Guest Post: Diabetes Glastonbury
Diabetes Glastonbury
Read Rob’s post from day one and two
If you don’t know, Glastonbury is a gigantic music festival in the UK. Over 5 days it deatures 2,000 different acts on 90 different stages. A town with the population of Buffalo NY is built in the Somerset countryside and lasts for just a couple of weeks before the fields are handed back to the dairy cows. You can’t make a plan because things distract you as you try to carry it out, you always want to be in two places at once, there’s mega-walking to do (I racked up 50,000 steps over 3 days) and the very best things (Jennifer Mahammadi’s talk on day 2 for me) are a complete surprise.
Glastonbury tickets 2020: Deadlines, sale dates and everything you need ...
Okay, so maybe it’s not exactly like Glastonbury
Happily, like the Sunday of Glastonbury, Day 3 of the Diabetes UK Professional conference are a bit more relaxed. The opening session was about early onset Type 2 diabetes. Not really my thing, but Professor Helen Murphy spoke of the importance of preparing women with diabetes for pregnancy. A lot of us worry about that for ourselves and our daughters and it surprised me that I hadn’t come across this idea. Here’s the message: If you’re planning to get pregnant (i) take 5mg of foli acid daily (ii) get your HbA1c down as low as you can, ideally below 43 (6.1%) (iii) check with your primary care doctor about medications that aren’t great during pregnancy such as blood pressure control tablets or statins. These things massively improve the odds of a successful pregnancy, to roughly the same level as the general population.
HbA1c<43 = Best chance of healthy baby. And get some folic acid.
Later on we heard about the future of CGM use in diabetes care. Personally, I found it a bit frustrating in several ways. The medics still aren’t getting just how revolutionary Dexcom and Libre have been for us. The HbA1c U shaped mortality study was referenced a lot. In a nutshell this massive 10 year study in China found that mortality increased when HbA1c fell below 5.7% and it also increased when HbA1c was over 6.7%. The study impresses because of it’s 10 year duration and the 35,000+ patients who were part of it.
But in referring to it the medics are overlooking a pretty gigantic factor: In 2012 Dexcom released the G4. In 2015 Abbott release Libre. These devices had had an utterly dramatic impact on the lives of those of us with Type 1. They make the Chinese study unhelpful at best and actively misleading at worst. Despite at least 2 people with Type 1 setting out to the conference just how much difference these things can make, the message still isn’t getting through. In terms of mortality below HbA1c <5.7, it’s akin to relying on a study performed before insulin was discovered in 1922.
It’s scary that the sexiness of big science seems far more important to some doctors than the value of providing treatment to individual patients. Hey ho. Rant over.
Median HbA1c down from 73 to 61 in 13 years – Well done HCPs! (And patients? Maybe?)
The final session of the day was presented by Professor May Ng, Dr Tom Crabtree and Dr Clare Hambling. Tom spoke on the success of the NHS England pilot to see the effect of closed loops on HbA1c in practice, May of the reduction in HbA1c among children using these systems and Clare on how they might be rolled out in practice. An idea she trailed was that of a national (international) helpline expert in all the different systems. Doctors sign up to practice medicine rather than IT but my own experience of AID is that it’s the techy side that’s the bigger problem, not the medicine. Comfortingly May also identified that whilst the UK is doing really well on diabetes care Sweden is doing even better. She didn’t mention the U shaped mortality study…
Complications: HbA1c really, really matters
So, that’s it from me at this year’s Glastonbury Diabetes Professionals Conference. It was an incredible privilege to be amongst these impressive HCPs. Their brilliance and commitment to the cause was beyond question. There’s going to be a lot of patients getting better care next week as the connections and ideas exchanged this week feed back into front line practice.
BOB
Rob (Bob Dee) Darbyshire
Guest Post: Grande Challenges!
Grande Challenges!
I thought Day 2 of the Diabetes UK Professional Conference might be easier. Maybe get some lunch and not spend so much time on my feet. I was a bit wrong. (Read Day One from Rob)
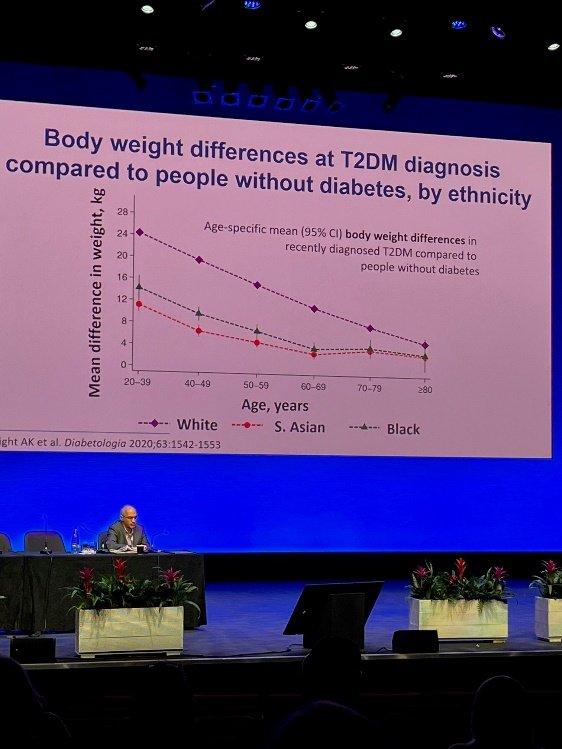
Ethnicity as a risk factor in T2
Today, I was able to spend more time in the presentations (and not just because I needed to sit down) mostly about diabetes causation and – drum roll - a cure. The day opened with an impressive lecture about the genetic links to diabetes. For me the takeaway was that Black and South Asian people develop type 2 when they’re skinnier than white people.
The rest of the morning I spent chatting with the awesome reps at Insulet and Dexcom. I got my hands on a Dexcom G7. It’s a real upgrade on my current Libre 2 because of the volume of real time data I could get out of it without a third party app. It’s small, really small, and much easier to apply than the G6. It may not seem important, but the box footprint is way smaller than the Libre 2 or the G6. This may sound trivial but with 3 Libre 2 users in the house, storage space is a genuine issue if we all get our scripts at the same time. Now I just need to persuade the kids to switch to Dexcom.
Omnipod 5 really is coming to the UK. And from what I heard, it may even be here sooner than we thought. The UK launch is going to be a “soft” one to avoid medics being hassled by all the current Dash and Eros users looking to upgrade. Cost shouldn’t be a barrier in the UK but appropriate staff training might be: HCP’s won’t be handing these out until they’ve been trained to use them.
The G7 is really, really tiny
After lunch we learned of the “Grand Challenge”. The Steve Morgan Foundation has donated an enormous £50 million to the prevention of T1 diabetes, and its cure through the development of robust stem cells that can grow into Beta Cells (without dying too quickly – that’s the barrier right now) and the development of smart insulins... that might be taken orally. As challenges go, “Grand” is an understatement.
Research on prevention seems the most advanced of these three things right now. Anyone who saw the slide I posted for the first day of the conference will recognise the increased risk of Type 1 among those with a family member already diagnosed. So far, as you can hear on Juicebox Podcast Episode #452, they’ve been able to delay the onset of Type 1 by around 2 years through the drug Teplizumab . As for a cure, it is progressing. As the implanted cells live longer and longer in their new homes, they present different problems over time. Slowly but surely, these problems are being overcome. As ever, we can look forward to a cure in ten years time… But real advances are being achieved already.
I finished the formal part of the day listening in to the discussions on eating disorders in diabetes. A shocking 40% of female teenage girls with type 1 in the UK suffer from a degree of diabulimia in which they consciously control their wait by avoiding injections. And it’s complex. We were addressed by the awe inspiring Jennifer Mahammodi. Jennifer was diagnosed at the age of 12. Her mother found it hard to help her manage with the result that there were a series of DKA hospital admissions – and Jennifer learned to associate those admissions with a time of caring and security, until she entered a cycle of almost fortnightly hospital admissions before being placed back into another foster care placement. Ultimately, living alone in social housing at the age of 19 she suffered, alone, a Christmas Day DKA episode so severe she could barely see. Thankfully, the adult care team at King’s College Hospital were able to provide psychological support and get her to a very much better place. It was a deeply moving address: amongst dozens of battle hardened HCPs there were very few dry eyes and it was the only address that I saw receive a standing ovation.
To cap off the day, I was invited to attend the presentation of a research award to Professor Roy Taylor. He’d been quite a presence at the conference putting questions to different panels with incisive intelligence and a dry wit. He pioneered the remission of Type 2 through rapid weight loss. As one of his colleagues pointed out to me, even if the diabetes isn’t remitted, weight loss is still a good idea for most Type 2s.
BOB
Rob (Bob Dee) Darbyshire
Guest Post: Diabetes Nerd Heaven!
Diabetes Nerd Heaven!
This week I’ve been lucky enough to get an invitation to Diabetes UK’s Professional Conference. As a poor muggle with no medical training beyond half a century of trying to tame the beast that is our collective family blood sugar, it’s quite a privilege. And it’s also a huge privilege to be able to share it with the Arden’s Day Blog. I’m hoping that some information about what goes on between the doctors when they think we can’t see them will be a helpful for insight for JuiceBoxers in the UK and around the world.
This year’s 3 day conference is taking place in Livepool’s Exhibition Centre and Arena. We’ll be kicked out on Friday to make way for Eurovision. Apparently, King Charles and Queen Camillahave been down to have a look at the venue this morning. As far as I know, they didn’t stop in for any of the lecture sessions at the conference. That’s a shame – they’d have learned a lot! It’s a huge event, with 4 or 5 simultaneous presentations. It’s been an 11 hour day for me there, and I’m looking forward to Manchester City vs Arsenal and an early night before the sae again tomorrow.
So – to business, A huge part of this event is networking. Over 2,000 Consultants, Junior Doctors, Diabetes Specialist Nurses, Academics, Practice Managers and so on and so on gather in Liverpool to renew friendships and share their experiences informally. So far, I’ve only managed to create one awkward silence by revealing that I’ve no medical training. But neither have I been asked how I achieve an HbA1c of 39 (5.7 in US numbers). Make of that what you will.
And I’ve learned! The first presentation of the conference was on “Nature or nurture” – the causation of diabetes. This comes up a lot as a question amongst us JuiceBoxers. Much of the chat was about Type 2 which is a really, really complicated question. For us Type 1’s Professor Ines Barrosso of Exeter University spoke of her research into the genes that are associated with Type 1. They’re now pretty clearly identified and partially explain this set of statistics:
The actual stats on family likelihood of developing T1, courtesy of Professor Barroso
But – and it’s a biggy – If one identical twin develops Type 1, there’s only a 40% chance that the other one will. And from that we can conclude that whilst there is a genetic component, there is also an environmental one. So it’s still your fault that you or your child lives with Type 1? You breast fed them, or not? You gave them anti-biotics or not? Nope. The “environmental factors” relating to causation of Type 1 are “largely unexplored” per Professor Barroso. What I take from that is that we cannot and must not blame ourselves, whether we have Type 1 or whether we have a child with Type 1. And that we need to support the research charities to find out what those causes are.
Type 2 is a different story. The impact of obesity is well understood. And there’s a genetic component. But for anyone who wants to say that one totally excludes the other – and this is the internet, we all know how it works – here’s a stat: The Pima Indians of Arizona and Mexico are the ethnic group with the highest incidence of T2 in the world, at 50%. But they’re a divided people. Those that live in Arizona, within the relative affluence and cheap calories of the USA, have rates above 50%, but their cousins in Mexico, in more straightened circumstances? 5%. The genes are playing their part, but so is lifestyle.
And other amazing things in brief:
• Get your doc or diabetes educator to give a talk in your child’s school. Not only will the kids learn something, but it’s a great way for kids who may not know each other to acknowledge each other as people living with Type 1. Having an ally in my year at school, or a couple of years above or below, would have gone a long way to addressing the loneliness I felt at school.
• Omnipod 5 really is coming to the UK. I can’t reveal when – because I don’t know exactly. But I can say that I won’t be ordering any more boxes of pods if I can get my healthcare team to switch me to a G6.
• Closed loop is coming as an “official” NHS supported tech in the UK. But don’t all rush for it at once. Rolling it out to every individual who may be eligible is going to take time.
• Dr Tabitha Randell of Nottingham University Hospital is a mega-star. Her patients are averaging an HbA1c in the 50s with minimal hypos. It won’t be a surprise to any JuiceBoxer that she’s a fan of getting a CGM on early and using a little bit more insulin, not a little bit less.
In terms of my wider experience of the HCPs, it’s become clear over the last 24 hours that the value of our “lived experience” is obvious to the clinical community. There are repeated statements about the need to listen to patients, ask what they want and ask how the medics can help. There’s real recognition, albeit with mixed levels of sensitivity, that the real experts in this condition are the people living with it. But… The Medical Establishment, like all great institutions, remains keen to look after itself before looking after the people it is supposed to serve. The word “safeguarding” is used in reference to patients, and deployed in a genuine effort to avoid damaging them. That’s great. But when it’s used to prevent those of us living with diabetes from damaging each other or ourselves it starts to be a bit weird. The internet exists. We sit alongside each other in clinics. We receive a monthly supply of a potentially lethal drug. We aren’t family pets that might or might not play nicely with other doggies. Peer support is coming as a pillar of care in the UK. It’s exciting. It requires clinicians to use judgement, tact and creativity to support it. From the guys I’ve met today, I think they’re going to be fine.
More tomorrow. Thanks for reading!
BOB
Rob (Bob Dee) Darbyshire
Guest Post: IronMan World Championship with Kris Freeman
I knew the IronMan World Championship course in St George would be hard... and it was. The 112 mile bike course had 7000 ft of climbing and the run featured unbroken climbs and descents that were several miles long. Shade was nearly nonexistent and the temp maxed out at 92 degrees in the mid afternoon.
My race plan was to start relaxed in the water, go slower for the first 60 miles of the ride than felt necessary and then see how fast I could go for the rest of the race.
My insulin strategy can be seen in the photos. I ran 1.3 units per hour until :15 minutes before my race (started at 6:45). Then I ran .6 u/h for three hours, .5 units for one hours, .4 units for one and a half hours and .25 units for :45 minutes at which point I tore the Pod off. The numbers in the photo are all .05 units lower than stated above because I was wearing a 2nd Pod that was delivering .05 u/h which is the minimum setting. In addition to the basal setting I also took a 4 unit bolus at the swim/bike transition with a syringe I pre filled before the race.
My swim was solid enough and I had no problems with my first transition. The terrain for the bike was very "western" with climbs that went on for miles followed by high speed descents that had me averaging better than 40 mph for several miles at a time. I took feeds at every aid station and probably consumed 12-16 twenty-four ounce bottles of Gatorade endurance 96 ounces of water, and a liter of Coke. I also took 8 Salt Stick electrolyte tabs. Choosing to conserve energy early ended up being a great call as my "easy" pace ended up being plenty fast and I never ran out of gas on the bike.
My transition into the run was also smooth if not super fast. I took the time to put vaseline coated socks on and chugged a full quart of water. However, my race got real hard a few miles later. I was overheating and I knew that I had to cool down or I wouldn't finish. There were aid stations every 1.5 miles and at each one I put ice in my hat and down the front and back of my suit. This was the first day of the year that I had worked out in any weather warmer than 70 degrees and my body was not happy with me. My half marathon split was far slower than I'd hoped (1:50ish) but at this point survival was the top priority. I bled tlme at each aid station but the ice and gatorade I was getting were the only things keeping me going forward. With 10 miles to go I was pretty sure I was going to get heat stroke at some point and I really wanted to get to the finish before that happened. I was stumbling and tripping over nothing as I ran on. My stomach was very nauseous and not at all happy about feeding. Even so, I forced about another gallon of Gatorade/water/Cola down my throat along with another 5 salt tabs for a total of 13 during the race.
I finished the marathon in 3:48 which was a good 20 minutes slower than I would have liked. But it wasn't for lack of trying. In the pictures you can see me striding across the finish and then taking a sharp left to get a cooler with insulin and fresh Pods from my coach. I went directly from there to the medical tent where I lied down on a Cot and proceeded to writhe around as doctors and nurses asked me how I felt. I had finished the race with a glucose of 140 so diabetes was not the main issue. I had all the symptoms of heat stroke including tingling/numb hands and feet and I began to dry heave. As the doctor decided to hook me up to an IV, I asked for a puke bag and started filling it. Fortunately the IV started to make me feel better pretty rapidly and I left the med tent under my own power about 40 minutes later.
All things considered the race went pretty well. It wasn't perfect but given the difficulty of the course and the heat it could have been worse. The consensus among the athletes I talked too was that this was the most difficult IronMan sanctioned event in the world. I finished in 10:13 which was good for a 19th place age group finish and 136th overall. I haven't been able to verify this but I think that these are the best finishes ever for a person with diabetes at the World Championships (If anyone knows differently please let me know). My result also requalified me for the 2022 World Champs in Kona this October though I chose to decline the opportunity. - Kris Freeman
Episodes of the Juicebox Podcast featuring Kris Freeman
#26 Olympian & person with diabetes Kris Freeman
How To Listen to the Juicebox Podcast
Are you looking for an entertaining and informative podcast to listen to that covers diabetes-related topics? Look no further than the Juicebox Podcast!
The Juicebox Podcast is the most popular diabetes podcast available and is a great way to get up to date on the latest research, treatments, and health tips related to diabetes. The podcast offers a variety of topics, from interviews with medical professionals to discussions on diabetes-related technology.
If you’re looking to listen to the Juicebox Podcast, there are several popular audio apps that you can use. Apple Podcasts, Spotify, Amazon Music, Stitcher, Google Podcasts, and Overcast are all popular podcast listening apps that are free and easy to use. Simply search for “Juicebox Podcast” in the app, and you’ll be able to listen to the full library of episodes.
Whether you’re a person living with diabetes, a family member, or a healthcare provider, the Juicebox Podcast has something for everyone. With engaging conversations and timely topics, the Juicebox Podcast is a must-listen for anyone interested in diabetes.
Check out the Juicebox Podcast today and let the learning begin!