Encapsulation Gives Me Reason to Hope
When I hear the word ‘cure’ it sends my mind racing with visions of science fiction television. I imagine my daughter being scanned by Doctor McCoy, in an instant his tricorder beeps and Arden’s pancreas springs back into action. Everyone in the room takes a pause for dramatic effect and type 1 diabetes is no more.
It’s that level of high yet unreasonable expectation, mixed with a healthy amount of cynicism that keeps me from becoming too excited when news of “promising research” is announced. I read the articles - well, I thoroughly peruse them - but most research news leaves me feeling like real-world science hasn’t quite caught up to the desires of the scientific community. Curing a disease without significant effort, crazy drugs and more than a bit of luck seems unlikely to me right now. In other words, I’m a tough sell.
Until I heard about Beta Cell Encapsulation…
Encapsulation grabbed my attention in such a big way that I asked it’s benefactor, JDRF (formally known as Juvenile Diabetes Research Foundation) if there was someone that I could interview about the technology. They were kind enough to put me in touch with JDRF Director of Discovery Research, Albert Hwa, PhD.
My conversation with Albert did a few things. It reminded me that I am not a scientist, gave me great hope for type 1 diabetes treatments and made me want to tell you about what I learned without being too sciencey - because I don’t want you to just peruse this article.
What is Encapsulation: In layman's terms, the process of encapsulation has made it possible for foreign cells to be introduced into the body after being coated (encapsulated) with a substance that protects them from your immune system. Specifically for the ViaCyte product design, the cells are inserted into a device that is currently the size of a business card and surgically placed under the skin during an outpatient procedure. The device allows its cellular passengers to interact with the body, measure the level of glucose and produce insulin without being identified by the immune system as a foreign body - all without anti-rejection drugs. Through the nature of science, encapsulation keeps your immune system from attacking the new insulin producing cells without blocking other needed functions. That’s science!
Is this a cure: Encapsulation is not a cure but it is the first stopgap between a cure and the reality that people living with type 1 diabetes experience that makes me say, “Where do I get this for my daughter?” It’s not a cure because the root issue is not being addressed, as the pancreas remains devoid of insulin-producing cells, and the autoimmune responses against them persists. The goal of this research is to introduce donor beta cells that will eliminate the need for manmade insulin. That would mean no more shots, finger sticks, insulin pumps, glucose monitors and the wildly fluctuating blood glucose levels that cause serious long-term health issues.
How long will the device last: Researchers aren’t positive at this time how long the cells will produce insulin before they need to be replaced, but a minimum of two years seems to be the initial hope and goal. Having a small procedure every two years is a vast improvement over what my daughter and the millions of other people who have type I diabetes deal with every moment of their lives.
More details you want to know: There are currently two companies conducting trials on encapsulation, both are being partially supported by the JDRF. The trial that was being held as I spoke with Albert Hwa was happening in a human being. Human trials are very exciting because so many ideas never get past animal trials; Most of the research that people with type 1 diabetes hear about cures mice but never makes the leap to helping people. The encapsulation human trials are in their infancy; Albert told me that even if everything went exactly perfect with the trials, it would still be “ten years” before Encapsulation could become a reality.
I chose to learn more about encapsulation because I’ve watched my daughter live for nearly a decade with type1 diabetes and this is the first time that I’ve felt like I was looking at a potential answer that could make it to market. I’m not a health care professional, just a father hoping for his daughter’s life to get better. In my estimation, encapsulation feels possible. I can imagine driving my daughter to her doctor to have a form of this device implanted, not unlike a pacemaker. For a guy that doesn’t usually feel very hopeful about stuff like this - I feel hopeful.
You can read more about encapsulation on the JDRF website, they even have the sciencey stuff:
Children who have had enterovirus infection are around 50 percent more likely to have type 1 diabetes
Arden had the Coxsackievirus prior to her type I diagnosis...
from science daily.com
A new study published in Diabetologia (the journal of the European Association for the Study of Diabetes) shows that children who have been infected with enterovirus are 48% more likely to have developed type 1 diabetes. The study is by Dr Tsai Chung-Li, China Medical University, Taiwan, and colleagues.
"Type 1 diabetes is considered to be caused by complex interaction between genetic susceptibility, the immune system, and environmental factors," say the authors. "Though the cue for genetic predisposition has been elucidated, evidence also points to involvement of enterovirus (EV) infection, including viruses such as poliovirus, Coxsackievirus A, Coxsackievirus B, and echovirus."
To investigate the link between EV infection and subsequent type 1 diabetes, the researchers used nationwide population-based data from Taiwan's national health insurance system. They looked at type 1 diabetes incidence in children aged up to 18 years with or without diagnosis of EV infection during 2000-2008.
Overall incidence of type 1 diabetes was higher in the EV-infected children than in the non-EV infected group (5.73 vs. 3.89 per 100,000 people per year, showing a 48% increased incidence rate in EV-infected versus non-EV-infected children). Hazard ratios of type 1 diabetes increased with age at diagnosis of EV infection, with a more than doubling of the risk of type 1 diabetes (2.18 times increased risk) for children aged over 10 years at entry. No relationship of allergic rhinitis or bronchial asthma to type 1 diabetes was found.
The authors point out that despite countries such as Finland and Sweden having the highest incidence of type 1 diabetes worldwide, they are thought to have low background rates of enterovirus infection, suggesting that genetic factors are a large component of the high type 1 diabetes rates in those countries. But they add: "Regions such as Africa, Asia, South America have a low but increasing incidence of type 1 diabetes and high prevalence of enterovirus infection; environmental factors like enterovirus infection may play a vital role in increasing incidence in these regions."
They add: "Taiwan has relatively low type 1 diabetes incidence; we believe that the marked escalation of the said incidence in recent decades can be largely attributed to the highly endemic spread of enterovirus infection in Taiwanese children, given that there has been little gene flow and genetic drift in such a short period."
They conclude: "This nationwide retrospective cohort study found a positive correlation of type 1 diabetes with EV infection. Our results suggest that preventive strategies, such as an effective vaccine against EV infection, may lessen the incidence of type 1 diabetes in Taiwan."
The journal article referenced can be downloaded as a PDF from Diabetologia here
JDRF Partner ViaCyte to Immediately Initiate Type 1 Diabetes Clinical Trial
We are extremely pleased the FDA has allowed the company to move forward with a human clinical trial of its innovative type 1 diabetes (T1D) encapsulated cell replacement therapy...
From JDRF.org
JDRF’s partner ViaCyte recently announced the U.S. Food and Drug Administration (FDA) is allowing them to move forward with a clinical trial of its innovative type 1 diabetes (T1D) encapsulated cell replacement therapy called VC-01™ product candidate. The company plans to immediately initiate the first ever clinical evaluation of a stem cell-derived islet replacement therapy for the treatment of people with T1D. The trial will enroll approximately 40 people at multiple clinical sites.
Trials on people, not mice.
Human GI Cells Retrained to Produce Insulin
I don't post nearly all of the stories that I read about cure research, but I found this one to be particularly interesting and wanted to pass it on.
I don't post nearly all of the stories that I read about cure research, but I found this one to be particularly interesting and wanted to pass it on.
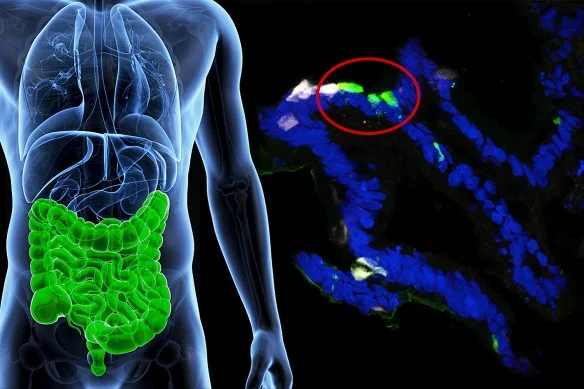
Human gastrointestinal cells from patients were engineered to express insulin (fluorescent green) in the lab. (Image by Columbia University Medical Center.)
Excerpts from a Columbia University Medical Center press release:
By switching off a single gene, scientists at Columbia University’s Naomi Berrie Diabetes Center have converted human gastrointestinal cells into insulin-producing cells, demonstrating in principle that a drug could retrain cells inside a person’s GI tract to produce insulin.
The finding raises the possibility that cells lost in type 1 diabetes may be more easily replaced through the reeducation of existing cells than through the transplantation of new cells created from embryonic or adult stem cells.
After seven days, some of the cells started releasing insulin and, equally important, only in response to glucose.
You can read the entire press release here
Type I Diabetes CURED (In mice)
Dear Scientists,
I know that it must be difficult to find research money for your study and I understand that you are under pressure to generate excitement about your work.
I'm also extremely grateful to anyone who is trying to find a cure for type I diabetes. I don't want you to stop looking or collecting grants and donors, but I do need you to do one small favor for me, well, actually for everyone who is touched by type I diabetes.
STOP publishing your "exciting" news about curing lab mice!
You see, when I open my laptop and read your story about how you coaxed a cell into producing insulin, I shrug and go about my business because my daughter has been living with diabetes for a very long time and I've seen a thousand articles just like yours. I know not to get excited - I know that you're fishing for donors. I understand that you are trying to justify the space that you take up in some lab. I get what the price of doing business is, I empathize.
But how about having some compassion for the countless families who are new to type I diabetes, maybe you shouldn't be getting their hopes up just to break their hearts all over again. Maybe, you should just shut up until you figure out a way to help a person. These stories hurt people. Parents, adults, friends and family. People are crushed when you lift them so high, only to drop them down onto their reality. The next time I hear you talk about a mouse, it better be because you figured out how to use that "cure" you found in a person. We have feelings, consider them.