Helping Children with Diabetes Gain Independence
This is the finale of the series. Links to previous posts are below, if you'd like to read it in order.
I was asked recently on my blog if I had any tips for a family that was considering Arden’s school day diabetes management plan. Anything that I hadn’t mentioned – perhaps a tip that would make the transition smoother. I responded in part by saying, “I didn’t know what I was doing when I started either.” I think that’s the most powerful message of support I could offer anyone. None of us know what to expect when we forge our own way with type 1 diabetes. All we have is the knowledge that we’ve been able to accumulate, but I think that’s a lot.
Consider how little you knew on the day that your child was diagnosed and remember how your doctors only began to scratch the surface when they explained diabetes care. Now, you probably have more diabetes knowledge than three doctors combined. I know that I am the foremost expert on my daughter’s physiology. I can, with great accuracy, predict how her body will react to insulin, exercise, stress and all of the factors that we pay attention to. I didn’t learn these things in school or at a doctor’s office, I learned them by experiencing diabetes – and that’s how our kids are going to learn.*
I want to caution you to not get too comfortable and to always keep a watchful eye as our children take over more and more control of their day-to-day diabetes health considerations. Because even though they are some of the most courageous and levelheaded kids a person will ever meet, they are still kids. I think they want and need to know that we are here. “We” doesn’t have to mean just parents. If you end up trying Arden’s plan in school, please remind the teacher that your child’s diabetes independence doesn’t mean that they don’t need an adult to be concerned and watchful at times. My friend’s new book reminded me recently that sometimes the most responsible children tend to get forgotten and that space can lead to apathy for them. Sometimes the trust is easy to take advantage of, especially if the child is experiencing diabetes burnout. It can happen to anyone and it will, so always remember to be a presence during those formable years.
It’s my sincere wish that this series has helped you to feel powerful and more in control. I hope that something I’ve shared has given you a new perspective and made you feel like the idea of anything being possible isn’t just something you read on an Internet meme. I also want to thank you, because I learned something from writing these pieces. I learned that I was getting too complacent and that we should be taking what we’ve learned from the last year of managing Arden’s diabetes from school and make something new happen.
I’m very excited to share that by the time you read this Arden will have gone to a concert with her best friend and her friend’s mother, without me or my wife in attendance. I’m going to take the things that I’ve learned from Arden’s diabetes management at school and use them to let go a little more. I’m going to use them to give Arden more freedom, so that diabetes can be a smaller part of her life. It may take a lot of self-control not to drive up the interstate behind our friend’s car and sit in the parking lot of the stadium, but I’m going to use the same courage I felt in an e-mail one of you sent me recently. If you can read about what I do and find the strength to try… so can I.
Thank you so much for reading!
My best,
Scott
Helping Children with Diabetes Gain Independence
This is part four of my six part series on helping children with diabetes to gain independence. I wrote this series for the makers of OmniPod, they are running it on their blog called, Suite D. If you missed them you can read the first three parts on Arden's Day here or on Insulet's site.
Part five, 'Taking it one moment at a time', is live today only on Suite D.
Part 4: Diabetes Management Plan
I began part one of this series by talking about technology and how it aids my family every day while we manage our daughter Arden’s type 1 diabetes. In part two, I spoke about the health and educational issues that lead me to want to do things differently. In part three, I jumped to the end of the story by sharing proof of my changes in the form of a much lower A1C and the elimination of missed class time. Today, I’d like to talk about the nuts and bolts of Arden’s diabetes management plan. It’s super simple…yet amazingly effective!
I’ll begin in the early morning because starting the day with a manageable blood glucose number gives you a reasonable chance of getting the rest of the day to follow suit. I like to check Arden’s blood glucose about an hour before her alarm is set to go off so that I can knock a high blood glucose or try to adjust a lower number with a temp basal. We test when Arden rises and pre-bolus for breakfast. The timing of the breakfast bolus is planned so that no more than two hours goes by before our next blood glucose look-in at 9:30 AM.
In between the breakfast bolus and 9:30 AM, Arden will text me if her CGM indicates that her blood glucose has gone below our low limit, above our high limit or shows arrows that indicate a fast rise or fall in her blood glucose. Most days, however, I don’t hear from her until the 9:30 AM pre-snack look-in. Both of our phones are programmed with matching alarms to remind us of CGM checks, pre-bolus needs, blood glucose testing and activities, such as gym class. The alarms are a back-up, as there are times that we both need reminding.
Arden’s text will arrive as simply as this: 140 >.
Depending on the situation I may say something like, “15 carbs,” “test” or “juice.” Arden responds in a few moments with the suggested bolus, a blood glucose reading from a finger stick or a suggestion for a different source of carbs. Our conversations generally last less than two minutes.
The next alarm sounds 15 minutes before lunch and we always test. I like, when the situation allows, to have Arden pre-bolus lunch unless her blood glucose is borderline. When that happens I have her bolus some of the lunch carbs early and then we do the rest when she is seated in the cafeteria. Arden’s 504 plan allows her to leave for lunch five minutes early everyday so that she can settle in and communicate with me prior to the insanity that surrounds the children piling into the cafeteria. We normally speak to each other at this look-in because there is a lot more going on surrounding a meal than during a simple CGM check or test and bolus. Our 504 plan also allows for us to call each other whenever we need, at any time of the day.
Two hours later, we take a look at the CGM. Too much lunch insulin? Not enough? This is a great time to find out and the check gets us ready for the bus ride that’s coming in a couple of hours.
Handling Low Blood Glucose Readings at School
At this point you are wondering how we handle low blood glucose levels, am I correct?
We have a stash of juice boxes, pre counted snacks and water in Arden’s classroom. Additionally, Arden carries herOmniPod PDM, CGM, lancing device, test strips, fast-acting glucose and a juice with her in a small purse. The combination of well-timed look-ins and our reminder alarms stave off most unexpected lows, but they still happen. Last week Arden’s blood glucose was falling fast during gym class. I received the following text…
“61 arrow down”
I replied, “juice then test.”
This is the moment when you have to trust the system because you have to wait for a minute or two to allow time for drinking and re-testing. It can be nerve-wracking…I won’t lie.
Arden: “Juice in.”
Me: “Dizzy?”
Arden: “No, I want to go back to gym.”
Me: “Calling.”
We spoke on the phone and Arden told me that her CGM arrow was already turning back up, she did not feel dizzy and reiterated that she wanted to go back to the activity.
As much as moments like these can scare me, most of the fear that I’m feeling is really Arden gaining independence, and of course, me giving away control. But isn’t that what I want and is there really a better way for her to learn?
Please know that I was compensated for my writing in an amount that would be considered standard for freelance blogging. My family pays for Arden's OmniPods with insurance and out of pocket cash. My writing for Insulet has no impact on my opinions or the information that I share here or anywhere online.
Helping Children with Diabetes Gain Independence
If you read part one or two you can skip this little description and move on to the post...
So a while back the people who make the OmniPod asked me if I would like to contribute to their new blog called Suite D. I said yes, but I had one caveat that I honestly never thought that they would agree to - but they did!
See, Insulet wanted me to write a series of posts about how we use text messaging to manage Arden's type I and I wanted to tell that story here on Arden's Day. My caveat? I get to repost my writing here after it has run on their blog. This is not something that many websites would agree to because they understandably want their content to be fresh and exclusive -- I want to give major kudos to Insulet for agreeing. You may be wondering what I said to get them to allow me to do this... Well, it was simple really. I couldn't write for them and give them my full effort if I felt like my writing was taking something from Arden's Day and taking something from you. I was honored to be asked and I wanted to take the freelance work, but not at the expense of my readers here. So we struck a simple, and I think, very reasonable deal. I get to repost after the piece has been live on their site for at least thirty days. A BIG "way to go!" from me to Insulet for being so cool and blogger friendly! Here's part 3 of my 6 part series on gaining independence through technology.
Part 3: Kicking Diabetes’ Butt!
In my last post, Helping Children with Diabetes Gain Independence Part 2: Texting Diabetes, I promised to tell you about Arden’s A1C. There are a number of things that I attribute to the reduction of Arden’s A1C, including:
- The support of friends, family and teachers
- The OmniPod insulin pump
- Finding the correct insulin dosing for Arden
- Utilizing Continuous Glucose Monitoring (CGM)
- Taking advantage of overnight monitoring (no food makes it easier)
- The Diabetes Online Community
- Being aggressive with high blood glucose levels
- Making good food choices
- The way that we manage diabetes while Arden is at school
Our children are at school for eight hours a day and that is a substantial chunk of time. In the past, Arden would eat or take insulin and then not see the nurse again for hours, scheduling her next check around the time we expected the insulin action to compete. So if there was a miscalculation of insulin at lunch or some other anomaly, Arden would go hours with an elevated blood glucose level. By removing other people from her diabetes management process at school,we also removed the constraints of relying on those people’s schedules. Arden no longer only considers her diabetes at 10:00 AM, 12:00 PM and 3:00 PM. Now we address diabetes-related issues as they arise and have the ability to make small adjustments. Being able to bump a low blood glucose and reassess in 20 minutes is far more effective than taking in a predetermined amount of carbs, hoping for the best and addressing any high blood glucose values that may arise hours later.
Similarly, if a mealtime bolus doesn’t work the way we expect, Arden’s CGM tells us her blood glucose is on the rise and she instantly texts me. I couldn’t expect the nurse to be comfortable giving more insulin an hour after a meal, but I am. I know Arden and how she reacts to different situations. I have the full knowledge of her diabetes history in my head. I can make adjustments on the fly, just as she will be able to do one day when we transition away from me being involved with her diabetes care every moment.
This access to Arden during the eight hours of each school day allows me to have the same control I do when she is with me, because honestly… it’s like I’m there.
Now, I promised you information on her A1C, so I better get to it!
All of the things I listed above are, in my opinion, critical to Arden’s A1C. I love the fact that she sleeps for a third of every day; diabetes management is so much easier then when there’s no food involved. There are two reasons I was able to let go of my fear of nights: the OmniPod and CGM technology. Using an insulin pump is key, because it allows for the reduction or temporary suspension of background insulin. For me, manipulating temporary basal rates is the essence of controlling borderline lows throughout the day – and especially overnight. The CGM lets me know if my plan hasn’t worked out and that’s already a third of the day covered.
The part of the day that she is with me and awake is the toughest for me. Handling things like big meals at inopportune times, running to sports and homework can be challenging. And I can get tired and unfocused in the late afternoon.
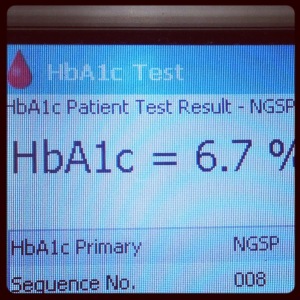
Arden’s A1C was in the nines when she was diagnosed. It languished in the mid-eights for years. I finally began to combine all of my diabetes theories into a cohesive plan in the early part of 2012 and we saw a reduction to 7.8. At the beginning of this school year we managed to get that number to 7.5. I was happy! Then the new school plan went into effect, which allows me to happily tell you two things today that you may not believe…
Arden has NEVER visited the nurse’s office for a diabetes related issue since we started our texting system and her A1C is 6.5.
Update on 2013-10-10 14:18 by Scott Benner
This post was written over four months ago. Since then Arden's A1c has been tested again and was 6.7.
Please know that I was compensated for my writing in an amount that would be considered standard for freelance blogging. My family pays for Arden's OmniPods with insurance and out of pocket cash. My writing for Insulet has no impact on my opinions or the information that I share here or anywhere online.
Helping Children with Diabetes Gain Independence
If you read part one you can skip this little description and move on to the post...
So a while back the people who make the OmniPod asked me if I would like to contribute to their new blog called Suite D. I said yes, but I had one caveat that I honestly never thought that they would agree to - but they did!
See, Insulet wanted me to write a series of posts about how we use text messaging to manage Arden's type I and I wanted to tell that story here on Arden's Day. My caveat? I get to repost my writing here after it has run on their blog. This is not something that many websites would agree to because they understandably want their content to be fresh and exclusive -- I want to give major kudos to Insulet for agreeing. You may be wondering what I said to get them to allow me to do this... Well, it was simple really. I couldn't write for them and give them my full effort if I felt like my writing was taking something from Arden's Day and taking something from you. I was honored to be asked and I wanted to take the freelance work, but not at the expense of my readers here. So we struck a simple, and I think, very reasonable deal. I get to repost after the piece has been live on their site for at least thirty days. A BIG "way to go!" from me to Insulet for being so cool and blogger friendly! Here's part 2 of my 6 part series on gaining independence through technology,
Part 2: Texting Diabetes
I sat down in my daughter’s 504 meeting after she finished second grade with a plan. Each year we make small adjustments – preparations for new aspects of the school day that come with advancing to the next grade level. These meetings are very productive, somewhat brief and usually not very eventful.
The nurse began to talk about how we could give Arden a little more responsibility with her diabetes management in third grade. This was something we did each year during this meeting and sometimes, if warranted, during the school year. We strive to shift Arden’s diabetes care onto her plate bit by bit, as she is able to accept new responsibilities. The idea is to slowly get her acclimated until the day comes when she is completely self-managing her diabetes without even realizing anything has changed.
I like that process very much and it was working extremely well. So well, in fact, that before the nurse could finish her thought I stopped her and said, “I don’t want Arden to come to your office next year. It takes up too much of her day and I think the lost time is damaging her learning process. She is missing vital parts of instruction and I want to change that.” They of course agreed, but were initially confused about how I intended to change the situation.I continued, “Arden is going to manage her diabetes herself from now on and I am going to help her. She will handle everything right from her desk and I will oversee each decision with text messages (and phone calls if and when necessary).”
Cue the blank stares…
I filled the silence before anyone could protest too much. Our previous governor signed a bill giving students with diabetes the ability to test their blood glucose anywhere in the school. So testing in the classroom wasn’t an issue. And Arden’s 504 plan already allows her to carry a cell phone, so all I needed to do was explain that sending text messages wasn’t going to be a distraction to the other students. They were intrigued.
I began to explain how much better I imagined Arden’s A1C would be if we could make small adjustments throughout the day instead of only addressing her blood glucose every few hours. Then I turned to her teacher and asked how much cumulative time she thought Arden missed each day while she was at the nurse. She replied, “Forty-five minutes maybe.” I didn’t hesitate to show off my impressive math skills and said, “That’s almost four hours a week… fifteen hours a month.”
They couldn’t disagree with my argument. Everyone knew that a student can’t thrive when they miss that much of their school day. There were a lot of faces in the room and I could see on each one of them that I had made my point. I reassured them that my idea would work and that we should try.
Arden and I practiced all summer and came up with our own little diabetes management shorthand. I found a few emoticons that were representative of the arrows on Arden’s continuous glucose monitor and we were off.
Putting Arden’s New Diabetes Management Plan into Action
Today, almost one complete year later, even I can’t believe how well my plan has worked. One week towards the end of the school year Arden’s blood glucose had been low all week. I didn’t know why. I had been using temp basal rates and adjusting boluses, and she just kept running low. I’m talking about blood glucose levels in the 50, 60 and 70 range – situations that required immediate action.
But guess how many times Arden had to go to the nurse’s office that week? Zero. Guess how many times Arden had to go to the nurse’s office all year? Yes, you guessed it… zero! Arden did not need to leave her classroom once to address a diabetes-related issue. We treat lows, bolus for highs and count carbs all with text messages like in the screen shot above.
This simple technology that most everyone possesses is one of the most valuable and productive diabetes technologies that we employ. The independence that it gives Arden and me is unmatched. The peace of mind that being able to text her brings me is soothing. The effect that this process has had on her diabetes management is staggering! Just wait until I tell you about Arden’s A1C in my next post.
Please know that I was compensated for my writing in an amount that would be considered standard for freelance blogging. My family pays for Arden's OmniPods with insurance and out of pocket cash. My writing for Insulet has no impact on my opinions or the information that I share here or anywhere online.
Helping Children with Diabetes Gain Independence
So a while back the people who make the OmniPod asked me if I would like to contribute to their new blog called Suite D. I said yes, but I had one caveat that I honestly never thought that they would agree to - but they did!
See, Insulet wanted me to write a series of posts about how we use text messaging to manage Arden's type I and I wanted to tell that story here on Arden's Day. My caveat? I get to repost my writing here after it has run on their blog. This is not something that many websites would agree to because they understandably want their content to be fresh and exclusive -- I want to give major kudos to Insulet for agreeing. You may be wondering what I said to get them to allow me to do this... Well, it was simple really. I couldn't write for them and give them my full effort if I felt like my writing was taking something from Arden's Day and taking something from you. I was honored to be asked and I wanted to take the freelance work, but not at the expense of my readers here. So we struck a simple, and I think, very reasonable deal. I get to repost after the piece has been live on their site for at least thirty days. A BIG "way to go!" from me to Insulet for being so cool and blogger friendly! Here's part 1 of my 6 part series on gaining independence through technology.
Part 1: Helping Children with Diabetes Gain Independence
I recall being handed syringes in the hospital and thinking that they seemed so very lightweight. I guess that I had never held one before that day and didn’t know what to expect. They felt flimsy in my hand and I struggled to understand just how these bits of plastic and metal were going to keep my daughter healthy.
That was my perspective only a few days removed from our two-year-old daughter’s type 1 diabetes diagnosis in August of 2006. Today, I realize that if Arden had been diagnosed fifty years earlier those little needles would have likely looked and felt like something from a science fiction movie.
Gaining Independence through an Insulin Pump
The technologies that help to improve the lives of people with type 1 diabetes are nothing short of amazing – and the ways that we use that technology are ever expanding and evolving. I love the idea of utilizing what we have available today to the fullest, but I always keep an eye on the future and wonder where it will take us.
The first time I saw the table full of insulin pump samples at our endocrinologist’s office, the OmniPod insulin pump jumped right out at me. I was first struck of course by the tubeless nature of the device, but quickly, my mind raced with the possibilities of how the manufacturer could continue to adapt and blend advancements, because of its self-contained design. I told my wife, “I like that one. When they improve it we won’t have to wait to benefit.” That’s what I liked most about the OmniPod – it felt like the future and I couldn’t see a limit to the possibilities of where it may go.
Here we are many, many years later and I find myself about to talk to you about technology and how it has improved my daughter’s life – really my family’s life – and given her more independence. But now I’m going to talk about another piece of technology that we all have in our pockets, something that when used correctly will take you to the future and free you from restraint. Let me explain…
Giving Our Children More Freedom with Diabetes
Our children go. They go to school, to their friend’s house, to a movie – they are constantly going. Parents of children with type 1 diabetes are conditioned to fear the feeling of their child’s natural desire to just go. We want our children to have that leisurely feeling of course – that carefree, run-out-the-back-door feeling that we enjoyed as children. I don’t want to think about what could go wrong on a school bus ride. I hate telling my daughter she can’t visit a friend’s house because their parents don’t have a working understanding of diabetes and I am willing to bet that you feel the same.
Freedom and independence for our children with diabetes – but how?
How Technology Can Provide More Independence
Arden was missing class each time she visited the nurse’s office at her school. Before recess, before gym, before lunch, after exercise and every other time diabetes came to call, Arden missed class time. It was only five minutes here and three minutes there, but by the end of the day those minutes added up. After a week, they were hours and by the end of the year, they were days. Days of learning, days of socialization and days of her life – gone.
If only I could just be there, stand in the corner so I could invisibly wander to her desk and oversee her insulin dosing decisions. I just needed to be able to whisper in her ear that she didn’t need all fifteen carbs to correct that low blood glucose. I only needed to be there for a second, just like when she is home with me. Then it hit me… I can be.
Arden was in her bedroom one Saturday afternoon when I needed to know what her blood glucose (BG) was. Instead of walking upstairs I sent her a text message that said, “Test your BG please.” A few moments later I received a return message: “134.” I was with her, but I wasn’t. We were managing her blood glucose with only a momentary pause to her activity; this was the minimal interruption that I dreamed of. If only she could have her phone with her at school…
I’ll be back soon to tell you how I explained to the school what I was planning for her diabetes management, their surprising reply and all the goodness that’s come since.
Please know that I was compensated for my writing in an amount that would be considered standard for freelance blogging. My family pays for Arden's Omnipods with insurance and out of pocket cash. My writing for Insulet has no impact on my opinions or the information that I share here or anywhere online.