:17) This this like, I just figured the schedule got messed up or they lost her. (22:22) Like, seriously. (22:22) Because you could Yeah. (22:23) They because I we really did just kinda run through the door with the wheelchair and we're like, alright, mom.
Scott Benner (22:27) Like, well, good Good night. (22:29) Yeah. (22:29) And, like, I was thinking, maybe she's just sitting in a hallway somewhere, you know? (22:33) But, but instead, it took the better part of the day to do what they ended up having to do for the same reason because they got there and they were like, wow. (22:41) There's more here than we expected.
Scott Benner (22:43) So Yeah. (22:44) Yeah. (22:44) Yeah.
Lara (22:44) My family was completely unprepared because they were waiting at the hospital and at some point, they had to go home. (22:51) And I remember them my husband saying, yeah. (22:54) We got the phone call. (22:55) We were almost home. (22:56) And it was way late at night, and the surgeon called and told him, but I still hadn't spoken or seen any of my family.
Scott Benner (23:04) That sucks.
Lara (23:05) And listening to these nurses in panic about these things that I don't know about.
Scott Benner (23:12) They're like, hey. (23:12) We can't get our blood sugar under control. (23:14) And you're like, what? (23:14) That wasn't part of why I was here. (23:16) Like Right.
Lara (23:17) Yeah. (23:18) And then there's and I and I don't even know what numbers mean at this point. (23:22) Right? (23:22) So my sugars were at 25, and I don't know what
Scott Benner (23:27) Oh, I could tell you. (23:28) But I only after I go to a conversion chart on my website.
Lara (23:31) I have a conversion chart saved on my phone from the Juice Box podcast. (23:36) But
Scott Benner (23:36) Thank you. (23:36) 20 oh my god. (23:38) 25? (23:39) Wait. (23:39) Are you serious?
Scott Benner (23:40) Yeah. (23:41) Yep. (23:41) Oh, that's a four like, a four fifty blood sugar.
Lara (23:44) Yep.
Scott Benner (23:44) Yeah. (23:44) Yeah. (23:44) Okay.
Lara (23:45) For hours. (23:46) For hours and hours and hours. (23:49) And once they got them finally back down, I think it was about 01:30 in the morning is finally when I left recovery and then went up to the ward. (23:58) But I had had asked to call my mom because I just wanted my mom. (24:02) I just as you do Yeah.
Lara (24:05) I just needed her. (24:06) And so I had the phone call with her completely out of it, totally confused, and very angry.
Scott Benner (24:13) Yeah. (24:15) And angry for a Canadian. (24:16) What does that even mean? (24:17) Were you saying darn it?
Lara (24:20) Oh, I can get super angry.
Scott Benner (24:23) I always tell people, you know, you don't know about Canadians. (24:26) So people always say there's there's not as much gun violence in Canada. (24:28) I was like, but they love to stab each other, so don't go giving them too much credit.
Lara (24:32) And I also hear we're very sweary. (24:35) So Yeah.
Scott Benner (24:37) Well, I know for sure in bars, you're very stabby. (24:40) So Yeah. (24:41) Because
Lara (24:43) we can't get guns here. (24:44) Right?
Scott Benner (24:44) Well, I I I assume that's why it's happened. (24:46) Yes. (24:47) Yep. (24:48) So well, you reached for your mom. (24:50) Like, you skipped right over I I I don't mean this in a bad way.
Scott Benner (24:54) I I honestly don't. (24:55) But when you thought I need help, you didn't go to your husband. (24:58) You went to your mother.
Lara (24:59) I went to my mom, and I and I always do, especially with the medical stuff, because she she understands more. (25:06) My husband's a little bit more of a stress case when it comes to all of these things.
Scott Benner (25:10) Mhmm.
Lara (25:11) And I knew that he had my daughter with him, and I kinda didn't wanna get her involved at this point before I'd even figured things out. (25:20) And I think you always just I I do just reach for my mom.
Scott Benner (25:25) I just think that this highlights a mother's instinct on your part because if I was in trouble, I would drag everybody into my horror immediately. (25:34) I'd be like, I don't can't believe you people left. (25:37) Was like, I need everyone back here. (25:39) I want a vigil. (25:40) There should be candles, crying.
Scott Benner (25:42) I actually cry in shifts. (25:43) So every time I look up, I see somebody sad. (25:45) Why?
Lara (25:46) I went total opposite. (25:49) I went into, like, recluse mode. (25:52) I didn't want to see anybody Mhmm. (25:55) At all.
Scott Benner (25:57) Yeah. (25:57) Did you think you were gonna die? (25:59) Is that when does that occur to you the first time?
Lara (26:02) The first time it occurred to me that I might die was when I first got the first report with the that I had pancreatic cancer because, I mean, the Google tells you no one comes out of
Scott Benner (26:13) it. (26:13) Yeah.
Lara (26:14) And so I tried really hard and I did. (26:17) Probably to my dismay, actually, in the end, I stayed off the Google, and I stayed off all of the Facebook groups for pancreatic cancer because it was all nothing but doom and gloom. (26:31) And I wanted to stay positive because I knew mindset had something to do with it. (26:36) And I always felt that I was in good hands and that I should trust the people that were dealing with me in my situation and not the random strangers that have had a myriad of ex different experiences, some good, some terrible. (26:51) Right.
Lara (26:51) And I didn't know where I was gonna fit into all of that.
Scott Benner (26:55) I hear you.
Lara (26:55) So I didn't do a whole lot.
Scott Benner (26:57) You don't wanna jump into somebody else's story and put it on yourself when maybe you're not in the same position they're in.
Lara (27:03) Yes. (27:04) Yeah. (27:04) And especially since so many of those stories are not good.
Scott Benner (27:07) Right.
Lara (27:08) It was not a safe place when I was learning a whole new life at the same time.
Scott Benner (27:14) Yeah. (27:14) Yeah. (27:14) You make yourself crazy, I would imagine.
Lara (27:17) Totally.
Scott Benner (27:17) Yeah. (27:17) So okay. (27:18) So you're you're kinda locked down. (27:20) You're you got your mom. (27:21) What's your does your mom say anything valuable, or is it all just a lot of love?
Lara (27:25) It's just a lot of love because at this point, she didn't know what was gonna be valuable to say other than she was it was gonna be okay and that she would be there every step of the way, which she has been holding my hand every step of the way along this whole journey. (27:43) She's not left my side Yeah. (27:45) And has been an amazing support for all of us, my family included. (27:51) So we couldn't have done any of this without her.
Scott Benner (27:53) Did she get off the phone with you and latch up the dogs, take a a big cut of whale blubber and head right to you on her sled or how did did she stay where she was? (28:05) That's how you guys get around. (28:07) Right?
Lara (28:08) That's right. (28:09) Yeah.
Scott Benner (28:09) Yeah. (28:09) Yeah. (28:09) Right. (28:10) Yeah.
Lara (28:11) So she was there early the next morning. (28:14) So at one in the morning, I ended up back in my room, a room, which was nice. (28:19) I had a private room, which doesn't happen very often here in Canada. (28:22) They're usually a four bed ward room. (28:26) And given the nature of what I was going through, I appreciated that time where I was just alone and not having other patients in the room, but she was there.
Lara (28:38) And you almost had to kick her out to leave at the end of the day. (28:42) So I spent nine full days in the hospital recovering from the surgery. (28:47) The next day after the surgery, they'd sent in the the first endocrinologist that I was to meet. (28:53) And I sent her out the door as fast as she came in because I knew immediately she wasn't gonna be a fit for me.
Scott Benner (29:00) How come?
Lara (29:01) She came in so bubbly and squealing with her hair in a high ponytail, and she's talking to me like, life is good. (29:11) We have insulin. (29:13) And she was so trying to be this bubbly positive person, and I was just I'm like, I like the facts. (29:19) I don't need no, like, fluffy stuff. (29:22) Tell me where it is at.
Lara (29:24) Like, tell me what I need to know, what I need to do.
Scott Benner (29:27) You and Armen might get along really well because you I I like that the the most despicable part of her was her high ponytail. (29:34) I
Lara (29:35) I just couldn't. (29:36) I couldn't deal with her. (29:38) And and she just she came in. (29:40) She gave me a meter. (29:41) She gave me, and left the nurses a basic LARPEN.
Lara (29:46) That's what that's how that went down.
Scott Benner (29:48) You know what I was really surprised by earlier in your story? (29:51) You can't be the first person to go into surgery and come out without a pancreas. (29:55) Why were the nurses so thrown off by it in post op? (29:58) Because, obviously, you're not a person using basal insulin when you win in. (30:01) You have no insulin at all.
Scott Benner (30:02) Like, your body is, like, devoid of insulin. (30:04) And so Yep. (30:06) I'm not a doctor, Blair. (30:07) I just wanna be clear. (30:08) And if you took a person and handed them to me and said, hey.
Scott Benner (30:11) I just took this person's pancreas out. (30:13) My brain would go, well, we have to get basal insulin going right now. (30:17) I don't know why that's difficult. (30:19) Like like, you know what mean?
Lara (30:21) Know what? (30:22) I don't either. (30:23) But I do know that they don't do these surgeries very often, and I am one of the few that it does happen because, normally, these things are found too late for this to make a difference.
Scott Benner (30:35) Yeah. (30:36) Oh, they don't do the removal because it's over by the before it starts.
Lara (30:40) That's right. (30:40) Yeah. (30:40) Yeah.
Scott Benner (30:41) No. (30:41) Yeah.
Lara (30:41) That part I get, but when you're when you are in that one to one care recovery room, I mean, surely, you've had diabetics through there before.
Scott Benner (30:52) Mhmm.
Lara (30:53) You know how to deal with the one to one and the IV drip of insulin, but they were shocked and didn't know what to do.
Scott Benner (31:01) This so this endo that comes and sees you after the surgery, she wasn't meeting your energy. (31:05) Let's just say that. (31:06) Right? (31:07) Yeah. (31:07) Because your energy was, hey.
Scott Benner (31:08) I just found out I have way more I had way more cancer than I thought I did, and now I have diabetes on top of that. (31:14) And she came in like mister Rogers, and you were like, no. (31:17) We're not doing this. (31:18) Yeah.
Lara (31:19) That's right.
Scott Benner (31:19) Okay. (31:19) Yeah. (31:20) I understand, by the Mhmm. (31:22) So what what ends up happening then? (31:24) Like, you got your Basilagar pen, but what else did you get out of that?
Lara (31:28) So they never actually this this is this is I know you're gonna find this shocking, and I've heard because I've listened to the diet the the diagnosis stories on the Juice Box podcast. (31:39) They would come in at night and give me a shot of Basaglar. (31:45) They didn't explain to me what that was.
Scott Benner (31:47) Mhmm.
Lara (31:48) And then with my meals, as I could eat, because there was a a long period of time where I had just really any difficulty. (31:57) Because they removed part of my stomach as well. (31:59) So this surgery comes with gallbladder, spleen removal, part of your stomach, and your pancreas. (32:06) So they've reconnected it all.
Scott Benner (32:08) Why the stomach? (32:09) Was there cancer there?
Lara (32:10) There wasn't. (32:11) But just how the digestive tract works, they have to When they remove Yeah. (32:18) I see. (32:18) They make the stomach smaller.
Scott Benner (32:19) Okay. (32:20) The basal guards basal guards Lantus. (32:23) So that's your so they were giving you slow acting at night, but not telling you what it was. (32:28) They didn't say this is basal insulin or nothing. (32:31) Well, in in fairness, you did scare the lady away who might have told you that.
Lara (32:35) Well, she didn't she came in, and she wasn't even really prepared to give me any education or anything at that point. (32:42) I think they thought maybe too early, but, obviously, they didn't know me because I need to be armed with the facts, and I need to know what it is that I'm doing and how how like, how is this gonna work? (32:54) Like, you can't just come and shoot me up with something and then expect me to know what it is when this hasn't been a part of my life. (33:01) And it and I actually, truth be told, only know one other type one diabetic in my life. (33:07) So Yeah.
Lara (33:09) I didn't know.
Scott Benner (33:10) Right. (33:10) No. (33:10) Yeah. (33:11) You don't you you have no idea. (33:12) Did you say nine days in the hospital after that?
Lara (33:15) Yep.
Scott Benner (33:16) Nine days. (33:16) Okay. (33:17) Do you have any idea what you're doing diabetes related by the time you leave even? (33:23) One
Lara (33:25) night, I'm gonna tell you this because what no one told me anything about diabetes. (33:29) They would come in. (33:30) They would give me when I would eat, they would give me a a shot of insulin with my meal. (33:35) They would give me the Basaglar at night, but they didn't explain to me, like, how much or what would happen or whatever. (33:42) And I remember one night not knowing not knowing anything, and I I didn't feel well.
Lara (33:49) And if you know me, you have to I have to be near death to press that nurse call button because I just can't stand it. (33:55) And it was in the middle of the night, and I thought I'm gonna annoy all these people at this point. (33:59) I was in a four bedroom, and I was sweating and shaking. (34:06) And and I felt like I was running out of time. (34:10) I pressed the call button, and, of course, I had a low blood sugar.
Lara (34:15) I didn't know this was gonna happen to me. (34:17) They didn't tell me. (34:19) They said, oh, you have low blood sugar. (34:21) Drink this juice. (34:23) Okay?
Lara (34:23) But they didn't tell me this would keep happening either.
Scott Benner (34:26) You just thought, like, oh, they probably just got it wrong this one time. (34:29) This will never happen again.
Lara (34:31) Yeah. (34:31) They didn't tell me this was gonna be a regular, almost daily occurrence for me.
Scott Benner (34:35) It's so difficult to be prepared for the first time anything happens. (34:39) And this is gonna sound disconnected for a second, but I have a fairly healthy life overall. (34:45) Like, I'm a a pretty robust person. (34:47) We were cleaning the other day. (34:48) My wife and I did the very adult thing of cleaning our house one Saturday and just, you know, spent the entire day cleaning stuff.
Scott Benner (34:55) And I'm a boy, so she's downstairs doing what she's doing. (34:59) I just take bleach and cut it with water, put it in a spray bottle and just, like, douse everything and wipe it down and, like, hey, look, it's clean. (35:05) And, by the way, it works great. (35:07) But I was cleaning in a corner. (35:10) This is gonna sound ridiculous, but there's a toilet in the corner and a corner in the corner.
Scott Benner (35:14) And so I sprayed down the toilet and I sprayed down the floor and then I walked away and came back. (35:21) And I was in a room, obviously, with a fan that was drawing the air up from the ground. (35:25) And I turned back around to kinda go down onto my knees into the space to, you know, wipe everything up and do everything I was gonna do. (35:33) And I think between the the ceiling fan running and how much I had sprayed, I just bent down and took in a bunch of bleach in through like a breath. (35:42) And I felt it hit the back of my throat and then started going down by a sock, like, I don't I don't know how air works, but it was going down through my chest.
Scott Benner (35:52) And as it was going down, like, I I wasn't I couldn't breathe. (35:57) And I've never been in that situation before. (36:00) And so I'm wearing rubber gloves. (36:03) I'm holding stuff. (36:04) I have earphones in my ears.
Scott Benner (36:05) Like, you know what I mean? (36:06) Like and I I'm I'm like, uh-oh. (36:10) And I'm I'm like, okay. (36:11) I need to get like, I feel like I should drink something. (36:14) It's the only thought I have.
Scott Benner (36:16) I stand up immediately, schnaught, running out of my nose. (36:20) My eyes are watering crazy. (36:22) I'm coughing to try and I'm thinking, oh, god. (36:25) I'm I'm coughing. (36:26) At least I'm breathing.
Scott Benner (36:27) And I'm coughing and coughing. (36:29) And I'm trying to pull the gloves off because I don't have a cup and I'm gonna I know I'm about to, like, just take water, like Tom Hanks in one of those movies, and, like, throw it at my face and try to get some in my mouth. (36:39) What was that one when he was on the island castaway? (36:41) Then I'm, like I'm gonna, like, do that. (36:43) Right?
Scott Benner (36:43) And but I'm I have the wherewithal to think I have bleach on my gloves. (36:47) I have to take the gloves off. (36:48) But as I'm reaching for the gloves, I'm like, oh, I'm gonna die. (36:52) Like, the I am gonna fucking die cleaning the goddamn toilet. (36:55) That is literally what went through my head.
Scott Benner (36:57) I was like, son of a bitch. (36:59) I'm quasi famous. (37:02) This is gonna get around. (37:03) And, like, so I'm, like, I'm pulling on these gloves trying to get them off. (37:06) I'm trying to get the water running.
Scott Benner (37:08) And as I reach for the water, I think, water or milk? (37:11) I forget. (37:12) Is water bad? (37:13) Woah. (37:14) Is water gonna make it worse?
Scott Benner (37:15) And then I just had the thought. (37:16) Was, whatever. (37:17) I gotta clear it. (37:18) Like, so I just started, like, shoveling water at my face. (37:22) I got one good breath and I was like, help.
Scott Benner (37:26) Need help. (37:26) So I start heading through the house to get to Kelly. (37:29) And I'm like going down the stairs. (37:30) I'm like like hacking up like it felt like a lung was coming out. (37:34) But we've been married forever, so she ignores me all the time.
Scott Benner (37:38) So so like I'm coming down the stairs, I'm like, Kel, Kel, Kel, help, help. (37:44) She goes, what's going on? (37:46) And I'm like, all I wanna say is, you son of a bitch. (37:49) Like, what's going on? (37:50) I'm dying.
Scott Benner (37:51) Look at me. (37:51) Like, I agree. (37:52) And I'm like I'm like, blah blah blah. (37:53) So now I'm like running through the kitchen getting trying to get a glass so I can force down as much liquid as I can in between breaths and having that real panic feeling like my brain's gonna shut off because I don't have enough oxygen. (38:06) And I finally get it in and I'm standing there just dripping out of every hole on my face and, like, just dying.
Scott Benner (38:12) And she's like, what's going on? (38:13) And I was like, you were no help what so ever. (38:16) And I'm like What's up?
Lara (38:18) Oh, god.
Scott Benner (38:20) I was like, I was counting on you and you just stared at me. (38:23) But but but my point in telling the story, besides Laura, let's be honest, it's funny. (38:28) But besides telling It's it funny. (38:30) Yeah. (38:30) Besides telling it for that story, I was thrust into a situation I'd never been in before around my health and I barely held myself together.
Scott Benner (38:39) And I and I think I was in like, I was in real trouble. (38:42) And then she got put into a situation she had never been in before, and she kinda, like, just froze. (38:48) And so I'm picturing you a couple of days shy of learning that, you know, all this just happened with my pancreas and all this other stuff, you get a low blood sugar. (38:57) You must have been me standing at the sink. (38:59) You must have been like, I'd right?
Scott Benner (39:00) I don't know what is happening or what I'm supposed to do.
Lara (39:04) Yeah. (39:05) It never happened to me before in my life, and I wasn't expecting it. (39:08) Didn't know it was a thing for me, and I didn't know how to deal with it. (39:15) But drink this juice. (39:16) Yeah.
Lara (39:17) Everything will be fine.
Scott Benner (39:18) Well, let me just say this. (39:19) If more of you would click on the links for the advertisers, I could probably afford to hire a cleaner to come through once a month and do a deep cutting on the bathroom.
Lara (39:27) I will share it all. (39:29) Yeah. (39:29) I mean,
Scott Benner (39:29) you guys could probably save my life by supporting the advertisers better. (39:33) I'm not a person who pays to have things done around my house. (39:36) Like, I like, even my neighbors, like, somebody's cutting their lawn. (39:39) I'm like, can you just cut your own lawn? (39:40) And she's like, I'm 60.
Scott Benner (39:41) And I'm like, just get out there and do it. (39:43) You'll be fine. (39:43) I'm kidding. (39:44) But, I mean, if the podcast got big enough, I would get somebody to clean the bathroom. (39:48) Just so you all know, you could save my life by supporting the sponsors.
Lara (39:52) And that's it's an important thing.
Scott Benner (39:54) Well, for me for me, Lara, because I obviously don't know enough to, like, dilute the bleach better before I
Lara (40:00) use Oh, boy.
Scott Benner (40:02) Basically atomized
Lara (40:03) lessons we learned.
Scott Benner (40:04) Yeah. (40:04) I basically atomized bleach and then, like, sucked it up. (40:09) So anyway, I'm an idiot. (40:10) But anyway okay. (40:12) And by the way, what am I complaining to you?
Scott Benner (40:13) You have fucking cancer. (40:14) So Yummy. (40:17) Yeah. (40:18) We haven't gotten to the the the the truly horrific part of your story yet. (40:21) Okay.
Scott Benner (40:22) So your low blood sugar, they get you back up. (40:26) Does that make you think not even, like, this could happen again? (40:29) You're not even at that yet. (40:31) Yeah.
Lara (40:31) Because I didn't know. (40:32) Like, I I honestly hadn't a clue. (40:36) Because really at this point, nothing had been explained to me. (40:39) They just kept coming in, giving me insulin, feeding me, which was a difficult thing for me to do. (40:45) They're giving me insulin for meals that I don't know that I can eat.
Scott Benner (40:50) Yeah. (40:51) Yeah. (40:51) Just
Lara (40:51) And then even checking blood sugars, they would come in, poke my finger, but not really explaining. (40:58) They would say this is good or whatever. (41:01) I I mean, I honestly didn't know. (41:03) I had a meter they gave me, but they they didn't come with enough lancets or strips to do anything with. (41:11) Just one of the sample ones.
Scott Benner (41:12) Yeah. (41:13) Yeah. (41:13) Sample meter, ten ten strips in it. (41:15) Right? (41:16) Yeah.
Lara (41:16) Done. (41:18) So I I was just really relying upon the care that they were giving me, and I figured by the time I was gonna go home, I would have have been to a class of some sort. (41:30) I don't know. (41:30) What how does this even work?
Scott Benner (41:33) Apparently not well. (41:34) Good job, Gary.
Lara (41:35) I fired my I my oncologist or my endocrinologist, so I they had to find a new one for me, which they did. (41:44) Thank god. (41:45) It wasn't until my they're getting ready to send me home after this nine days in there. (41:51) And I said, but I don't know. (41:54) Like, what am I what do I do?
Lara (41:56) They still hadn't explained that to me. (41:58) So the endocrinologist came in and said, give yourself thirty five units of Blade Basaglar at night, four units of Admalog for breakfast and lunch, and six units of Admalog at dinner.
Scott Benner (42:12) Did they tell you to count? (42:14) Like, would they put you on a sliding scale or tell you to have a certain amount of carbs or anything like that?
Lara (42:18) Just eat like a diabetic plate. (42:21) Oh. (42:22) So my dad's a type two diabetic, so my mom's like, okay. (42:26) Well, you need to have, like, a little bit of carbs, lots of vegetables, and some protein. (42:30) So outside of that, I didn't know how to eat anything else.
Lara (42:34) I didn't know that I could give myself more insulin if I had a snack. (42:39) I didn't know any of that until I found your podcast. (42:44) No one taught me that.
Scott Benner (42:45) That's something. (42:46) I wonder if people in the medical profession hear that and are just ashamed.
Lara (42:50) Well, they should be because it is such a huge thing, and it is something that can, as you know, kill you in a second
Scott Benner (42:59) Yeah.
Lara (42:59) Or send you into DKA if you're not careful with with taking enough insulin at the right time. (43:07) Brutal.
Scott Benner (43:07) I'm assuming you're along with this because these meals were probably not properly covered by insulin at all. (43:12) I mean, he who even knows if that was the right amount of basil for you? (43:16) Right? (43:16) So Who knows? (43:17) Because 35 And I mean, I may I ask how much you weigh?
Lara (43:21) I was much heavier at the time.
Scott Benner (43:24) Okay.
Lara (43:24) But as you well know, cancer and all of this surgery and all, I the massive weight loss, very quickly then put me into a point where I was experiencing multiple lows through the night
Scott Benner (43:39) Yeah.
Lara (43:39) Because I was having too much at that point. (43:42) So I was I think at the end, I was down to twenty one units of bezaguars.
Scott Benner (43:48) I was gonna say. (43:48) Yeah. (43:49) Mhmm. (43:49) Did you have any situation where somebody who you kind of knew saw you one day and was like, oh my god, Lara, Ozempic? (43:55) And you were like, no.
Scott Benner (43:55) Cancer.
Lara (43:57) Pretty much. (43:58) Yeah. (43:58) Yeah. (43:58) I kept it all very quiet, actually. (44:00) I didn't tell anybody what was going on until until I started chemo, actually.
Lara (44:06) I I didn't let anyone in. (44:09) I was so in such a terrible state of mind. (44:12) I didn't let any other than my very close circle, no one knew what I was going through.
Scott Benner (44:18) Can you give me a little bit of color on why that was? (44:21) Like, what why did it seem important to you to keep it to yourself at first?
Lara (44:24) It seems silly now, but I felt like I was going to be judged for maybe having a bad lifestyle or I I don't know. (44:36) I think it was just also shocking for me too. (44:40) Like, even just saying the words out loud put me into a place where I didn't wanna be.
Scott Benner (44:46) Yeah.
Lara (44:47) And it's made it all more realistic, and I wasn't prepared to answer people's questions because, well, I really didn't know what was going on at that point for myself. (44:58) And trying to explain it all, I just wasn't ready for it all. (45:03) And then in the end, when I did tell everyone, the support and the outreach was astronomical. (45:09) And I probably should have done it sooner.
Scott Benner (45:11) Yeah. (45:12) Your worry, was you just imagined, really. (45:15) Yep. (45:16) Yeah.
Lara (45:16) 100%.
Scott Benner (45:17) Okay.
Lara (45:18) So when I left the hospital, I left the hospital with my one Basaglar pen and had to stop at the diabetes educator on the way home from the hospital where she gave me a sample of the Freestyle Libre. (45:35) A little schooling on how to inject, where to inject, may and then I stopped at the pharmacy for my Admolog pens, which I didn't have, needles, digestive enzymes, which is another something I have to take every day with everything I put in my mouth.
Scott Benner (45:54) Yeah. (45:55) Which ones do you use?
Lara (45:56) I use BioCase. (45:58) Okay.
Scott Benner (46:00) I use pure encapsulations, but I don't need it every time. (46:04) But I and I obviously don't have the same issue you do. (46:07) I might not even have an issue. (46:08) I don't even know. (46:09) I just know it helps.
Lara (46:10) That's all it's important.
Scott Benner (46:11) Yeah. (46:11) Yeah. (46:11) Honestly, like, I had a slice of pizza yesterday and I put the pizza on the plate and then I thought, where are those little pills? (46:20) Mhmm. (46:20) And I popped two in my mouth.
Scott Benner (46:21) I went with two because cheese and grease and Yep. (46:25) Boom. (46:25) I swear to you, I don't know that I eat pizza. (46:28) Like, any bloating or, no bloating, no gas, no unpleasant trip to the bathroom, you know, hours or days later, nothing like that. (46:36) And it's all just from this little tiny freaking, like, thing.
Scott Benner (46:39) It's amazing. (46:40) So but you need it because they took they took your pancreas, is a a huge part in in digestion.
Lara (46:47) Yes. (46:48) And and with pancreatic enzymes, there is either it's a fine balance. (46:55) Too little or too much have the same effect, and trying to find that happy medium sometimes is just impossible.
Scott Benner (47:03) What's the effect?
Lara (47:05) You get a serious diarrhea.
Scott Benner (47:07) Yeah. (47:08) That's what I thought you were gonna say. (47:10) Yeah. (47:10) Too much or too little, same same situation. (47:13) Yep.
Scott Benner (47:13) Gotcha. (47:14) Okay.
Lara (47:14) Which is fun. (47:17) Really, really fun.
Scott Benner (47:18) Yeah. (47:18) Make make you long for those oily stools.
Lara (47:21) Right. (47:22) I'll take that.
Scott Benner (47:25) Isn't it weird when
Lara (47:26) you draw your lines? (47:27) Life is full of grossness. (47:29) Let me tell you.
Scott Benner (47:30) That's what happens. (47:31) You bring the inside outside. (47:32) Yep. (47:32) Yeah. (47:33) Yeah.
Scott Benner (47:33) Mhmm. (47:33) Okay. (47:34) So you've alluded to this a couple of times, but you really wait. (47:37) Wait. (47:37) I haven't let you dig into it because I'm in I'm trying to be modest.
Scott Benner (47:41) But the podcast helped you with your diabetes care, like, in totality? (47:46) Like, this is it. (47:48) This is where you learned about it. (47:49) Okay.
Lara (47:50) 100%. (47:51) I taught I took what they told me at the diabetes educator. (47:55) I threw it out the window. (47:57) I've only actually had one appointment with my endocrinologist since the fall went down. (48:04) I managed myself and learned to be bold and brave with the insulin so that I wasn't getting the huge spikes that I had, but it was the episode where Jen her name is Jen.
Lara (48:18) She had a total pancreatectomy as well. (48:21) She was actually my gateway in the Google search for finding like people like me. (48:28) Wow. (48:28) And that's how I found it and haven't stopped listening since.
Scott Benner (48:32) Let me tell you. (48:33) I I I mentioned earlier that there's something I have to tell you. (48:35) Right? (48:36) Mhmm. (48:37) Yesterday, I mean, I have a fairly robust, Facebook group.
Scott Benner (48:41) And I I forget, I posted something yesterday and someone a lot of times, people use my threads just to find me, which is smart because tagging me at this point is it it's difficult. (48:51) I I have trouble seeing all my tags. (48:53) She just asks out of nowhere, have you ever had somebody on with, t three c? (48:59) And I thought I definitely have. (49:01) Like, I thought of Jen right away, but what I but then what I thought was and I'm about to sit down with somebody who I think has it because this was, like, literally, like, two hours ago that I saw this post And I thought and I had looked at my I did I did brush my eyes over my my calendar this morning, like, as I was getting ready to sit down to do this.
Scott Benner (49:20) And so I'm, like, sitting here answering messages and at the same time setting up the file for you. (49:24) And I'm basically I open up my calendar to, like, put your name in the file. (49:28) And I saw it and then what struck me was it said, what's your connection to diabetes? (49:34) And it said other. (49:35) And I was like, other?
Scott Benner (49:36) What does that mean? (49:37) And I scrolled and then I saw, I am a pancreatic cancer survivor. (49:42) And then I saw all your notes and I was like, And so then I I finished responding to the person online and I said, and ironically, I'm interviewing someone today, like, who has it? (49:52) Like, you know, who has this situation. (49:54) And that's incredibly odd because people do not ask me about it with any frequency.
Lara (49:59) Timing is everything.
Scott Benner (50:00) Really insane, I thought. (50:02) So Mhmm. (50:03) Yeah. (50:03) So okay. (50:04) So you found Jen's, which is hers is just called type three c.
Scott Benner (50:08) Right? (50:09) Let me see if I
Lara (50:09) can find I think it says Jen Jen has no pancreas.
Scott Benner (50:13) Oh, yeah. (50:14) I do name things like a four year old. (50:15) Hold on a second. (50:16) It's not my fault. (50:19) I was not well educated.
Scott Benner (50:20) I was not well educated. (50:22) I don't have a lot of big words at my disposal. (50:25) Let's see. (50:27) Yeah. (50:27) Let me see if I can find it.
Scott Benner (50:28) I'll tell people what episode it is. (50:30) Okay. (50:30) What do we got here? (50:31) Pre owned pancreas, owner of a useless pancreas, two artificial pancreas studies. (50:36) You too can build an artificial pancreas, Kelly's bionic pancreas.
Scott Benner (50:40) I wait. (50:41) Was that not it? (50:42) Was pancreas not in the word in the title?
Lara (50:46) I thought it was.
Scott Benner (50:47) Hold on. (50:48) Jen had a pancreatectomy.
Lara (50:50) That's it.
Scott Benner (50:52) Episode two seventy nine. (50:54) There it is, if you wanna hear that. (50:56) Wow. (50:56) That was years ago. (50:58) Oh my god.
Scott Benner (50:58) I've been doing this forever. (50:59) How about that?
Lara (51:00) Mhmm.
Scott Benner (51:00) 2019. (51:01) Okay. (51:02) Well, then it was about time we had somebody else on to share their story. (51:04) So that's that's really it's great of you to do. (51:06) You you mentioned before we started recording today that this is out of your wheelhouse, like, being on the podcast, but you just wanted to Yep.
Scott Benner (51:13) To help other people.
Lara (51:15) I do. (51:15) I I have an innate desire to help people. (51:18) It's just who I am, and and I think that with this platform and the things that I've gone through, there is a lot of help or support or hope or whatever can be offered. (51:33) And for people that are going through this, that is everything.
Scott Benner (51:38) Yeah. (51:39) So once the surgery is done and you kind of, you know, you find the podcast and you figure out how to take care of your blood sugars and everything, how what's the length of time it's been from, well, I guess, first from the surgery. (51:50) How long it's March 2021 was the surgery. (51:53) Is that right?
Lara (51:54) It was March 2022.
Scott Benner (51:57) 2022. (51:57) Excuse me. (51:58) Okay. (51:58) So that's a year and, more than a half ago
Lara (52:02) Yeah.
Scott Benner (52:03) For the surgery. (52:04) And you did the six months of chemo.
Lara (52:07) I did.
Scott Benner (52:08) At the end of chemo, you rang the bell. (52:11) They told you were clean, the whole thing?
Lara (52:14) The whole nine yards. (52:15) Yep. (52:15) Totally clean. (52:16) Scans were clean. (52:18) There was no sign of cancer.
Lara (52:22) And because I didn't do my research and I stayed off the Google, I didn't realize that this is something that recurs even. (52:30) Like, they told me my margins were clear. (52:32) Everything was good there. (52:34) Everything they took thirty two lymph nodes as well. (52:37) They were all clear.
Lara (52:38) So after the six months of really strong chemo, which also that chemo, I will tell you, is infused in sugar water over forty six hours, which is good for diabetic.
Scott Benner (52:55) Yeah. (52:55) You had the bolus for chemo?
Lara (52:57) Mhmm. (52:57) Bolus chemo, and they said keep your try and keep your sugars at 10. (53:02) Okay. (53:03) Well, 16 to 22 was the average over those three days
Scott Benner (53:07) Mhmm.
Lara (53:07) Of chemo.
Scott Benner (53:09) Hey. (53:09) Did you get the bone pain after chemo? (53:12) Yeah. (53:13) Did anything help it?
Lara (53:17) I take, like, a Tylenol three.
Scott Benner (53:20) Uh-huh.
Lara (53:20) Mostly, it bothers me at nighttime. (53:22) It gives me restless legs, and the bone pain in my legs is is pretty bad. (53:27) So codeine, Tylenol codeine, helps with that.
Scott Benner (53:31) Did they give you anything for the restless leg besides the codeine?
Lara (53:34) No. (53:35) And I've had restless legs for years off and on, but it just gets exacerbated like crazy on chemo nights. (53:42) It makes chemo nights are impossible to sleep just from the jiggly legs and the pain.
Scott Benner (53:47) There's a medicine that helped my mom with the legs. (53:50) I'll ask my brothers and see if I can get you an answer. (53:54) Cool. (53:56) Oh, shit. (53:57) Laura, I'm sorry.
Scott Benner (53:58) Yeah. (54:00) So I'm sorry. (54:01) So you did the chemo, and it was really aggressive, and you're clean margins, but you didn't know that it has a a likelihood of coming back. (54:09) They didn't tell you?
Lara (54:10) They didn't tell me this. (54:11) There was zero discussion of reoccurrence.
Scott Benner (54:14) Yeah. (54:14) They told my mom, like, this is an aggressive cancer you have, but, you know, it's, you know, it's here in your ovaries and we're gonna take all that out. (54:22) Like, my mom got a whole hysterectomy. (54:24) Right? (54:24) So
Lara (54:25) Mhmm.
Scott Benner (54:25) We're gonna take all that out and you're clean and blah blah blah. (54:28) And, but then nobody really said anything about, like, but it could come back. (54:33) And it was crazy because ovarian cancer eventually takes my mom, but shouldn't have ovaries anymore. (54:42) So if you're a lay person, you think that doesn't make sense. (54:44) Like, you know what I mean?
Scott Benner (54:45) Like, how how could I have finger cancer if my fingers are gone? (54:48) But turns out Yep. (54:50) You can. (54:50) Right. (54:51) So Mhmm.
Scott Benner (54:52) Are they tracking you? (54:53) Did you get markers or symptoms? (54:55) How did you know that there was a recurrence?
Lara (54:57) So in July, I had my first scheduled follow-up. (55:03) So they were the plan for me was to do scans and blood work every six months for three years and then yearly after that for two years. (55:14) So July was my first six month follow-up. (55:18) And because of our beautiful free medical system here in Canada, my CT scan that should have occurred in July actually wasn't scheduled until the September. (55:29) But I went for the blood work, and they were tracking my CA nineteen nine tumor marker.
Scott Benner (55:37) Yeah.
Lara (55:37) And when I got that result, because we can check those lab results on yourself, I was sitting at home that day I had had this test done, and my tumor marker came back at 1,823, and normal is under 27.
Scott Benner (55:56) And they gave you a scan. (55:57) They couldn't find any masses, but they tell you we're gonna track the marker, and we're gonna go back to chemo. (56:02) Is that about the plan?
Lara (56:04) So they put they put in a request to get the scan done in a stat manner, and I ended up having to pay for a private PET scan because I couldn't get one done in a timely manner here. (56:16) And I was gonna have to drive four hours to get it. (56:20) And I don't know if you noticed that with a PET scan, you have to be off all insulin for six hours before a PET scan. (56:27) Oh. (56:28) And when you are insulin dependent, that's a feat in itself.
Lara (56:34) It has to be below 10. (56:37) Your sugars have to be below 10.
Scott Benner (56:39) But without insulin?
Lara (56:40) Without insulin.
Scott Benner (56:41) So you what? (56:42) You just starve yourself? (56:44) Yes. (56:44) Yeah.
Lara (56:45) Pretty much. (56:45) So I did I did it, but I thought driving four hours do that. (56:49) I I wasn't gonna do it.
Scott Benner (56:51) So we
Lara (56:51) paid to have a private PET scan done, which showed spread. (56:57) So I have no pancreas, but the pancreatic cancer cells were showing, on my liver, kidneys, and lymph node. (57:07) But there there was three masses that they could see on my liver.
Scott Benner (57:11) So they could see masses already. (57:13) How long ago was this?
Lara (57:15) This was in July.
Scott Benner (57:17) Four months ago. (57:18) Yeah. (57:20) Well, first of all, you're not nearly the only Canadian I know who can't get in for simple testing. (57:26) You know So there's an argument to be made like, yeah, health care is really expensive in America. (57:31) But at the very least, if you're waving cash around, somebody will see you.
Lara (57:35) Yes.
Scott Benner (57:35) You know, like so, you know, I have insurance. (57:38) There's someone to bill. (57:39) Oh, we can get you in. (57:41) But in Canada
Lara (57:42) Yeah.
Scott Benner (57:42) I think I know this to be true from people's personal experiences. (57:47) They basically it's whoever's gonna die first is at the top of the list. (57:51) So you That's right. (57:52) Right. (57:52) So you could have a problem that isn't, you know, imminent And you could you could end up waiting a year or more to get treatment for it.
Scott Benner (58:01) And that's not not not uncommon from what I understand.
Lara (58:04) It's not uncommon at all.
Scott Benner (58:06) Yeah. (58:06) Some provinces are apparently better than others where I guess, again, I should say province. (58:11) But you don't know you sound like that. (58:12) Right? (58:12) It's just that that you you have no idea.
Scott Benner (58:14) And so that's okay. (58:16) Oh, yeah. (58:17) Yeah. (58:17) So you get put in that so they would have killed you if you didn't pay for the PET scan.
Lara (58:22) That's right.
Scott Benner (58:23) And you ran the risk of your sled dogs being picked up on the scan by mistake. (58:27) You had because you had to go yeah. (58:29) Right. (58:29) Right. (58:29) I understand what's going on up there.
Scott Benner (58:30) Don't don't you worry. (58:31) And the Bob and the Snowman and all the stuff you guys have. (58:33) Yep. (58:34) So oh my god. (58:35) So yeah.
Scott Benner (58:36) Like, let's really think about that for a second. (58:38) If you would've waited on their schedule, all these masses are growing the entire time.
Lara (58:44) That's right.
Scott Benner (58:45) Oh, there's no way you would have lived. (58:46) Yeah.
Lara (58:47) When I finally got in for my provincially paid for CT scan, it took seventeen days for it to be read by a radiologist.
Scott Benner (58:57) Oh, that's not bad. (58:58) Just seventeen?
Lara (59:00) Just seventeen. (59:01) What the Shows cancer, but seventeen days before it was read by a radiologist.
Scott Benner (59:07) No kidding.
Lara (59:08) I already knew that I had cancer because the PET scan told me this. (59:14) And but and the blood blood work showed me this. (59:17) But then the oncologist wouldn't go by my private PET scan, and they were waiting for the CT scan result.
Scott Benner (59:24) Really? (59:25) They wouldn't look at the scan you had done?
Lara (59:27) No. (59:28) We had to hand deliver the images and the reports to them for them to put in the file, but they were waiting for the CT scan. (59:36) We had to drive an hour to the facility, get a CD ROM disc or whatever. (59:42) I remember the name.
Scott Benner (59:44) Go ahead. (59:44) Yeah. (59:44) Yeah.
Lara (59:45) Old school. (59:46) Deliver it. (59:46) Hand deliver it to the BC Cancer Center.
Scott Benner (59:49) Someone just had me fax something for, an insurance thing, and I said, am I sending it to 87? (59:55) Like, what are we doing? (59:56) I can't I can't just send you a PDF? (59:58) And they're like, no. (59:58) No.
Scott Benner (59:58) No. (59:59) I was like, why? (1:00:03) Does anyone ever stop and wonder why? (1:00:06) Like, like,
Lara (1:00:06) there's I ask these questions all the time.
Scott Benner (1:00:09) And by the way, at least, you know, a handful of years ago, Trudeau was at least handsome. (1:00:14) Now he's a little chubby. (1:00:15) So you're not even getting anything out of that anymore. (1:00:18) You know? (1:00:18) Nope.
Scott Benner (1:00:19) Canada. (1:00:20) I'm shaking my hand to Canada. (1:00:22) And you got all that stuff.
Lara (1:00:23) Oh, I am. (1:00:24) Yeah. (1:00:25) I'm shaking my head every day too. (1:00:27) Like, what the actual
Scott Benner (1:00:29) So Larissa, I'm sorry. (1:00:30) So this doesn't sound positive. (1:00:31) So, I mean, obviously, chemo and and in I guess you're getting infusions to shrink, swell. (1:00:37) Yeah. (1:00:38) Right?
Lara (1:00:38) I am. (1:00:39) So I I've opted for a few things, and I do have some positive I do have some positivity to talk about because I am doing very, very well. (1:00:49) So I have started on gemcitabine, Abraxane combination chemo, which is different from the first chemo. (1:00:56) They told me that the first time, the cancer cells have already seen this drug or these drugs. (1:01:03) It was a four dose combination, and they're still here.
Lara (1:01:07) So I opted to try something different, which is not the first line treatment. (1:01:11) It's second line. (1:01:12) So it is working well for me. (1:01:15) My recent scans show that there is delineation. (1:01:21) There is shrinkage.
Lara (1:01:24) There is no evidence in the kidneys any longer.
Scott Benner (1:01:29) Oh, wow.
Lara (1:01:30) The liver masses, the three of them, they are shrinking and delineated. (1:01:34) So I'm also along with what I'm doing, the chemo, I'm doing high dose vitamin c infusions and hyperthermia treatments along with a million supplements, through a naturopath, which they
Scott Benner (1:01:49) Are you doing cold plunge or you're just walking outside?
Lara (1:01:51) I'm actually the hyperthermia is not cold plunging, although I have considered it. (1:01:57) I haven't done it yet. (1:01:58) I'm a little bit of a chicken.
Scott Benner (1:02:00) Larry, you have cancer.
Lara (1:02:01) Don't think
Scott Benner (1:02:02) there's anything left to be afraid of.
Lara (1:02:05) True.
Scott Benner (1:02:06) Yeah. (1:02:06) Yeah.
Lara (1:02:06) The hyperthermia is where they heat the tumor. (1:02:09) So tumors, cancer can't live anything over 40 degrees.
Scott Benner (1:02:13) Oh, you you said hyper, not hypo. (1:02:15) I'm sorry. (1:02:16) Hyper. (1:02:16) Okay. (1:02:17) That's
Lara (1:02:17) okay. (1:02:18) So, yep, hyperthermia. (1:02:19) So I it's targeted treatment. (1:02:21) So I lay in this water bed type thing, and then they have a panel that goes over top of you, and it sends heat up and down. (1:02:30) So it heats the tumors, which then help the die off.
Lara (1:02:34) So you do that the day after you do chemo and then the day after that, so two days in a row, along with high dose vitamin c infusions Mhmm. (1:02:44) By IV.
Scott Benner (1:02:45) And this is being provided by Canada or you're No. (1:02:49) No. (1:02:50) I gonna say you're paying for this yourself. (1:02:51) Right?
Lara (1:02:52) Yeah. (1:02:52) It's $655 for one treatment.
Scott Benner (1:02:57) Jesus. (1:02:59) So I did cry in case you're wondering. (1:03:01) When you said the tumors were shrinking, it made me cry. (1:03:04) You you got me.
Lara (1:03:05) Thank you.
Scott Benner (1:03:06) Yeah. (1:03:06) Yeah. (1:03:06) Yeah.
Lara (1:03:06) So I've been told that one third of pancreatic cancer patients risk don't respond to treatment. (1:03:14) One third respond moderately. (1:03:17) One third respond well, and I am in the third of that third that are responding exceptionally well.
Scott Benner (1:03:24) Oh, good for you. (1:03:25) That's well that's lovely. (1:03:27) And I have a
Lara (1:03:27) So I'm determined.
Scott Benner (1:03:28) Well and maybe I have an answer for you. (1:03:31) My brother sent me the answer. (1:03:32) So rope in a roll, but it's commonly known as Requip, and it's a Parkinson's and, restless leg drug. (1:03:42) So Perfect. (1:03:43) R e q u I p.
Lara (1:03:46) Okay. (1:03:46) I'm gonna look into that. (1:03:47) I'll ask about that because it's brutal.
Scott Benner (1:03:50) We tried a number of different things to help my mom. (1:03:52) My mom was like, mom was doing some, like, drugs at the you know, for the for the restless leg and the bone pain at one point. (1:03:59) And we just kept pushing and pushing and, Requip was one of the things that actually helped her.
Lara (1:04:04) Cool. (1:04:05) That's good to know.
Scott Benner (1:04:06) Yeah. (1:04:06) I hope
Lara (1:04:06) I like to hear that.
Scott Benner (1:04:07) Meanwhile, you're gonna have to call a doctor, then they'll they'll return your call in seventeen days. (1:04:12) And then Right. (1:04:13) You'll mention that you heard it on a podcast. (1:04:14) They'll say, I'm sorry. (1:04:15) We have to do our own testing.
Scott Benner (1:04:17) And then they'll give you an appointment for nine years from now, and your legs should stop shaking about the time that you die of natural causes in your nineties. (1:04:24) So that'll be perfect. (1:04:25) Yeah.
Lara (1:04:25) Oh, you've got this Canadian medical system down pat.
Scott Benner (1:04:28) But it's free.
Lara (1:04:30) I know. (1:04:31) Right?
Scott Benner (1:04:32) You know why it's free? (1:04:35) It sucks. (1:04:36) It's not worth any money. (1:04:37) Yeah. (1:04:38) Yeah.
Scott Benner (1:04:38) You should live here because people still bring up Canada. (1:04:41) They're like, oh, it's free in Canada. (1:04:42) I'm like, have you ever spoken to a Canadian? (1:04:45) Oh,
Lara (1:04:46) the Americans, especially with pancreatic cancer, are so far ahead of the game and standards of care. (1:04:55) It's unbelievable the things that can happen down there in these big medical centers. (1:05:00) I if I was rich, man, I would be down there, and I'd be getting a nano knife surgery, and you name it. (1:05:06) I would get it all.
Scott Benner (1:05:07) Right. (1:05:07) I mean, there's no listen. (1:05:08) There's no doubt. (1:05:09) It varying degrees of of, you know, everything that the luck of the draw of where you're born and how much money is in somebody's pocket is a lot to do with the kind of care you get. (1:05:20) And it you can, you know Mhmm.
Scott Benner (1:05:21) You can whine and complain all you want that it's unfair, but, that's how the world works. (1:05:25) And it Yep. (1:05:26) It's what it is. (1:05:27) So that really is
Lara (1:05:29) Advocate. (1:05:29) Advocate. (1:05:30) Advocate. (1:05:31) That's all you can do.
Scott Benner (1:05:32) Yeah. (1:05:32) You gotta keep arguing. (1:05:33) That's for sure. (1:05:34) I have found recently Jenny and I are doing a series that is aimed at doctors. (1:05:38) I keep being upset by the word advocate because I know what it the intention of it doesn't exactly match the reality of it.
Scott Benner (1:05:46) Like, people are like, you have to advocate for yourself which means like, you you know, which should mean what? (1:05:52) Like, you know, don't you you're asking for things you should just have anyway and that they should give you an so you're telling me like, have to talk you into doing your job more completely? (1:06:02) Like, that's Mhmm. (1:06:03) Like, I I need to understand what I need medically or else it won't happen? (1:06:08) Yep.
Scott Benner (1:06:09) And then, by the way, when I bring it up, you're gonna yell at me and tell me not to look at the Internet. (1:06:13) How the hell do you want me to understand this? (1:06:15) Like, you're telling me you either know and won't do it or don't know. (1:06:20) Either way, I'm not comforted by that answer. (1:06:23) And so I That's right.
Scott Benner (1:06:24) Come to you and push you to do more, but I I need information about what that means. (1:06:29) So I go to the Internet, so I turn to you and I go, hey. (1:06:31) Look. (1:06:31) I read online. (1:06:32) You go, oh, I read online.
Scott Benner (1:06:34) You're like, wait. (1:06:34) What? (1:06:35) Like, so so you know you know what I mean? (1:06:38) So I I don't know. (1:06:39) It's upsetting.
Scott Benner (1:06:39) The seriously, the word just keeps pissing me off because I don't think it should have it shouldn't exist. (1:06:43) You know what I mean?
Lara (1:06:44) It's you shouldn't have to. (1:06:46) I actually have two oncologists. (1:06:48) One that my one that I started with and the one that I was re referred back to. (1:06:54) And, apparently, he's very brilliant. (1:06:57) But trying to have a conversation with him, like, I'm very real.
Lara (1:07:01) I like to ask questions. (1:07:03) Unless he's read it in a textbook or it comes out of a textbook, he can't have an off the cuff conversation about anything. (1:07:10) So I have found a second oncologist who's teaming up with him that's my real talk guy. (1:07:18) And he I can ask him stuff. (1:07:20) I he's the one who gives me the positivity and the good notes and the and the high fives, whereas the other one basically looks at me and says, well, we can't cure you.
Lara (1:07:29) We're just prolonging your life, and this is how it's gonna be. (1:07:32) And this other guy is like, we're gonna get you into some clinical trials, and I've talked to this other specialist. (1:07:38) So the help is there. (1:07:40) Unfortunately, you really do have to look for it yourself.
Scott Benner (1:07:43) Yeah. (1:07:44) No. (1:07:44) That's exactly right. (1:07:45) And that advice and experience clearly translates back to managing diabetes. (1:07:52) And Mhmm.
Scott Benner (1:07:53) You know, like, if people are like, oh, god. (1:07:54) He's talking about cancer. (1:07:55) It's a diabetes podcast. (1:07:56) What are we doing? (1:07:57) It's all very specific to just helping yourself.
Scott Benner (1:08:00) Yep. (1:08:01) If you take what someone tells you, you are very frequently not gonna end up well. (1:08:05) Like, you know Nope. (1:08:06) I I don't know if you've heard me talk about this in the podcast, and I am gonna try to get through this real quickly. (1:08:11) My mom only got the surgery to remove her cancer because my neighbor's son grew up to be a surgeon.
Scott Benner (1:08:19) And he went to medical school with a girl who eventually ended up in OB oncology. (1:08:25) And so I could ask my neighbor if it was cool if I texted his son. (1:08:30) When I texted his son, I said, is there any chance you know somebody that could be helpful with this? (1:08:34) Because the oncologist my mom has seen will not help her. (1:08:37) Like, he was talking about, like, just hospice and, you know, blah blah blah.
Scott Benner (1:08:42) My mom got two more years. (1:08:43) And instead, he was just gonna manage her into the ground
Lara (1:08:47) Mhmm.
Scott Benner (1:08:47) Over the idea that he he said, I'm not gonna kill your mom in surgery, which my neighbor's son told me translates to, hey, his hospital keeps score. (1:08:59) And if someone dies in his surgery, his score goes down. (1:09:02) And I was like, are you serious?
Lara (1:09:05) Because that's the important stuff.
Scott Benner (1:09:06) Right. (1:09:06) Right. (1:09:06) Right. (1:09:07) And so I'm like, okay. (1:09:08) So he's like, don't worry.
Scott Benner (1:09:09) I know a girl from med school. (1:09:10) So he calls his girl. (1:09:12) That girl's like, oh, yeah. (1:09:13) I work for this guy. (1:09:14) He's amazing.
Scott Benner (1:09:15) And two days later, my mom and I are sitting in an appointment and the guy is scheduling her surgery.
Lara (1:09:20) Amazing.
Scott Benner (1:09:21) But my neighbor's kid grows up and does something different, my mom dies two years earlier. (1:09:25) That is not an over exaggeration.
Lara (1:09:27) And that's not acceptable.
Scott Benner (1:09:29) Yeah. (1:09:29) Is that how this is all supposed to work? (1:09:31) Like, right? (1:09:32) I'm lucky because my I don't know. (1:09:36) That's ridiculous.
Scott Benner (1:09:37) By the way, the guy on the other side's kid is an engineer. (1:09:40) So I guess, good thing I bought on this side of the street. (1:09:44) Like, do you know what I mean? (1:09:45) Like Yeah. (1:09:46) How is it that random?
Lara (1:09:48) It's ridiculous. (1:09:49) Oh, jeez.
Scott Benner (1:09:50) You guys are you guys are right now like, Scott, one of your neighbor's kids is an engineer, the other one's a surgeon. (1:09:54) Your your son's got a quantitative econ Where the hell do you live? (1:09:58) I'm in a castle. (1:09:58) Okay? (1:10:00) A castle.
Scott Benner (1:10:01) Yes. (1:10:01) The freaking point is, what the hell?
Lara (1:10:04) Yeah. (1:10:04) I have fought my way through everything. (1:10:06) I fought, I have fought, I fought, I fought for myself. (1:10:10) And and even when it comes down to diabetic technology, like, I they made me wait a year before I could get the Omnipod. (1:10:17) I asked to switch to the Dexcom.
Lara (1:10:19) Like, those are all things that I took control over myself. (1:10:24) Yeah. (1:10:24) And and forced the issue because they would've just let me keep going at status quo, and I know there's better.
Scott Benner (1:10:32) Yeah. (1:10:33) Listen. (1:10:33) People die. (1:10:34) Okay? (1:10:35) And some people don't have great care, and that's a fact of life.
Scott Benner (1:10:40) But what you need to understand is that the people you're talking to, they try very hard to see you as a person, but honestly, you're a drop in a stream. (1:10:52) Yep. (1:10:52) And when you look at a stream, you don't see droplets of water. (1:10:55) You see water rushing by. (1:10:57) And so if you wanna be treated like a special drop, you need to take care of yourself because everyone else is just at work doing their best.
Scott Benner (1:11:05) You know what I mean? (1:11:06) Like, I I don't listen. (1:11:07) You if you have a really nice car and you take it in for new tires and it gets scratched later, they didn't see your really nice car and think like, oh my god. (1:11:14) It's a Mercedes. (1:11:15) I should try harder.
Scott Benner (1:11:16) They they they got 50 cars they gotta change tires on today. (1:11:20) That's that. (1:11:20) And this this whether you wanna hear it or not, medicine's exactly the same way. (1:11:25) It's just
Lara (1:11:25) like Totally.
Scott Benner (1:11:26) And it's not that they're bad people. (1:11:27) They're not bad people. (1:11:28) They're fantastic people. (1:11:29) They went to college for ten goddamn years so they could figure out how to get inside of you and take out your pancreas without killing you. (1:11:35) I mean, that's amazing.
Scott Benner (1:11:36) You know what I mean? (1:11:37) Like, god bless them and thank you. (1:11:39) But the system Yep. (1:11:40) The process is where if you're not if you're not on top of it, then somebody else is. (1:11:46) Like, so
Lara (1:11:47) That's right.
Scott Benner (1:11:48) You know, I grew up around here, so I'm I'm more accustomed to a killer be killed lifestyle because that's just I mean, if you for you guys that live in the South and everybody's like, oh, I'm gonna go to lunch and two hours later, I'll do it. (1:12:01) Like, you would you know, that doesn't happen here. (1:12:03) Like, you're out there trying to get ahead constantly. (1:12:06) You know what I mean? (1:12:07) Like, you're not just climbing a ladder.
Scott Benner (1:12:08) You're also kicking with your foot as you're going up making sure nobody's following you. (1:12:12) And and that is not a good way to live. (1:12:15) This wasn't my point. (1:12:16) But when when you have that that inside of you, it helps with this other stuff. (1:12:22) Like, you've ever listened to the podcast and been like, how did Scott get that for his daughter?
Scott Benner (1:12:25) How did like, I would never accept anything less. (1:12:28) That that's how.
Lara (1:12:29) And that's the thing. (1:12:30) You don't have to. (1:12:31) Yeah. (1:12:31) You you don't have to accept anything less.
Scott Benner (1:12:33) You just need to know what to do and often people don't have the knowledge of like where to go next or who to speak to or, like, you know, you even if you have all this piss and vinegar, like, where do I point it exactly? (1:12:43) Yeah. (1:12:43) You know? (1:12:43) Yeah. (1:12:44) Absolutely just I I I can't say that it's it's just so true.
Scott Benner (1:12:48) It it just it just really is. (1:12:50) You know, I just happen to be a person who won't I won't accept that. (1:12:56) And I will reset the hill I'll die on every day. (1:12:59) So, like, you don't wanna, like, get into a thing with me. (1:13:03) I won't give up.
Scott Benner (1:13:05) You know? (1:13:05) And but I have people in my family. (1:13:08) My mom was like, well, they said they can't do anything. (1:13:10) And I was like, no. (1:13:11) No, mom.
Scott Benner (1:13:11) I'm like, that's for other people. (1:13:13) We're gonna work this out. (1:13:14) You you know? (1:13:15) And so
Lara (1:13:16) That's me too.
Scott Benner (1:13:17) Yeah. (1:13:17) Good for good for you. (1:13:18) It's why you're here.
Lara (1:13:19) Yep. (1:13:20) I'm already defying the odds with this time frame.
Scott Benner (1:13:23) So Sure.
Lara (1:13:24) I'm just gonna keep going.
Scott Benner (1:13:26) Yeah. (1:13:26) Good for you. (1:13:27) And when when does your daughter graduate, did you say?
Lara (1:13:30) She graduates this year. (1:13:31) So her grad will be in June.
Scott Benner (1:13:34) Can I ask a a hard
Lara (1:13:35) question? (1:13:37) Yes.
Scott Benner (1:13:38) She's young. (1:13:40) Obviously, you and your husband have had private conversations. (1:13:42) But when do you when do you bring your your child into it and say, look, mommy's fighting. (1:13:48) We're doing all these things. (1:13:49) This is what's going right.
Scott Benner (1:13:51) But we should have a conversation about the things I haven't said to you yet that you might need to know, especially a person like you who knows the value of talking to their mother even in their mid forties. (1:14:02) So Mhmm. (1:14:02) Have you done that, or are you thinking about it?
Lara (1:14:05) Yeah. (1:14:06) That's that's the hard one for me because and this is where I'll cry. (1:14:13) Though those conversations do happen, and we're pretty real about things around here. (1:14:18) And there's a few things that I'm working on for her so that she has some things for from me after I'm not here should something terrible happen to me in an untimely manner while I'm not ready. (1:14:33) But we do have the real talk about about those things.
Lara (1:14:37) And, unfortunately, that brings forward a lot of emotion. (1:14:41) And and for a 17, well, it should be 17 this month, it's really hard to regulate those emotions around those things. (1:14:52) So we're trying to learn to be patient and graceful with each other and giving each other grace and space and time. (1:15:00) But there's definitely some some work still to be done in that regards with her and the family. (1:15:09) But I at this point, I'm focusing on doing well.
Lara (1:15:16) It it consumes me.
Scott Benner (1:15:18) Of course. (1:15:18) Right? (1:15:19) I mean, because you what do you what do you start thinking about? (1:15:22) Something you wanna say to her on her wedding day or if she has a baby Yes. (1:15:25) Or like that kind of stuff.
Scott Benner (1:15:26) Right? (1:15:26) Yeah.
Lara (1:15:27) The exactly that. (1:15:28) And I saw I saw in one of the feeds on Facebook, it was a going away to college, like, photo album with notes and gift cards and that kind of thing for specific days along the way, and I was kind of working on that. (1:15:45) One page would have, like, a photograph and then a little note from me and and go get a manicure or buy someone a coffee or something like that. (1:15:55) So I'm focusing on on those kinds of things and then preparing for the eventuality should I not be there. (1:16:03) At first, I wasn't sure I was gonna be here for her graduation, but I'm pretty I'm pretty sure that that's gonna be a okay given how things are going.
Scott Benner (1:16:12) That's amazing.
Lara (1:16:13) But beyond that, I don't know.
Scott Benner (1:16:16) Yeah. (1:16:17) I saw these two girls on TikTok maybe, and they're not not that old. (1:16:21) They're they they felt to me, like, between 19 and, like, 22, like, that that age. (1:16:26) They're sisters. (1:16:27) Right?
Scott Benner (1:16:27) And I guess they lost their mom to cancer. (1:16:29) And they get together once in a while and tell their mom into a TikTok video all the things that that that, they you're thinking it's gonna be something sweet. (1:16:40) They tell them all the they tell their mom all the things they've screwed up or didn't tell her when she was alive or something. (1:16:45) It's pretty hilarious. (1:16:47) And
Lara (1:16:47) I love that.
Scott Benner (1:16:48) Yeah. (1:16:48) They like unburden themselves to their mother through TikTok. (1:16:51) Their their mother has passed. (1:16:53) And at one point, the girl one of the girls just starts cackling, laughing, and she goes, I drove my car for a year without insurance. (1:16:59) I didn't know you needed it.
Scott Benner (1:17:01) Like and she's just, like, laughing and, you know, and she's, like, here I think they get on there, like, mom, here's all the things we've done since you're gone that I know you'd be disappointed by. (1:17:10) And they just start rattling off this stuff. (1:17:12) It's very funny.
Lara (1:17:13) I kind of love that.
Scott Benner (1:17:14) Yeah. (1:17:14) It's very funny actually. (1:17:15) And it it made me feel good for them because they were really, like, together just they were laughing heartily. (1:17:21) Like, they they they were remembering their mom in a in a really lovely way. (1:17:25) And at the same time, I think there was some, like, child like, hey, I screwed a couple things up and I need to tell somebody.
Scott Benner (1:17:35) Like, it was Mhmm. (1:17:35) It was really interesting. (1:17:36) So again, we're not gonna think about that for you. (1:17:40) No. (1:17:41) But it would be I mean, I don't know how I call myself good at this and don't ask you that question.
Scott Benner (1:17:46) So I appreciate you answering
Lara (1:17:48) it. (1:17:48) No. (1:17:48) Seriously. (1:17:49) Yeah. (1:17:49) No.
Lara (1:17:49) It's it's the real it's the real talk about this stuff. (1:17:53) I mean, there's so many different layers and and so many things to think about and and plans to make both good and bad. (1:18:00) But I I think in actuality, everybody needs to be prepared for that because life changes in a second.
Scott Benner (1:18:08) Yeah. (1:18:08) And and you know what else too? (1:18:09) Like, I could get all granola here and say something and it'll sound like bull but it's actually true. (1:18:15) Having the idea like, we all live with the idea generally that we're gonna live forever. (1:18:22) Right?
Scott Benner (1:18:22) You know, like, we all feel like, oh, we'll live into our eighties and, you know, by the time I go, I'll be peeing on myself and I won't care anymore. (1:18:28) Or I say stupid stuff I'm gonna I can't wait to pinch nurses in a nursing home because nobody will say anything. (1:18:33) I wanna get to that age, you know? (1:18:35) Yeah. (1:18:36) But the truth is is that there would be value in knowing your expiration date because, you know, it's hard to think about.
Scott Benner (1:18:46) But, you know, even for me, like, my son's not married. (1:18:49) If I was gonna get hit by a car tomorrow, I'd spend the rest of the day writing things down to my children and my wife and letting them know what I what I want them to know. (1:18:57) But I don't know that. (1:18:58) So instead, if I get whacked tomorrow by a car or if, hey, let's be more realistic, Lara. (1:19:02) What if I try to clean the fucking toilet and almost kill myself?
Scott Benner (1:19:05) Okay? (1:19:06) And so, like Daddy. (1:19:08) What if I have a terrible toilet cleaning accident and I'm dead and I'd never by the way, do you think my kids would care about my advice if that's how I die? (1:19:16) Probably not. (1:19:17) Right?
Scott Benner (1:19:18) They'd be like, what are we listening to this guy for? (1:19:20) He killed himself with a spray bottle. (1:19:25) Anyway, I would I would have the wherewithal to do some of the things that you're thinking about. (1:19:31) And, you know, it's not a thing you wanna think about happening, but if it's going to happen, then isn't it a blessing of sorts to know and be able to prepare and not a blessing for well, you know what? (1:19:42) I was gonna say not a blessing for you, but maybe because you get to live through those emotions as hard as they are.
Scott Benner (1:19:46) But then, you know, five, ten years from now, your daughter gets to to have your thoughts with her, you you know. (1:19:54) Yeah. (1:19:54) And and so I don't know. (1:19:55) There's an argument to part be
Lara (1:19:56) of it all.
Scott Benner (1:19:57) Yeah. (1:19:57) There's an argument to be made. (1:19:58) Like, you're what you're trying to do is you're trying to complete your contract as a parent even if you're not gonna be able to stay for the entire employment, basically.
Lara (1:20:07) That's right.
Scott Benner (1:20:08) Yeah.
Lara (1:20:08) Yep. (1:20:09) That's a good way to look at it.
Scott Benner (1:20:10) Yeah. (1:20:10) Of course, is. (1:20:11) It's easy to say, of course, for me as I do not currently have cancer. (1:20:15) But for you, I just think as the person talking to you and and listening to you, that makes sense to me. (1:20:21) Yeah.
Scott Benner (1:20:22) So yeah. (1:20:22) Well, you have such a good attitude. (1:20:24) Can I ask that my last question is how are you maintaining this good attitude?
Lara (1:20:29) Well
Scott Benner (1:20:30) Are you on the Canadian weed? (1:20:31) Is that what's going on?
Lara (1:20:33) No. (1:20:33) I I think if you asked me before, I was quite a very pessimistic person. (1:20:41) But I quickly learned that this is not a time for pessimism because I I'm just simply not ready. (1:20:49) And I know that I subscribe now to the thoughts that what you put out there, you be specific about. (1:20:58) You you keep your attitude positive even when it's not.
Lara (1:21:02) Some days, I fake it, and some days, I I don't. (1:21:06) But I have an immense support system. (1:21:09) I have so much support from family and friends that has helped a great deal. (1:21:15) And I think, honestly, it's just it's just had I've had to take a mind switch and and change. (1:21:22) I had to.
Lara (1:21:23) Yeah. (1:21:24) Otherwise, I wasn't gonna be getting out of bed every day, and I wasn't gonna be putting in the effort to get dressed. (1:21:29) And I it was very in those early stages, I realized that I was gonna go downhill very, very quickly if I if I didn't turn that around. (1:21:38) So I just I work it's something I work at every day, and I try to keep myself out of the news and and surround myself with positive stories.
Scott Benner (1:21:49) Yeah. (1:21:50) I bet you cancer really makes you stop caring about global warming pretty quick. (1:21:53) Pretty quick. (1:21:55) Yeah. (1:21:55) You're like, who are they gonna vote in?
Scott Benner (1:21:56) And you're like, don't care.
Lara (1:21:58) Don't care. (1:21:59) What's going on in the world? (1:22:00) I really don't know.
Scott Benner (1:22:01) I can just Yeah.
Lara (1:22:03) Focus on myself.
Scott Benner (1:22:04) Yeah. (1:22:04) My situation just changed. (1:22:05) I don't care what you do. (1:22:06) That's fine. (1:22:07) Oh, you discovered a new plant, did you?
Scott Benner (1:22:10) Don't care. (1:22:11) Yeah. (1:22:11) Yeah.
Lara (1:22:13) Yeah. (1:22:13) Well, I That's me.
Scott Benner (1:22:15) I know you came on to help other people, but I'm gonna end by thanking you for doing something kind for me, which you don't know that you did. (1:22:21) To know that I did something that helped you was it felt very good for me. (1:22:28) And
Lara (1:22:28) You really did.
Scott Benner (1:22:29) Well, and you're you're nice to say that. (1:22:32) And I'm not unaware of the reach and the impact of the podcast. (1:22:36) But for some reason, this coupled not for some reason, per pretty obvious reasons. (1:22:40) That knowledge coupled with you also struggling with cancer and what has recently, you know, transpired with my mom. (1:22:48) And and, you know, because there's part of me that thinks I didn't help my mom enough.
Scott Benner (1:22:53) And I know that's not the trust me, like, intellectually, I understand that's not true. (1:22:57) But emotionally, it feels like I could have made a couple better decisions along the way or zigged when we zagged or something like that or, you know, I I was listening to this thing the other day. (1:23:08) I learned about this, supplement that helps with your blood pressure. (1:23:12) And my mom couldn't take her infusions after chemo because her blood pressure was too high. (1:23:17) And I thought, oh, I wonder if this supplement would have brought her blood pressure down, and then she could have kept taking the the infusions that were gonna keep away the ovarian cancer in which she's have lived longer.
Scott Benner (1:23:28) And, like, that's a really unreasonable thing to think, so I don't consciously think it. (1:23:32) I wanna be clear. (1:23:33) Like, I'm not sitting around beating myself up about that.
Lara (1:23:36) Yeah.
Scott Benner (1:23:36) But emotionally, it hurts. (1:23:39) And when you said what you said, you you emotionally made me feel better. (1:23:45) I I thought, like, oh, this lady has this this struggle and I made this thing and it it made it better for her. (1:23:51) Like, they didn't fix it, but it made it better. (1:23:53) And, anyway, so you you've made me feel good.
Scott Benner (1:23:57) I appreciate it.
Lara (1:23:58) I'm so glad. (1:24:00) I I really enjoy the podcast. (1:24:02) I shared it with others. (1:24:05) I I don't know. (1:24:06) I think there's value in it for a lot of people.
Scott Benner (1:24:08) Yep. (1:24:09) I also defy other people to make a ninety minute podcast about pancreatic cancer where you laugh and curse as much as we did. (1:24:15) I thought we had a good time.
Lara (1:24:17) We did.
Scott Benner (1:24:18) We did. (1:24:18) Did. (1:24:18) Really did. (1:24:19) I did enjoy it. (1:24:20) Well, thank you so much for doing this.
Scott Benner (1:24:21) If you hold on for just one second, I'd like to talk to you after we're done recording.
Lara (1:24:24) Yeah. (1:24:25) You bet.
Scott Benner (1:24:33) Thanks so much to Laura for coming on the show and sharing her story with us. (1:24:38) A huge thanks to Dexcom for supporting the podcast and for sponsoring this episode. (1:24:43) Dexcom.com/juicebox. (1:24:45) Go get yourself a Dexcom g seven right now using my link. (1:24:50) A huge thank you to one of today's sponsors, Gvoke Glucagon.
Scott Benner (1:24:54) Find out more about Gvoke HypoPen at gvokeglucagon.com/juicebox. (1:25:00) You spell that, gvokeglucagon.com/juicebox. (1:25:20) If you're looking for community around type one diabetes, check out the Juice Box podcast private Facebook group. (1:25:26) Juice Box podcast, type one diabetes. (1:25:29) But everybody is welcome.
Scott Benner (1:25:31) Type one, type two, gestational, loved ones, it doesn't matter to me. (1:25:35) If you're impacted by diabetes and you're looking for support, comfort, or community, check out Juice Box podcast, type one diabetes on Facebook. (1:25:45) The episode you just heard was professionally edited by Wrong Way Recording. (1:25:50) Wrongwayrecording.com. (1:25:53) If you're not already subscribed or following in your favorite audio app, please take the time now to do that.
Scott Benner (1:25:58) It really helps the show. (1:26:00) And get those automatic downloads set up so you never miss an episode. (1:26:04) Thank you so much for listening. (1:26:06) I'll be back very soon with another episode of the juice box podcast.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!