#1432 Carter's Tzield Story
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
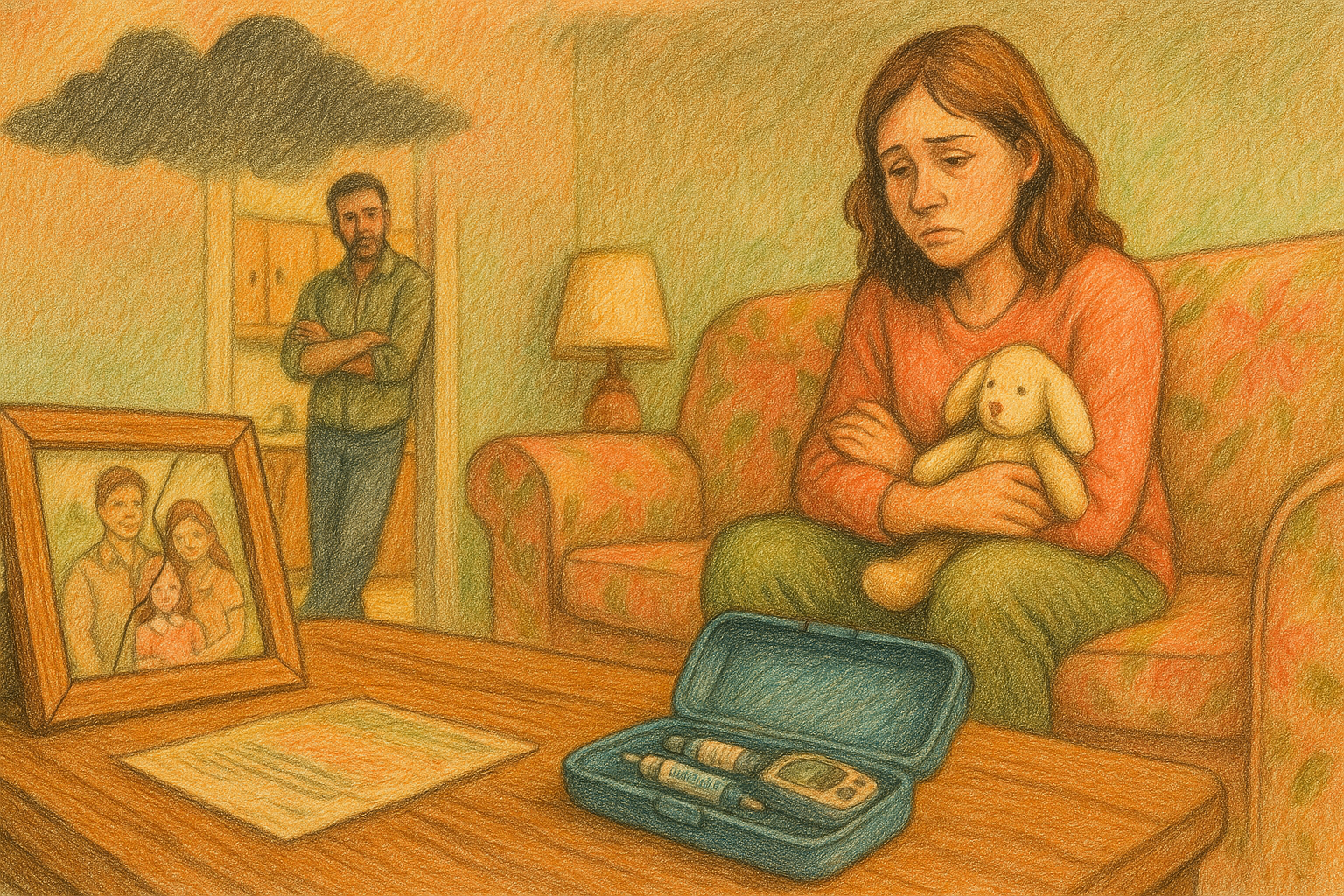
Jaime, shaped by lifelong T1D, dives into Carter’s Tzield treatment.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Friends, we're all back together for the next episode of The Juicebox Podcast. Welcome.
Jaime 0:14
Hi. My name is Jamie. I am joining today to talk about my son Carter's experience using TVL,
Scott Benner 0:20
nothing you hear on the Juicebox Podcast should be considered advice medical or otherwise, always consult a physician before making any changes to your healthcare plan. When you place your first order for ag one with my link, you'll get five free travel packs and a free year supply of vitamin D drink. Ag one.com/juice, box, don't forget to save 40% off of your entire order at cozy earth.com All you have to do is use the offer code juice box at checkout. That's Juicebox at checkout to save 40% at cozy earth.com Are you an adult living with type one or the caregiver of someone who is and a US resident, if you are, I'd love it if you would go to T 1d exchange.org/juicebox and take the survey. When you complete that survey, your answers are used to move type one diabetes research of all kinds. So if you'd like to help with type one research, but don't have time to go to a doctor or an investigation. T, 1d, exchange, org slash juice box. It should not take you more than about 10 minutes. This episode of the juice box podcast is sponsored by us med. Us, med.com/juice, box. Or call 888-721-1514, get your supplies the same way we do from us. Med. This episode of The Juicebox Podcast is sponsored by Medtronic diabetes and their mini med 780 G system designed to help ease the burden of diabetes management, imagine fewer worries about mis boluses or miscalculated carbs thanks to meal detection technology and automatic correction doses. Learn more and get started today at Medtronic diabetes.com/juicebox
Jaime 2:09
Hi. My name is Jamie. I am joining today to talk about my son Carter's experience using T deal. I have had type one diabetes since I was three years old. I was diagnosed in 1983 so those were the days of no blood test meters at home. So I've seen a lot of changes myself in diabetes treatment over the years. I have two healthy kids, and I'm trained as an epidemiologist. Growing up with diabetes sort of motivated my interest in working in the healthcare field. How old
Scott Benner 2:40
were you when? When 1983 was happening? How old were you? I was three, three. Wow. Yeah, I could figure out how old you are now, or you could tell me, which would you prefer? I am 40
Jaime 2:51
I'm 4444 Okay, thank you.
Scott Benner 2:55
All right, so you're the type one in the family. Married. I'm married. Okay, so there's a four person house, that's what we're talking about. We
Jaime 3:05
have two households. So my son's Dad and I share custody, and then I'm remarried. His dad didn't have any history of of type one in the family. My aunt has type one diabetes on my dad's side. Okay, my mom also has Graves' disease,
Scott Benner 3:20
Okay, gotcha, you just have type one. There are any other autoimmune for you? No, no, all right. How do you manage what technology do you use?
Jaime 3:30
Sure, so I probably use everything there is. But for quite some time, I've used Omnipod over 15 years, and I was excited when omnipot Five came out, and I tried that, and I did not like it, but I really didn't want to stop the, you know, non wired pump. So right now I loop
Scott Benner 3:51
and I love it. Okay, you didn't like what about Omnipod five wasn't for you?
Jaime 3:56
I don't know. I have very different insulin needs at certain times of the day, usually around 3am and 3pm I would have a much lower basal rate, or, you know, or around the 3am and the 3pm for a period of time. And Omnipod just somehow could not sort that out. And I ended up with highs at certain points of the day and lows at other points of the day. I don't know. I adjusted the settings. I couldn't seem to sort it out. I didn't like that. You couldn't change the basal. And I exercise a lot, and I was really comfortable with Omnipod, where you could say, like, a certain percentage decrease, a certain percentage increase, but then you had to turn off the automation. I don't know, with loop, you can keep the automation on and turn on those overrides, you know. So
Scott Benner 4:39
you like having more control with the overrides and everything, yeah, yeah. But the tubeless nature of it meant enough to you that you weren't like, I'm gonna go try a T slim or something like
Jaime 4:50
that. No, I would not. I just, I don't know, never had it. Don't want it. Gotcha, all right, yeah.
Scott Benner 4:55
And then you are wearing a G 6g, 7g,
Jaime 4:59
Six. My son has wore a g7 a few times, and we haven't had a great experience with g7 so far, so I'm sticking with the six. Okay,
Scott Benner 5:07
excellent. All right, so how does your son end up having an experience with T Z? Like walk me through that process. I
Jaime 5:15
knew about screening for antibodies for quite a while, and my son, zad, and I had decided we weren't going to do that, because I figured I would know when he gets diabetes, and there was nothing to do about it for a long time. And then I heard about T Z yield, I think I heard about in the Facebook group. And then I I'm on LinkedIn. I'm connected with a lot of people in the life sciences and med tech industry. So I started seeing posts coming up on LinkedIn, and I'm like, Okay, well, he's yield to her. Like, now we can do something if we find out he's going to get diabetes. So let's do the screening. So I ordered the kits, and then I left the kits in the closet for months. It's like, yeah, I gotta do that kit, but I don't want to do it today. I don't know it's interesting. Like, I've talked to other people, they say they do the same thing, like, you can't actually sit down and do it because you almost don't want to know, yeah, is that
Scott Benner 6:05
it is, what slows you down is that you're just like, Oh, what if it's like, what if they do have antibodies, that's the vibe. Yeah,
Jaime 6:12
yeah, it's a strange block. But anyway, there was a long weekend in January, I think it's Martin Luther King weekend. I was like, Okay, we're gonna do it this weekend. So I sat my daughter down, and it is hard to get the blood out of the finger into that tube, and it went on and on, and we finished hers. She's like, Mom, that was terrible. What do I get for doing that? Like, you can have some ice cream, you
Scott Benner 6:32
know? So you might get diabetes, sweetie, hold on a second. Yeah, just hold on a few weeks. So, and your son's looking over from the corner, going, I'm okay, thanks.
Jaime 6:45
Yeah, exactly. So I packaged it up in the shipping package, and I noticed when I was packaging it up that I put it in the wrong container. I put Ashley's in Carter's container, and you could tell, because of the IDs on a study form. And I mean, this is sort of funny, because I'm an epidemiologist, you're supposed to be, like, protocol driven scientist. Oh my gosh, I can't believe I did that, right? I knew that the study wasn't going to accept them because they're mixed up. Like, that's not how a study works. So I was like, All right, you know, it's too late. I can't call them. I'm just gonna assume we're going to have to do this again, and in the meantime, I said I'm just going to do a fast like a random blood sugar, because I want to see it be normal and I'm going to feel better for the rest of the weekend. So my daughter's like, again,
Scott Benner 7:35
there's no blood mommy.
Jaime 7:39
So I did hers. She was 85 I did Carter's. He was like, 150 something, and they had both eaten lunch at the same time, and it had been about two hours since the meal. And I was like, now I know the screening guidelines for diabetes actually have done research in diabetes earlier in my career. I don't right now, but you know, and I looked up the guidelines at that moment, and I'm like, This is not good, but it's not terrible. So the next morning, I'm like, Hey, Carter, we gotta do a fasting. Alright, Mom, how
Scott Benner 8:10
old is this point? By the way? He's
Jaime 8:13
1414, okay? And at the time, she was 11, all right, I did his fasting, and the first one came back, 126, I'm like, we're doing a second one, something again in the 120 wash your hands. Yeah, right. I know. I'm like, Oh, no. You know, most people with type one are like, that's not too bad. But for screening purposes, you do not want to see something above 100 fasting, yeah. And so I'm like, you sure you didn't eat anything, even when you
Scott Benner 8:41
know your meter might be off a little bit, and you start going, like, okay, let's give it 15% and then you go, Oh, it's still high. Yeah,
Jaime 8:48
yeah, I agree, but still not. I'm not flipping out. I'm not like, oh. So I sent a note in my chart to his pediatrician, and I said, I just did these fasting numbers. Can you please order antibody screening, because we need and another blood test fasting. And she wrote me back and said, I'm going to order the A, 1c, and fasting, we won't order the antibodies right now. The message said, we'll save him some blood. I'm like, No, take all his
Scott Benner 9:15
blood. We won't it's not looking to do it twice, yeah, the
Jaime 9:19
next day, we go to the fasting lab at the actual lab that came back 111 and the A, 1c loaded in my chart. I think it was the next day. Maybe it took a day for it to load, and I saw that it loaded. And at this point I'm 80% thinking Carter has early type one diabetes. Yeah, right. It could be some of our explanation here, but I'm 80% thinking it. So I hovered on that screen. I'm like, Oh my I just like impending doom. When I clicked on it, right, yeah. And it showed 6.4 and I was like, oh, like, oh, no, you know.
Scott Benner 10:01
I knew then, like that moment you're describing Jamie. I had that moment in a 24 hour pharmacy. I stood in front of the meters, and I had the conscious thought, if I never leave here, Arnold Arden will never have diabetes if I don't leave this space. You know what I mean? It's an interesting I understand that. Yeah, today's episode is sponsored by Medtronic diabetes, who is making life with diabetes easier with the mini med 780 G system. The mini med 780 G automated insulin delivery system, anticipates, adjusts and corrects every five minutes. Real world results show people achieving up to 80% time and range with recommended settings without increasing lows. But of course, Individual results may vary. The 780 G works around the clock, so you can focus on what matters. Have you heard about Medtronic extended infusion set? It's the first and only infusion set labeled for up to a seven day wear. This feature is repeatedly asked for, and Medtronic has delivered. 97% of people using the 780 G reported that they could manage their diabetes without major disruptions of sleep. They felt more free to eat what they wanted, and they felt less stress with fewer alarms and alerts you can't beat that. Learn more about how you can spend less time and effort managing your diabetes by visiting Medtronic diabetes.com/juicebox I used to hate ordering my daughter's diabetes supplies. I never had a good experience, and it was frustrating. But it hasn't been that way for a while, actually, for about three years now, because that's how long we've been using us Med, US med.com/juice, box, or call 888-721-1514, US med is the number one distributor for FreeStyle Libre systems nationwide. They are the number one specialty distributor for Omnipod, the number one fastest growing tandem distributor nationwide, the number one rated distributor in Dexcom customer satisfaction surveys. They have served over 1 million people with diabetes since 1996 and they always provide 90 days worth of supplies and fast and free shipping us. Med carries everything from insulin pumps and diabetes testing supplies to the latest CGM, like the libre three and Dexcom g7 they accept Medicare nationwide and over 800 private insurers find out why us med has an A plus rating with a better business bureau At US med.com/juice box, or just call them at 888-721-1514, get started right now, and you'll be getting your supplies the same way we do. So
Jaime 12:50
then she wrote, right away, wrote the pediatrician, said, I've sent a stat order to endocrinology. You know they'll be calling you to set up the appointment immediately. I called Endo. So he's in a very restrictive health plan, like an HMO and a small hospital network. Okay, I know a lot about health insurance, because you have to when you manage prior authorizations with type one diabetes, but his plan, it's his dad's plan, and it's a great hospital network, but it's very restrictive. And in a sense, I didn't mind, because the doctors here are very good, but you can't they usually won't schedule that appointment until the referral is approved. And I'm like, take it first appointment. Like, give me the first appointment. They're like, well, actually, we have one tomorrow at 2pm but you know, you may not be covered because your referral isn't approved. I'm like, I don't care. Just self pay. Just write me self pay. We're coming in tomorrow, so we tell Carter he was at his dad's house. His dad's like, I'm gonna tell him, you know, the results came back and we need to go see a specialist. And, no, actually, it's a little
Scott Benner 13:52
different. Hey, you got a good ex husband. How'd that happen? Most of them would be like, Oh, we get along very well, yeah. He's like, I'll take care of this is a bad thing. I love my kid. I'll tell him, like, Wow. I was like, That's really impressive. No,
Jaime 14:03
and we're all communicating back and forth, I mean, the whole time. And it was actually, I'm very proud of how we did that. Everything was decided together with conversations and discussions. And yeah, no, that day we told him, you're gonna need, that's right, you're gonna need to see a specialist. And he broke down. And my kit Carter is so flexible. Yeah, everyone says, hey, where do you want to go to dinner? He's the only one who wants to go to this one place, and everyone wants to go somewhere else. He's like, That's fine. Never about anything. He's just flexible. He doesn't get upset, yeah, and he got really upset, really, really upset. And I cried. His dad cried, he cried. And we didn't even really know what was going on at that point, but we did sort of know, you know. And it couldn't calm down. It was awful. I said, you know, trying to say some positive things, you know, trying to explain the uncertainty. It didn't help. I'm like, you know? Why? I can go take a shower. Sometimes it helps people calm down. So he did. He sort of took a step away from the conversation, and he calmed himself down. And the next day, he was fine. I mean, he wasn't having a meltdown,
Scott Benner 15:12
right? He wasn't thrilled, but he wasn't then we got it,
Jaime 15:15
yeah, yeah. Then we got a call from the doctor's office, and they said, You guys need to go to the hospital, and we're like, what? And they said, well, any potential type one, the protocol is, you go to the hospital, and I sort of get it, because, you know, most type ones aren't diagnosed in stage two, like he could be in DKA, right, if he's a probable type one. So anyway, we picked Carter up, surprisingly, from school. He didn't know that. Then we were going to go to the emergency room. So we go to the emergency room. They do a whole bunch of tests. And I had read, I was up for hours reading about T Z yield and how we were going to get qualified for T Z yield that night, right? And at the hospital, like, don't do another A, 1c, or or fasting, or OGTT, don't
Scott Benner 16:01
do it, because if he, you need the number they had already, yeah, yeah. I gotcha,
Jaime 16:05
yeah. I'm like, I need that 6.4 if he, if it had been 6.5 it's possible he wouldn't have been eligible. I don't know for sure, but that's the qualification cup point. No one in the trial was above anyone, right? So they didn't. And, you know, it's fast, whatever the random came back high again, and they tested them for celiac that was negative, thyroid was normal. Did a whole bunch of tests, and they ran the antibodies, and they let us know they won't come back for two weeks. And the doctor said, you know, we can't know for sure, but basically, we already know he has stage two type one diabetes. He's eligible for T Z yield. We don't do tea field at this hospital. That same day, we had an appointment member with the at, actually a different hospital, the pediatric endocrinologist, we got the referral to. And I'm like, well, we might as well meet them, because they're probably going to be the ones that figure out the T field situation, not this hospital doctor. So we left and we went to see this other doctor who
Scott Benner 17:03
she's like, Oh, you didn't like this one.
Jaime 17:06
No, I'm no, okay. She She said, Well, you know, it's possible Carter has type one diabetes, but it's also possible he ate a lot of sugary things over the holidays, and that's why his ANC is elevated. Wow,
Scott Benner 17:21
that's a misunderstanding of the human body. Yeah. I was like,
Jaime 17:26
what I mean at that point? I'm like, this, this is our doctor, oopsie,
Scott Benner 17:31
like I knew she's wrong. Are you sure you just didn't have a Mars bar and then eat ice cream and then got a six over a six
Jaime 17:42
days and days every three hours. I mean, what like?
Scott Benner 17:46
So let's say I ate a bunch of sugary stuff and my body still hasn't regulated it. What do we call that? Hmm, let me think. Let me think. Is that diabetes? I don't know. It might be.
Jaime 17:59
Oh, you know, I know kids get type two, but like, he's slim, you know, I
Scott Benner 18:05
Well, how about you have type one? Yeah. I mean, like, come on,
Jaime 18:09
come on. And so I'm like, Well, why was the hospital telling me? Like, this is what's happening. I mean, we're 99% sure, and you're telling me something else that doesn't make any sense. So she leaves the room. She said, I'm going to call the hospital like, okay, so wait. She comes back in and she says, Well, the hospital and I differ on our opinion here. You know, that's all I can say at the time. We won't know for sure until the antibodies come
Scott Benner 18:33
back. Yeah, but I'm super excited to misdiagnose your son, put him on Metformin and watch him and go into DKA. Can't wait to get this going. I love this part of my job. How often does this happen? You know, I don't know. We
Jaime 18:45
get in the car. I'm driving him back to his dad's, and Carter's like, oh, like, I guess it sounds like I might not have diabetes. Yeah. Great.
Scott Benner 18:53
Way to go, lady.
Jaime 18:57
I also said to her, will you let us know the minute those antibody tests come back, because they're going to be in a different system, they don't go into member or two different systems. They don't go into the Yeah. She said, Well, we'll have an appointment in three weeks. I'm like, no, no, no, no, not three weeks. We the second that lab comes back, I need to know, well, I guess you can keep calling me off. I'm like, oh boy. So she's like, the systems don't connect. So then I'm trying to call, where am I supposed to call the hospital emergency room? Like, to get the lab so I I'm like, Okay, I need to get on the my chart of the hospital, because then if I'm on that one, I'll see when the labs come through. And now you're welcome to California law about health records for teens I cannot access his labs. I'm blocked the state of California. Well, this is this hospital's interpretation of the State of California doesn't allow me to view Carter's medical information, so I won't know when they he's
Scott Benner 19:54
14. He could take care of himself,
Jaime 19:58
not only that, Scott, I'm like 10. Mind, then I'll make him an account, right? Or have his account. And I, I was on the phone multiple times with the hospital, like people that manage this record system, and they're like, No, the children can't have access either. They're minors. You don't understand.
Scott Benner 20:13
He's not old enough to have this. He can't have it, and I can't have it. That's great. What kind of system is this? That's great.
Jaime 20:24
So that I call, I find the name of the doctor on the outpatient record. I'm like, I'll call his outpatient office somehow, just to make sure I
Scott Benner 20:31
real quick. Is it Dr Bombay, by any chance is that the doctor's name? Does anyone have a Am I too old? Like, does anyone get my bewitched reference? Right now. It's not a crazy witch doctor. No, no, okay, never mind. I'm sorry. Go ahead.
Jaime 20:45
So I called that outpatient doctor, and they're like, well, he doesn't have a record in the system because you were seen in the emergency room. So I don't know, I can't send a note because there's no record. I'm like, you know, almost crying off on. I'm like, listen, someone needs to be watching for the labs. Like, who's watching for the lab? So that I get the labs, please? I
Scott Benner 21:04
love that she's just willing to wait like, three weeks. Like, what was it going to be a gender reveal? Were you going to, like, hit a pinata when you got there or something? Like, What is she thinking about? Yeah, anyway,
Jaime 21:13
I don't know. So annoying, and I got so annoyed. Then I'm getting annoyed about California health laws. I mean, I was annoyed about enough, you know what? I mean, yeah, after we found out it was actually the day after the eMERGE, the emergency room visit and that annoying post doctor visit, I was like, Okay, I need to figure out every step to get Carter tea sealed. I felt like a warrior. I'm like, it's going to be hard. This is a newly approved drug, right? And it's very expensive, and we're in this limited plan. And from what I can tell, both of these hospitals in the plan will not allow us to get they don't have T cell they can't administer it. It's a 14 day infusion. They don't do it. So I'm like, Okay, so we're gonna have to go out of network. How are we going to do this? Where are we going to go? So I called, and I said, Listen, I called the Health and I need to speak with someone who knows about prior authorization for specialty medications. I need to speak to an expert. And they just connected me with one. And this woman was so nice. She stayed on the phone with me for 45 minutes. We needed an out of network, referral to the facility that could administer the drug. That person who was going to administer the drug had to write a stat prior off, which should have a three day turnaround time. Then, because it was out of network we had, oh, and we needed a referral to that out of network facility with a specified and she told me what had to be in the referral note, like it has to say that we cannot do this at this facility. So that's why we're referring out of this facility, right. There would need to be a letter of agreement between the facility and the health plan, documenting the financial payment terms, because it was out of network. You can't figure that out afterwards, because it's so expensive, so all those things needed to be in place. I'm, like, I got it. We're going to make it happen. I'm going to make all those things happen. And I just, I was so I couldn't stop thinking about getting Carter tea deal. What do we need to do to get teased? But we're we can't do anything until we get the antibody results. Oh, I had to find the facility. So I knew someone at this other facility, nowhere near where we live, and a physician, because I know I know them through looping. I messaged him, and he said, Yeah, we do it here. I'm like, Oh, thank God. So he referred me to the doctor at that facility who did T field. We got an appointment very quickly. I actually wrote the referral letter from that remember that doctor who thought Carter might not have diabetes, I told her what needed to be in the referral letter, the out of network referrals, and I don't trust that she's she's going to know what to do over there, I dropped it off in person like, hi, I need to see this handed to someone who's going to hand it to the
Scott Benner 23:58
doctor case. So I don't know that you're a nutcase. I think you you recognized along the way that there's just too many there's too many pain points, there's too many possibilities for this to go wrong, and then somebody just either drop the ball or just tell you, Oh no, it doesn't work, and not really know the answer. Can I tell you something just real quickly, hold your spot in your story. Okay? You want to hand it to somebody and see them. Hand it to a doctor. Okay, I have to sign something for my bank, and they sent me an email, and it says, Please read this and then sign it, and you open it up and there's nothing there. So I emailed back, and I said, Hi, opened up your document, but there's nothing there. You know, sorry, they resend it, of course, it's exactly the same. I send it back. I say, I'm sorry. It's the same. I opened it up and there's nothing there. I've also now tried three different browsers. That doesn't matter, there's nothing there. They send it back again, no explanation, no like, nothing. Just. Here's a new email. I try it on my phone, it doesn't work. I tried it on an iPad, it doesn't work. I email them back. Now I'm sending them screenshots. This is what it looks like when I open it. Thing that you want me to do isn't there, and she just sends it to me again. And I responded back, and this time I said, whatever her name was. I think I was like Lynette. When I open your document, the thing you want me to review does not exist. I cannot see it. I have looked on my computer, on three different browsers, on an iPad, on an iPhone, it's not there. And she responds back, just click the boxes and hit accept. And I responded back and said, You want me to sign a legal document. But I don't know what it is that doesn't seem like a thing I'm going to do. Here's my phone number. So this morning they called me, and she says, Hey, we just need you to sign that. And I was like, Yes, I know I've been going back and forth with Lynette, but as I explained to her, and I went through the whole thing again, now I'm speaking to a second human being. She says, Well, hold on, we'll resend it to you. And I went, please do not I said, Please, please do not do that. By the way, Jamie, I'm gonna just admit this to you. Okay, because I think it adds to the story, and it happens to be true. I was in the middle of my morning constitutional while I took this phone call. Okay, now I'm like, I'm like, Look, I hold on. This has been going on for two weeks. I go over it with her. No matter where I open it, it's not there. Here. Do you have an email address? I do. Hold on a second. I email her the page. I said, are you looking at that? She said, Yes. I said, That's what I see. There's no information there. And she goes, I swear to God. She goes, just click on the things and hit accept. I said, I'm not signing a legal document that I can't read. First. She goes, Oh, that makes sense. Can you come by? I said, I live 45 minutes from you. I will not be stopping by. And she goes, okay. And I said, if you want, you can mail me a paper copy of it and I will sign that and send it back to you. She goes, Why don't I just tell you what it says? No. I said, You want me to let you read me a legal document, and then me just assume that when I click on these buttons, that's the legal document I'm agreeing to. And she goes, yeah. And I went, you think that's a thing I'm gonna do? And she goes, No. I said, Would you do that? She says, No. And I was like, Okay, now this is a thing, by the way, that someone else had to sign. I'm helping my son with something, right? This is like, very parse, but I'm co signing on something for him, right? And she goes, Well, your son signed it. And I said, he's an idiot. I'm not going to do it, okay? And she's she, and she goes, what? I'm like, He's 24 he'll click on anything you tell him. And I said, Why don't you take this opportunity to send this problem to your IT department? Maybe they can get it fixed. And she says, Well, we've never had this problem before. And I said, it's more likely that you've never sent it to someone before who was like, I don't think I should sign something that I can't read. Yeah, and this has been going on for two weeks. This is signing a PDF with a bank.
Jaime 28:05
Either they're gonna have to get in the car, you're gonna have to get the car.
Scott Benner 28:07
No, no, this is not my point. Jay, that's not my point. My point is those people work at the hospital too, and they work at the and they work at the insurance company, and they work and all I could think while I was doing it was I genuinely I started thinking over the things in my life that involve another person or another entity, and how many times does it actually go well, like smoothly, like the person on the other end understands it? And the answer is incredibly infrequently, you know, right? Yeah, and now you are in the situation where you're like, I'm I'd like to try to get my son this drug protocol that might push off his type one diabetes, you know, diagnosis for God knows how long. And I don't want to leave it up to Lynette at the bank, right? Like, so, yes, when you said to yourself, I was nutty, or whatever you said, I don't agree with you, I think you were probably the exact right level of interested and dedicated. So that's why I stopped.
Jaime 29:05
I mean, I wasn't screaming or crying, you know that's and even then, if you're worried about your kid getting diabetes, you can scream and cry, in my opinion, yeah, I wasn't. I mean, I'm
Scott Benner 29:16
so sorry. You're at the doctor's office. You're holding the document. What happens next? So
Jaime 29:20
they take it. They they're confused. But, you know, no one else just pops up there demanding things like that. But I don't feel totally confident. Then I'm sending my chart messages. Have they seen the file? How quickly is the referral going to be sent below? Like, could you write me back within the next 24 hours? The thing is, this is a time sensitive treatment, right? And I had no idea like but the insurance require another blood sugar check, and then he progressed, and we're too late or something. You know, there's just a lot of unknowns. And this person at the health plan, I won't say her last name, but her first name is Heather. I just in my entire I've had diabetes for 41 Years, and I've dealt with so many prior auths, oh my gosh, especially when everything's gone through medical benefits and not prescription benefits. First of all, that's what prepared me to know what I was doing here, and to recognize that the system is going to be completely messed up. You're going to have to track every single step of the way. But I had this friend, really, at the health plan who checked everything. Oh, yes, I see it in the system. Oh, now it's moved on to the right, and you're going to hear back from this within two days. Hi, Jamie. I just heard back. Here's the result, here's the information, because a lot of stuff would come by mail instead of right, right. Just like a godsend. She even messaged, how's Carter doing after the treatment, just like she's like my friend at this point, Heather. You know, if you have any questions about billing afterwards, I just love this woman. Heather's a good one. If I was just upset, I would call Heather. I'm like, Heather, I can't I'm still waiting. I'm very upset. She's like, it's gonna be okay. Wow. So Oh, finally, at the doctor's office, they're like, we're gonna have someone call you when the antibody results came back. This is the person who's going to call you, blah, blah, blah. I'm like, okay, great. So it was a resident who, that's who we had seen in the hospital, who called me with the antibodies, and he, about a week and a half later, had, that's how long the test takes. Had four antibodies positive, and so he was eligible. You have to have two or more. So everything just sort of worked well for a while. We got the out of network referral approved. We went to the third facility, virtually had an appointment, went over all the questions about T Z yelled Carter during this whole thing, emotionally, is doing fine. He's like, Yeah, we're just trying to see if we can get this drug. And I had a very frank discussion, very long, like trying to understand his feelings, making sure he understood all of the risks and benefits of the treatment. Because his dad and I were like, we want this. There was no question, right? I read the trial results, I read everything about that drug. I read the full label. I understood there were small risks of certain bad things happening, but very rare, usually tolerated really well. But we, I told Carter all of this, there's like, a 1% chance you could have this really weird side effect, that they're going to be taking labs to check it, and you know it's going to delay, but there's not a guarantee it's going to delay. So it's possible that we get this infusion, and it doesn't, it doesn't delay. That could happen, and this is the average delay that was seen in the study, but some people had more of a delay, and some people had less of a delay. What's the average? The study of teas yield was patients who were in stage two, type one diabetes, the people who were in the control group developed diabetes on average in two years. But that's the average. That's not like, Oh, you're going to develop into some were six months, some were five years, right? The average of the control group who didn't receive T yield was two years. The average of people who received T yield was four years. So the delay, it's not a four year delay. It's a two year delay on average. So you won't get the diabetes in two years, you'll get it in four there's a lot of variation. That's just the average, and that's what they're allowed to say on the label, because that's what was found in the study, right? Oh, so I had this in depth conversation with Carter. He asked them questions. I'm like, it's really your decision. You're 14 years old, you know, you don't want to do this. California
Scott Benner 33:19
says, and we're not, I can't see your records, but you're not old enough to see them either. But anyway, we're gonna let you talk about this. Go ahead. What do you think? Did he talk it through with you? Like, what was his process?
Jaime 33:31
Yeah, he asked a few questions. He wanted to know. Like, how does the infusion work? You know, you say infused, they don't. There's actually two options. You can have sort of a permanent thing put in your permanent, I forget what they call it, similar to what you get for cancer treatment, like fistula, maybe, or, I can't remember what it's called anyway,
Scott Benner 33:51
they can put a port in and then every procedure,
Jaime 33:53
yeah, right. And then you don't have to get stuck every day. Or you can, you know, get an IV every day, and you have a choice there, and they'll go over that more at the hospital. And after the whole conversation and discussion, he's like, Well, worth a shot. And that was it. I love it. That's like, Carter's flexible attitude is worth a shot.
Scott Benner 34:16
That's excellent. So he does it. He ends up doing it. Well,
Jaime 34:20
then we get to the real stick, sticky point. Okay, the letter of agreement between the facility and the health plan, everything that went through, all said that was the last thing we needed. And that negotiation went on and on, and I was getting no updates. First, the doctor from that facility, where he's going to get it, was communicating with me by my chart, it's in progress. So like, two days later, I'd be like, Okay, is it done? Jamie, all I can tell you is that it's in progress. I'm like, can you connect me with the person who's actually working on this at the facility? No, we manage the communication with the patient, because we're the doctor. I'm like, That's not acceptable. So I call the infusion center. I want
Scott Benner 34:55
to say also the way he's the way he's managing it is by saying they're telling me it's in progress. Yes, that's probably all they know,
Jaime 35:04
too. The doctors not doing anything. It's billing. People managing this, right? So I call the infusion center, and I get some nurse and they're like, oh, yeah, I know that case is going on, and they're working on it, but you know this, it's really expensive. They got to sort out all these costs that the whole therapy could end up costing a million dollars. I'm like,
Unknown Speaker 35:26
a million dollars. Did
Scott Benner 35:28
they say it like in that cartoon? 1 million. Was it like that or no,
Jaime 35:34
no, it was like a horrified sound. I do believe this went on and on. Finally, I did get connected to a billing person? They're just saying the same thing. I'm like, well, we met again, and we're supposed to meet in two days, and this went on for three weeks. I'm like, what has happened? What have you decided? Are you making? Please explain the progress you're making. Well, we're just meeting. We're just meeting to go over the points. I'm like, This is nuts. So I contacted a friend of mine who's a health attorney, and talked with her for like an hour, and she gave me some tips about what to say, and I said them. Basically, there's a state agency that you can send complaints to when care is being delayed inappropriately, if you think it's inappropriate, right? So first you have to file a grievance with the health plan, a grievance with the facility. And then once you've done that, you can report to this state agency. So they had, like, the billing person's like, manager who it was a very senior title, VP of blah blah blah at the facility, ended up calling me one one day because I was so annoying. They're like, please, don't worry, this is in progress. It's going to be resolved soon. And that was right after I talked to the lawyer. I'm like, listen, I do not believe you that this is going to be resolved soon. That's nice that you're telling me that, but this is what's going to happen if this isn't resolved by Friday, I'm filing a grievance with your facility. I'm filing a grievance with the health plan. And then after the grievance, it's going to go to the state agency for investigation, if it's not done by Friday.
Scott Benner 37:06
Used all the magic words at once. Used them all up.
Jaime 37:09
Yeah, used them, yeah, yeah. And then that's how Teasel got approved. The next day, I got a call. That is it? 24
Scott Benner 37:15
hours later, yes, yeah, I love peanut butter sandwiches. Ah, yeah. No problem. Here it is. Turns out it's not a million dollars Crazy, right? Here you go. Oh, their job to say no to see if you give up, you know.
Jaime 37:31
So then we rented an Airbnb, and we went up there and we got tea sealed. And, I mean, it was smooth sailing. We just got the infused. He didn't want a permanent thing in him. They used something called the J tip on the insertion to numb the area. So he said he didn't even feel when the infusion was going in Nice. He did have somewhat hard to find veins, but they have a special it was a pretty advanced hospital where he got the infusion, and so they had everything. They had some special team that could find, hard to find veins, and he was totally calm. And it was, I look back at it like a medical vacation. We went to a nice area in the morning. We went to the hospital. We played poker, mostly during the infusion. And I didn't get to spend, I don't spend time like that with Carter, like he's 14 years old. He's doing his own thing a lot of the time. It was hours days of just meeting Carter. I was there for the first 10 days, and then his dad came up for the last four and I came home, we did that. And then the afternoons, he felt fine. We went to museums. We went hiking. It was amazing. Nice.
Scott Benner 38:34
That's excellent. After the that process happens, he gets the 14 days of infusions. What's the follow up? Like, like, how do you keep track of this? Did it work? Is it working? Like, agree, how long until you just forget about it and just hope it works for as long as it does, there's
Jaime 38:51
actually no indicator. You can't tell, like, oh, is is it gonna work? There's nothing you don't, like, get a test and they're like, Oh, it worked. It's gonna delay. You just keep monitoring the blood sugar. So his a 1c in January was 6.4 it was done about six weeks after the infusion again, and it was 5.4 with a normal C peptide. Now, the other thing about stage two, it could have been the impact of T seal, but also stage two sort of goes up and down like your your insulin levels get better, get work. Yeah, it's not necessarily, apparently a linear thing, but we're thrilled with the 5.4 he's also taking, I did some research on vitamins that might help delay so he takes those. And his doctor definitely recommended the follow up doctor that we're seeing here now, we found a really good one, and I like him a lot. So he takes fish oil and vitamin D, as recommended by the doctor, and then he also takes zinc and a B complex with C. I decided the C and the Zinc because of immunity. You know, you don't want to get sick like that's part of what kills the insulin cells. You get the flu, you get. Yeah, a cold, yeah, right. Those are sort of to try to keep so he takes those and I trying to limit the carbs. The doctor also recommended a lower carb diet. Some research that may be helpful. It's not super strong, but we didn't really drink, you know, juice or soda. But those are also you there's no sugary beverages allowed, so
Scott Benner 40:20
Well, you might as well try everything you can think of, right?
Jaime 40:25
Yeah, and he wears a CGM, like, one cycle a month, and because it could just boom progress, right? And you don't want to end up in DKA, so that's why you keep doing the a one CS every three months. And he wears a CGM, but he doesn't have to wear it all the
Scott Benner 40:39
time. What's the timeline on this from the time you thought, hey, he might have diabetes, until the infusion started? And how long has it been since the infusions were done,
Jaime 40:50
the end of January, when it all started, and then the infusions were mid March?
Scott Benner 40:56
Wow. You've accomplished all this basically in the last eight months. Yeah, it's been a lot. I imagine he's doing great. Yeah, excellent. Your company was good with you taking time off to go away, yeah. So I took
Jaime 41:09
FMLA, okay, so because it was more than five days in a row, I guess it would have been sick time only less than five days. But because it was continuous for that long, I just had took FMLA, and so I was able to do that. So part of it was unpaid, but that was okay for me, right? Well,
Scott Benner 41:25
the big parts like they, you know, not that they're just gonna fire you, but you know you've got your job when you come back and you know they can't. Oh, yeah, yeah. All that 10 days is pretty short, but FMLA is pretty cool about what it protects people from, especially when you're It is, yeah, fighting an illness like that. Have you guys had any conversations about diabetes now? Or are we, like, just gonna act like it's out of sight, out of mind for now? Like, where are you at with that?
Jaime 41:52
So especially when we were doing the T field infusion, it was like, a lot of focus on diabetes, right? We're here to prevent diabetes or delay diabetes, and so it was just on our minds a lot. So during those 14 days, we had a lot of conversations about diabetes. It was probably pushed more by me. I'm like, I want to get some of this info out there, you know. And one of the most interesting conversations we had, we talked about, like, symptoms of low blood sugars. And by the way, he does have some low blood sugars, but he feels no symptoms. So I'm a little puzzled by that, but that's the doctor said, Yes, you can have more lows in stage two type one diabetes, as well as the highs, because your glucagon production is a little bit off. Your body's releasing too much insulin at certain times. So, but for whatever reason, he feels no symptoms of them. Okay, I don't know, we talked about the insulin pump, like I showed in my loop, you know, showed, hey, this is what I do, and this is how the screens work. And I showed him night scout. Here's some of the data I look at to see how my trends are doing. I'm like, but there's lots of different options out there. And, you know, for many years, I just use needles. Or it's like, I think I want to use that thing. It's cool. You can control it from your phone,
Scott Benner 43:00
you know, like, Wait, it's got an app I'm in,
Jaime 43:05
right? Can I play? The one conversation I really wanted to have with him was about, you know, when teens developed, I Well, really, anyone there can be, like, a rebellious stage or a time period where you're not going to pay attention, and for whatever reason, it's my personality or how my parents raised me, or what I've never had that I never was like, Oh, I'm going to eat this and forget about it. I mean, make mistakes, whatever you forget. But I was never overtly, I'm not going to manage this closely. I was always like, this is very important, and I want Carter to feel that way, right? But how do I make sure that he feels that way? How can I encourage him to feel that way? So I just posed the question to him in this conversational way, like, hey, you know, sometimes, especially teenagers, if they get diabetes, they they don't pay attention to it, and they maybe they don't take their insulin, and they get really frustrated or mad about having diabetes, and they stopped paying attention to it. Like, what do you think about that? And it just allowed us to have a conversation about he's like, why would they do that? I'm like, Well, I don't know. Why do you think they might do that? Well, I guess just because you don't want it and maybe you can ignore it. I'm like, yeah, absolutely, it makes sense. But what's the implication of doing that? Right? That was one of the most interesting conversations I had with Carter, and one of them that I felt was really important to have. Okay, yeah,
Scott Benner 44:32
well, He'll either have it happen to him and he'll be like, Oh, this is the thing my mom and I were talking about. I still don't feel like taking care of this. Or, yeah, it'll creep up and he'll think, oh, okay, yeah, this is a thing to look out for. I'll get ahead of it somehow, and hopefully he'll be able to
Jaime 44:48
it's interesting wearing a CGM, because he can see how certain foods, you know, affect blood sugar. Obviously, when he gets type one, he'll need to take the insulin to match the foods, right? Right, but it's funny, the worst blood sugar, I actually texted his dad. I'm like, hey, what Carter eat at like, three o'clock yesterday? His dad said, blueberries. I'm like, blueberries, sugar. When Carter came back, I'm like, hey, that's fine. Did you notice how your CGM spiked up? He's like, I didn't notice. Like, okay, well, the worst was, like, 3pm the other day you were eating blueberries. He's like, Oh, yeah, I ate the whole container. Also,
Scott Benner 45:23
I am not looking at the CGM, in case you're wondering, right? Well,
Jaime 45:26
his high alarm is off. What's he going to do about it? Right? But it's just interesting to learn that. And so we have a new role of pairing carbs with protein. I'm like, you want to eat the blueberries, you got to have a piece of cheese or the nuts or something
Scott Benner 45:41
to slow this down a little bit, fair enough. And he, and he's, and he's flexible about it. As you go,
Unknown Speaker 45:47
yeah, he seems to be, yeah. Can
Scott Benner 45:49
I ask you? I mean, you're the type one, right? So, and you're of the parents. Do you have any feelings of guilt or strange, like psychological impacts from what's happening to him.
Jaime 46:03
I don't feel guilty at all. I had a thing happen where I was feeling so bad, just bad that Carter. This was happening to Carter, and it was when he got really upset that week. He so he does his own laundry, and I, I did his laundry that week, and he comes home. He's like, Mom, why did you come and dads? He's like, Mom, why did you do my laundry? I'm like, Well, you know, you're, you're getting diabetes. I just, I just want to do something, you know, extra for you. And he's like, Well, you have diabetes too, Mom,
Scott Benner 46:34
you should have said, yeah, do my laundry. Why are you helping me? Like, why have you been doing my laundry? I think the question here is, how come you have not been helping me with the laundry, right? So okay, that was interesting. I get your feel
Jaime 46:45
guilty i And also, like, when I think about my diabetes, I mean, I hate it. I wish it was gone. I'd be thrilled, but I wouldn't be who I am without growing up with diabetes. I wouldn't know who I would be. I it's part of me like it's who I am. And yes, I would get rid of it in a second, but that's how I feel about my diabetes. And I think the reason I don't feel guilty is a little bit because of how I feel okay about having my own diabetes. You know what I mean? And I don't actually feel that Carter will have complications. I have none. I feel very healthy. I'm very active. It's because I take care of myself really carefully and maybe a little bit of luck. I don't worry about Carter's physical health. I worry about his mental health. And I feel that growing up with diabetes now, in a sense, is very, very different than it was when I grew up with diabetes, because of all the constant monitoring we didn't have that. You had no idea what your blood sugar was running around like, you felt low. You ate two candies, and off you went again. Like, so it wasn't in your mind. You were also
Scott Benner 47:54
using regular and mph, right? Regular
Jaime 47:56
and mph, yeah, not too many shots a day. Like, in a sense, it it was in the background more than I think kids and parents anyone with type one lives today. I don't know. And maybe that's just me. Maybe that's me, I don't
Scott Benner 48:09
know. Let me offer a different perspective. You got diabetes at a time where they expected your life was going to be shorter, and this was the best they could do for you, so they didn't really pay attention to it. And then you got lucky, because at the end of the 80s, when the faster acting insulin came, you got scooped up. But if you would have been diagnosed in 1963 what you'd be saying right now is completely different. You know what I mean,
Jaime 48:31
that's true, yeah, that's true. And somehow, I was treated at Jocelyn Diabetes Center as a kid, so I had the best treatment there was in the country, right? Yeah. And
Scott Benner 48:41
still, the best treatment there was in the country was, shoot this in the morning, shoot this at night. And if you get dizzy, have a piece of candy, right, right? What I was going to say then is, the rest of it is, I've seen this over years. I mean, people who are kind of like, you know, have had type one for a longer time, or got diagnosed long ago, or, you know, had a kid that was diagnosed back before there was monitoring and everything. And they always say, like, they say exactly what you said, Oh, we just ran around. If we got dizzy, we ate something. It was fine and blah, blah, blah, but you don't really know if it was fine and it wasn't fine. Yeah,
Jaime 49:15
I'm sure we were high and we were low, but it didn't affect our mental capacity. You see, yeah, maybe yeah, gonna cause complications later on.
Scott Benner 49:23
But Right, right. There would be some people who might call that blissful ignorance. But now you have the opportunity, sense, yeah, yeah. Now you have the opportunity to, if you want to manage this out to the nth degree, if you want to, and then at least it puts it in your hands, and you can decide, I think that's, you know, the option is there for people who can't handle it for reasons of, you know, stress or whatever, they'll find a different way to manage but I like that the opportunity is there for the people who want it. Yes, yeah, that's all. Anyway, I think that's interesting, by the way. I didn't mean to say that. I think you should feel guilty. I. Was just, I've spoken to people who do, and I was oh, no, yeah. I know. I don't. I do feel very I felt sad, yeah, no, of course, yeah. The stuff I feel sad about for my kids, you know that aren't a life altering disease. I still feel sad for things all the time, you know, experiences that they have, but I was like, Oh, I wish I would have went differently for them. Or, you know, I wonder why this couldn't happen. Or, like, Yeah, I mean, that's just being a parent. That part's that ain't going away. Is there anything that we haven't included in your story that we should have? I want to make sure that this is a nice, tight bow for you, and everything's here. I think we covered most of what I wanted to talk about nice. Well, do you want to, like, flip back around for a second and give people a little more? Because when you first signed up, you signed up to talk about FMLA. Oh, yeah. What did you want to talk about? About that? Like, because we can include that here in the last couple minutes.
Jaime 50:52
So I use FMLA for Carter's treatment, right? But I have both type one diabetes, and then I have a neurological disorder called dystonia. Meant a lot of years I had terrible pain in my neck, but I had scoliosis as a teen, you know, founder and screening, I had an injury as a teen my neck, a sweating accident, right in my neck, and then I had a car accident in my early 20s, when I was in college, and about six months after the car accident, terrible pain. And for years that I'd go to the doctor, this pain is so bad and like, well, your muscles relax and take some Advil, go to pt. It didn't, it wasn't making any improvement, like, only a very small improvement. And finally, after this, having this pain for like, 15 years, I was diagnosed with dystonia, which is a very rare neurological disorder, and there's a treatment for it, Botox, and the other similar medications, similar to Botox, that's injected about every 12 weeks into the muscles by a neurologist. For years, my neurologist told me, I don't use it for diabetes, but I just want to explain the situation so other people understand how they may be able to use it for diabetes, for ongoing, chronic health issues, right? I don't feel the need to use FMLA for diabetes, but for my neck pain. For years, my neurologist told me, Jamie, what's going to reduce your neck pain the most is working less at the computer. And I would just sort of laugh, like, that's funny, right? I'm the primary breadwinner in my family. I make two thirds of the income in my family. It was just a funny thing to me, like, what are we going to do move out of our house if I work less than a computer,
Scott Benner 52:23
you know? Yeah, maybe we could eat every other Thursday.
Jaime 52:27
I don't know. I just, I never did it. And then the pain was getting worse, and I was felt like it was really affecting my mental health to be in pain. So, yeah, standing at the computer, I stand and I sit, but the end of the day is the worst, because I've been there for eight hours, you know? And then that's when you interact with your family and you're in a bad mood because you're in pain. And finally, I'm like, You know what? I'm going to try to work less. Now, the type of job that I have, no one works part time. No one, right? It's not an industry where I work for a big publicly traded company, I have a pretty senior job, senior director level. You can't be like, Hey, can I work part time? They'd be like, What are you talking about? No,
Scott Benner 53:09
you could quit or go to hell.
Jaime 53:13
I mean, no, your job's a full time job, but FMLA covers 12 weeks per year of leave, and you can use it intermittently. So I talk, you know my doctor again, Hey, Jamie. I'm like, You know what? Yep, let's do it. He's like, Well, I really think it should be two days. I'm like, that's not going to cover that. I can't take two days a week because the FMLA is going to run out. So you can take one day off a week every year and use FMLA. Okay, so I'm like, well, write it for one to two and off we go. And I talked to my manager, and my manager said, you know, they just referred me to an outside company, you know, reviews the FMLA form. Here's the form. And I debated that too, Scott for so long, just even doing I'm like, I felt like a failure. Like, why can't I work? Why can't I manage this and work full time? And right? Am I limiting my whole career? Like a lot of my identity is, is associated with, like, doing the work that I do. It's very important to me. I like it a lot. It's like part of who I am, you know. So I almost felt like I'm failing, or I'm failing or not able to progress in this important way, like maybe this is going to limit me in the future. But I just ended up deciding I don't care. I can't be this uncomfortable all the time. And so that was it. It was approved in one day. And I don't work on Fridays. Yeah, my calendar is blocked, and that's it. So, you know, for diabetes, it would be the same thing. You can also use ADA for diabetes, because it's covered as a as a disability under ADA. So if you need accommodations in that way. Right? As I understand it, FMLA actually has slightly stronger protections. If all you need is is just one day, which is what I'm using right now per week. You can use it by hours. You can use it to they have to accommodate. If you have to take your kids to a doctor's appointment at 2pm they have to let you go, you know, yeah, you have to. If they're not letting you go, you use FMLA, you have to, right? I've had no pushback at all. And every six months, the form gets filled out again, and off we go. Well, it's interesting.
Scott Benner 55:28
I appreciate you sharing that as well. Thank you. Yeah, this was lovely. I appreciate you doing this. Have you heard from other people who have done t, z yield, like, has the process been as disjointed as yours was?
Jaime 55:40
So actually, I should there's a Facebook group called Tea sealed families, okay, and it's grown a lot. There were a few 100 people in it when I joined in January, and it's grown by hundreds. It's in the 1000s now, I think. And so you can join there and ask questions that people are really helpful about, you know, answering them. People post their their pictures of their kids and the treatment, and, you know, say how the treatments going. People do have trouble. I think I had a lot of trouble because of the type of health plan that we were in. So why is there so much trouble with this treatment? It's an infusion. Endocrinologist, don't do it. Infusions. There's no infusion an endocrinologist does. So this is like, the first time of this type of treatment for the entire specialty. You know, that's weird. It's also 14 days in a row, and most infusion centers are closed on Sundays. They've got to figure out some way around this Sunday closure, which isn't always easy to do. So I don't know. The drug has some challenges in terms of administration and how it works, yeah, yeah.
Scott Benner 56:45
Well, hopefully as time goes on, they'll stream better streamline it. Yeah, that's interesting. Okay, all right. Well, hey, Jamie, thank you so much for doing this. I really do appreciate it. Yeah, thank you, Scott. Well, it's my pleasure. Can you hold on for a second? You thanks for tuning in today, and thanks to Medtronic diabetes for sponsoring this episode. We've been talking about Medtronic mini med 780 G system today, an automated insulin delivery system that helps make diabetes management easier day and night, whether it's their meal detection technology for the Medtronic extended infusion set, it all comes together to simplify life with diabetes. Go find out more at my link. Medtronic diabetes.com/juice box. Us. Med sponsored this episode of the juice box podcast. Check them out at us med.com/juice box, or by calling 888-721-1514, get your free benefits check and get started today with us. Med, hey, thanks for listening all the way to the end. I really appreciate your loyalty and listenership. Thank you so much for listening. I'll be back very soon with another episode of The Juicebox Podcast. Are you starting to see patterns? But you can't quite make sense of them. You're like, Oh, if I Bolus here, this happens, but I don't know what to do. Should I put in a little less? A little more? If you're starting to have those thoughts, you're starting to think this isn't going the way the doctor said it would. I think I see something here, but I can't be sure. Once you're having those thoughts, you're ready for the diabetes Pro Tip series from the Juicebox Podcast. It begins at Episode 1000 you can also find it at Juicebox podcast.com up in the menu, and you can find a list in the private Facebook group. Just check right under the featured tab at the top, it'll show you lists of a ton of stuff, including the Pro Tip series, which runs from episode 1000 to 1025 Hey, what's up? Everybody? If you've noticed that the podcast sounds better and you're thinking like, how does that happen? What you're hearing is Rob at wrong way recording, doing his magic to these files. So if you want him to do his magic to you wrong way recording.com. You got a podcast. You want somebody to edit it. You want rob you.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#1431 Peter Thompson, PhD - T1D Researcher
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
Pancreatic islet biology and Diabetes (link)
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Welcome back, friends. You are listening to the Juicebox Podcast.
Today we'll be speaking with Pete Thompson. He's a PhD at the University of Manitoba. He's an assistant professor at their max ready College of Medicine, and we're talking today about type one diabetes research. Nothing you hear on the Juicebox Podcast should be considered advice medical or otherwise, always consult a physician before making any changes to your healthcare plan. I know this is gonna sound crazy, but blue circle health is a non profit that's offering a totally free virtual type one diabetes clinical care, education and support program for adults 18 and up. You heard me right, free. No strings attached, just free. Currently, if you live in Florida, Maine, Vermont, Ohio, Delaware, Alabama or Missouri, you're eligible for blue circle health right now, but they are adding states quickly in 2025 so make sure to follow them at Blue circle health on social media and make yourself familiar with blue circle health.org. Blue circle health is free. It is without cost. There are no strings attached. I am not hiding anything from you. Blue circle health.org you know why they had to buy an ad. No one believes it's free. I'm having an on body vibe alert. This episode of The Juicebox Podcast is sponsored by ever since 365 the only one year where CGM that's one insertion and one CGM a year. One CGM one year, not every 10 or 14 days ever since cgm.com/juicebox
Peter Thompson, PhD 1:51
My name is Peter Thompson. I'm an assistant professor in physiology at the University of
Scott Benner 1:56
Manitoba. Peter, welcome. I appreciate you doing this for me.
Speaker 1 1:59
Fantastic to be here. Thanks a lot, Scott for the invitation. Oh, it's
Scott Benner 2:03
a pleasure. You know how you ended up here, right? Yeah,
Speaker 1 2:06
I have a little bit of an idea. I think it's really fantastic that you've got a lot of Canadian subscribers, and they think that the work you're doing on the podcast is really amazing. It's been game changing for them. And so, you know, they put the bug in my ear about this, and I think that's how I got here, right? Am I can correct me if I'm wrong on that? No,
Scott Benner 2:24
that's definitely right. I got the messages. I got the emails. Should I call you? How do you like to be referred to? Dr Thompson, Peter, what do you expect?
Speaker 1 2:32
You can call me Pete. Peter, I go with either of those. Don't call me Dr Eddie.
Scott Benner 2:38
I'll stick with Pete, because that's the first thing you said, Good. Tell me a little bit about your background. All
Speaker 1 2:43
right. So basically, for me, I been a researcher for now about five years. I got started doing my research training in Alberta. So if you're familiar with things like the Edmonton protocol on islet transplantation, I did a lot of my training in Edmonton at the University of Alberta, and then I moved to Vancouver, and I did a doctorate there. It was actually not until later on in my training that I did a research fellowship. So, you know, this long, convoluted route that we take in order to become academics involves, you know, doing all these degrees, but then you have to do sort of an independent, mentored research training stint called a postdoc. So I did a postdoc in the University of California, San Francisco, and that's really when I got into the field of doing diabetes research. So So yeah, it's been a long journey.
Scott Benner 3:34
Yeah, no kidding. Time wise, how long is that journey? I hate to say
Speaker 1 3:38
this because it's I don't want to dissuade young people from picking up a career in science their research in this way, but bachelor's is four years. Masters was another two and a half, and then PhD was five. So we're looking at about that's, I guess, 12 years, and then my postdoc. So about 16 years of total time from bachelor's and undergrad, even in college, to being a researcher, research professor,
Scott Benner 4:01
yeah, well, that's a lot of dedication to get to something. So what drew you to put that much effort into something? Why this?
Speaker 1 4:07
Yeah, you know, I've always been a really curious person. I love understanding how things work. I've always been curious about nature and understanding the world around us. I've been involved in science for pretty much as long as I can remember, from, you know, having my first sort of science kits at home as a kid, to doing science research as a as an undergrad student, and then continuing in it. You know, I think I always felt like I could do something in science, but it's really something that you have to do in community. It's something that you get mentorship for. It's something that you need people to believe in you in order to do well and to move ahead and to keep going. And so, you know, I think everyone has those times in your life where you just feel like, oh my gosh, what am I doing? Am I gonna continue being able to do this? Or am I just gonna throw in the towel? And you know, I had a number of those times during my training, but I always had people to kind of bring me back. Fan. Family Members, good friends, mentors who were further along than me in the road and could say, hey, no, you're gonna you're gonna make it. Keep at it. And they saw the potential in me when maybe sometimes I didn't see that in myself. So you know, I owe a lot to you, the people who've shaped me in that way. And I think everybody, in some ways, kind of a product of of the the people that are around them. So really grateful for that. That's
Scott Benner 5:21
wonderful. So as you're going through the process, how do you hone in on diabetes? Like, because I imagine in the beginning, you didn't start off thinking, I'm going to be a researcher for diabetes, right?
Speaker 1 5:31
That's right. Yeah, I, you know what, I didn't really know much about diabetes again, like I said, until much later in my training. I think it was during my my PhD, and as I was studying, we were working on sort of fundamental questions about how cells make decisions. And some of these questions are things that have been studied for many years, but some of some aspects of them are things that we really just only recently had the technology in order to develop and think about more critically. And so it was at that time I was thinking like, you know, okay, do I want to be kind of studying these things, you know, in a very abstract way, where I really don't know if this is going to really move forward. And, you know, you talk about, when people talk about stem cells, there's a lot of excitement around, you know, being able to develop new therapies for all sorts of diseases. But the work I was doing at the time was very, very fundamental. It's very, very like, hey, how does a cell turn on this gene? How does it turn off this gene? Things like that. And so it wasn't something that I could see being directly relevant to, you know, how people live their lives. And, you know, treatment for disease. And people would often ask me, oh, what do you do? And I kind of have to try to make up some sort of explanation that made sense. Because, you know, to me, I was like, Well, this is interesting from a scientific perspective, but maybe no one else in the world really care about
Scott Benner 6:47
that. I'm trying to pay for this degree, is what I'm trying to do.
Speaker 1 6:52
It was, it was a process. And then, you know, during my research fellowship training, that's kind of when I made that decision. I thought, you know, okay, what are, what are some, some ways, or some questions that are out there that, you know, if we had a bit of a sense of what the answer could be, you know, maybe that could really unlock some doors, and it could, it could actually help somebody. And I really, I started, I guess I don't know, maybe existential crisis sort of thing, where you just think, what am I doing? What's my life about? But I had that point at that time in my training, and I felt like I really needed to do something with a medical focus. And so I, I was thinking about going into either cancer or diabetes, and I have people in my family who have been affected by both of those diseases. And so really, you know, personally, I saw that the person side of both of those, you know, in terms of making a decision, I was really drawn to diabetes because of some of the things I started to learn, especially about type one and, you know, to me, I think, I still think that, when I was learning about this, it's just shocking to realize that, you know, in the history of what has been done for type one diabetes, you know, you go back over 100 years now, And we're still using what was at the time expected to be a stop gap measure. It was expected to be something that could help manage the disease, not something, of course, that was ever envisioned to be something that was like the end game of this is all we're going to be able to do. And, you know, 100 years later, of course, we've made a lot of advancements in a lot of different ways. I don't want to undercut that, but our mainstay therapy for feeding diabetes. Type one diabetes is still insulin. And I just found that staggering. I don't know of any other branch of medicine or disease based investigation where, you know, we're still using something that we used 100 years ago. You just think about that, right, like so that to me. I think that really stuck out to me. And as I started to dig deeper, I realized that, you know, there's a lot of there was a lot of puzzles, there's a lot of things, mysteries that we don't quite fully grasp yet around type one, when I started getting to the field, there was a bit of a renaissance happening. So there were a lot of focus, moving away from just thinking about type one as an auto immune disease and just saying, well, we need it. We need to fix the immune system, starting to think about the pancreas and what's happening to those cells that get targeted in the pancreas, the insulin producing beta cells. So there was a lot of things going on at the time, but I guess that kind of maybe summarizes some of those things for me that were really impactful.
Scott Benner 9:12
I have to be honest with you, I've asked that question of a number of people. This is the most complete and thoughtful answer I've gotten so far. And I've been doing this a very long time, you'd be surprised. Some people are just, I think the wind blew one way, and they ended up as an endocrinologist. It is interesting. Some people it's, you know, family background, or, you know, like I was trying to help myself. I do find that there are people who have diabetes who end up in health care. It's almost like they're maybe subconsciously trying to help themselves. You know what I mean. Like, there's Yeah, but that's a real Thank you, Pete. I really appreciate that. Like, as you were talking, I was like, I finally got, like, a clear answer on that one awesome when you finally find a place to work, do you come in and do you decide I'd like to try to work here because I like what they're doing, or is it more about finding, like, pay. Lab space where you can try a thing you want to try, like, how do you go on day one? How do you get started? This episode of The Juicebox Podcast is sponsored by ever since 365 and just as the name says, it lasts for a full year, imagine for a second a CGM with just one sensor placement and one warm up period every year. Imagine a sensor that has exceptional accuracy over that year and is actually the most accurate CGM in the low range that you can get. What if I told you that this sensor had no risk of falling off or being knocked off? That may seem too good to be true, but I'm not even done telling you about it yet. The Eversense 365 has essentially no compression lows. It features incredibly gentle adhesive for its transmitter. You can take the transmitter off when you don't want to wear your CGM and put it right back on without having to waste the sensor or go through another warm up period. The app works with iOS and Android, even Apple Watch. You can manage your diabetes instead of your CGM with the ever since 365 learn more and get started today at ever since cgm.com/juicebox, one year, one CGM, yeah,
Speaker 1 11:13
great question. I think there's a lot of different ways to get started. Most of the time, though, you have to really reach out to established researchers that have a program in the area of research that you want to study, and see whether they're willing to sort of mentor you and take you on and help you to get to where you want to go. So you know, I guess the main thing is that this time in your training is really supposed to be a springboard. It's supposed to help you get to that next step. A lot of people will do their research fellowship, and then they'll, they'll want to get an academic job. Other people will want to do, you know, an industry job, go into, into pharma, what have you. There's lots of different directions you can go, and you really want to try to target or find the right sort of environment and the right sort of research that's going to help you to get to where you want to go. And you know, to be honest with you, I mean, I didn't necessarily know that I wanted to focus on this really sort of niche area in type one. I just was really excited and really intrigued by some of the things I didn't understand. And I was kind of coming in as a newcomer and an outsider to the field a little bit, you know. And I would sit in these seminars as I started, getting started, I chose a lab, and the lab was, at the time, mainly focused on type two diabetes, but they had a lot of projects were kind of overlapping. And I remember the, you know, the first day, I sat down with my mentor, and he was saying to me, yeah, we're gonna, we're gonna get started. And I had been in conversation with him over a long period of time, and then he says to me, you know, you wanted to start. You, I initially thought, okay, diabetes. I really didn't know a lot about type one versus type two, so I just thought, Okay, we're going to work on something related diabetes. And he's like, Well, you know, you came in here wanting to work on type two diabetes or something along those lines. We're not going to do any of that. I just feel like, like, my gut just dropped. I'm like, oh my goodness, I've invested so much time and effort in this process of finding a lab and getting this position, and I moved my family from Vancouver all the way to San Francisco, you know, we had two little kids, my wife and I, I'm like, Oh, my goodness. Like, so you're telling me now that we're not going to do what I I signed up to do, you know? And it was really a jaw dropping moment. And then he says to me, Well, you know, what do you think about type one diabetes? You know, anything about type one I said, Well, goodness, no, I don't know. I don't know, really, anything about anything. So anything is
Scott Benner 13:23
new to me. Yeah, I was here to find out about type two diabetes. But okay, yeah,
Speaker 1 13:28
so it was a, I really look back on that moment and I see how what could have been, like, okay, oh, my goodness, I'm done. I should just, you know, get out while I can, like, just try to find another position here. Because, you know, now I'm not gonna be able to do it. Yeah, that. Or I could say, hey, well, maybe, maybe there's something here. Maybe I should, I should pursue it further and just look into it at least. And, and so I'm, you know, I really thankful that I did, because I would not be where I am today if I hadn't stayed in this lab. And, and it was, again, like I said, it was a confluence of all these different factors, where the field was going in general, and then we're glad that I chose to do my fellowship training in where they had decided to go, and my mentor was saying, you know, yeah, we want to start moving into tech one. And we think there's some really cool concepts that haven't been explored and all this stuff. So it was, yeah, there's definitely some serendipity there. I'll say that. Is
Scott Benner 14:20
there any, in hindsight, understanding of why the mentor made the shift?
Speaker 1 14:24
I've looked back on this a lot, and I've thought, I've tried to think of, you know, was there anything that he kind of had a sense for? You know, he's a type of guy that I think reads very deeply. He reads a lot of things, he attends a lot of seminars, and he picks up information. I think other people might not see any value. And so I think he probably had been, sort of had some ideas brewing and cooking for a while. But, you know, then when I came to the lab, is like, Okay, I've got, you know, someone new to train. And who can I get to work on something that pretty high risk. But you know, if it pays off, it could, it could go, it could go pretty far. And so I was willing to take a risk. I took a bit of a gamble. And. Pete off there. I think he's
Scott Benner 15:01
thinking, Liz Peter guy is he's screwed. Basically, I just drug him across the country, and he's got his he can't even say no. He's gonna have to say yes. I think
Unknown Speaker 15:10
some of that entered into the equation for sure. Yeah.
Scott Benner 15:12
He's like, Finally, I got a sucker here to work on this new thing for me. Totally. It's awesome though. Like, look where, like, you know, so let's walk through where that moment led to you. Tell me that day is how long ago? Five years that day
Speaker 1 15:28
now is, it would have been january 2016 so it's going on nine years. Nine
Scott Benner 15:34
years, okay, so nine years ago, by the way, I'd like to do another podcast on the conversation you had with your wife when you got home that night.
Speaker 1 15:43
Oh yes, I think she would love to wait on that. There was, there were some tight moments. There so dense moments, for sure,
Scott Benner 15:49
in our home. Yeah, you know what? You make a better point. I'll get her, because she'll start out so dummy took us from Vancouver over here.
Unknown Speaker 15:57
Yeah, totally Yeah. What did
Scott Benner 15:59
these last nine I know this is a big question, but, but what have these last nine years been, and where did where they led you? Like, where are you right now? Yeah, so
Speaker 1 16:08
we started out with just a really simple idea, or a really simple question, which is, you know, if you look in how type one diabetes develops, can we look a little earlier than when diagnosis happens, and if so, what is going on in the pancreas? What's going on at the level of beta cells? Are they really just kind of sitting there, sitting ducks to be picked off by this really, you know, sort of poorly understood auto immunity that we really don't understand yet. Or is there something going on? Is it a sort of a two way street and and maybe some things that they're doing could be part of this really complex equation that leads to type one, right? And so we started thinking about these earlier sort of stress responses. We like to, we like to think about beta cells as cells that are very prone to being stressed. And simply what we mean, what I think I, you know, mean by that would be just that, you know, there's a lot of ways that they can stop doing what they're supposed to do, and not just in the sense that they they get killed by the immune system or they die, but that they can sort of say, well, I'm not going to make insulin for a little while. I'm too tired. I'm too exhausted. I got to these other things to deal with. So they have these complex behaviors that we're kind of still trying to work out, I would say, in the field. But we started to really pioneer this idea that early responses in beta cells and how they interact with the immune system could shape the progression of the disease, and really could lead to whether the disease happens really quickly or whether it takes a long time. So we started out with fairly simple experiments in animal models where we were just looking at some of the things that could happen to these cells. And we were really surprised when we started to get data that suggested that beta cells are undergoing a process that is actually causing them to be like accomplices to the auto immunity. You know, here, we here, here, all along. The dogma is really that type one diabetes is really just driven by auto immunity. It's really the immune system to blame. The beta cells have nothing to do with the matter. So we really just need to focus our efforts on the immune system. And I think if I could summarize a lot of common knowledge and medical textbooks on type one diabetes and how it works. That's kind of really where we've gone as a field, and it's only it was only in the last, I would say, 10 years or so, that our work and that of a number of other labs in the field, has started to really think about these early stress responses in the beta cell and how these might be sort of galvanizing or accelerating the process. And you know, this cross talk between pancreas and the beta cells themselves and the T cells, these, these immune cells that actually target the beta cells in type one
Scott Benner 18:48
So are you saying that what you're looking at is that the T cells we thought attacked the beta cells, the beta cells gave up, and you have type one diabetes, but you're saying they're in the symbiotic relationship that's holding them this way.
Speaker 1 19:00
Yeah, yeah, that's the really exciting thing. And so we, we did some work in in some animal models to show this, that when you basically block or help the beta cells to overcome those stress pathways, you can actually slow down the process of the autoimmune destruction. So the autoimmunity is not some sort of foot on the accelerator that that cannot be shaped or slowed down. It's actually in this very complex dialog, as it were, between what the T cells are seeing and what the beta cells are doing. So we can, we can look at both sides of that equation now. And I think there's some really exciting clinical work, clinical research studies that have come out to really substantiate this further. So we've we've we focused our efforts on that, and from that discovery, we've been able to move forward with some new things that we're doing in the lab around looking at whether we can detect these markers of beta cell stress and. Earlier in the progress of type one Okay, and this is really exciting because, you know, now there's this idea around type one diabetes stages. I don't know if you're familiar with this idea, but it's, it's a fairly recent concept, but the idea that there's sort of pre clinical or stages that happen before someone gets diagnosed that we can actually measure to detect whether they're likely to progress to actually diagnosis. So you have the auto antibodies. So these are antibodies that the immune system produces against beta cells. And if someone has two or more of these auto antibodies, that's considered stage one of type one diabetes, right? And then if they have two or more auto antibodies, and then there's, you know, changes in their glucose tolerance, we would say that's stage two, and then stage three is when they get diagnosed. So if you think about it, there's now these two pre clinical stages that we can measure with a blood test that will look at auto antibodies, and we can do things like glucose tolerance testing in order to know where someone would be along that continuum before they get diagnosed, being able to look at stress in the beta cells and in the pancreas specifically, and then being able to link it back with some of these earlier stages of type one, I think, is going to be really transformative. And that's I think we're the work we're doing is headed and, yeah, it's a really exciting time to be in the field. Are you? I mean,
Scott Benner 21:18
obviously you're still in the process of figuring out what that communication between the cells is, but have you begun to wonder how to interrupt it?
Speaker 1 21:26
Yeah, yeah. So we have, we definitely have some clues from our animal studies where we've identified specific components in the cell that we think are good drug targets. Unfortunately, you know, obviously it would be wonderful if what we did in an animal model immediate. Model immediately was translatable to people. But as we know, I think the history of medicine will tell us that a lot of things that are studied in animal models just really can't tell us what we need to know about what happens in humans. So
Scott Benner 21:53
Pete, I've long been a proponent of instead of trying to figure out how to stop type one diabetes in humans, you should figure out how to take humans with type one diabetes and turn them into lab mice, because they think if you could do that, you could just cure them all very quickly.
Unknown Speaker 22:10
That would be wonderful, any number
Scott Benner 22:12
of 1000 different ways that we figured out how to do that. I understand your point. I want to let you finish your point, but then I have a follow up question. I'm sorry I cut you off with stupidity, but finish your point there, and then I'm going to follow something else. So
Speaker 1 22:23
we do have some ideas. I guess I was just, I was just going to follow up by saying that we have some we have some inclination, but we need to do use some of the tools that we have where we can study human cells in a sort of lab based setting. So we we have really great collaborators. We have an amazing team here in Manitoba that studies pediatric diabetes. Maybe I'll get into that a little bit later, but I also have lots of colleagues that work on type one diabetes from the human perspective, and so we do get deceased organ donor tissues and things like that that can help us to really make connections between what we're seeing in the animal model and what could be happening at the cellular level in the human pancreas. So those are really amazing tools, and I'm very indebted to, you know, the expertise of of my colleagues in that way, those who are doing the immunology side of it. Because I'm not an immunologist myself, but you know, we do want to understand the immunology. We know that there's a cross talk there. And I hope nothing that I've said would let anyone or lead anyone to believe that I'm not, you know that I'm saying that type one is not a non immune disorder. You know, of course it is. But I think we just need to broaden our understanding what that actually means. You know, we don't want to just think that it's only the immune system and that there's nothing that is going on with the beta cells
Scott Benner 23:35
themselves. Oh, no. I think it's important to I mean, as you were talking, what I was like, focused on, in my own mind, was that idea that somebody has an idea like, you know, like, oh, you know what it might be this, and then they spend a lifetime chasing that pathway. Well, maybe that will be it. Maybe they'll get to the end and be like, Oh, I fixed it. But we need other people going down other paths, yeah, and chasing other ideas. Like, a decade ago, there was somebody saying, like, I think it's possible. You know, we used to think of the beta cells as being dead, but I forget the name of the research. They're like, I don't think they're dead. She's like, I think they're frozen. That's how she described them as they were, like, swollen and couldn't move and do their job and or something like that. And I was like, when she said that, I thought, cool. Go figure out if that's what's happening. Absolutely. You go look at that right now. I have a new second question. I'll ask my first. I'll ask this one. First, how much do you count on other labs do you have? I've spoken with other researchers. Some of them share their like you guys had kind of a network of computers, I guess, and like in back room stuff, where you can see what other people are doing, but is AI going to help you move these things along more quickly? You're in Manitoba, and you're thinking about what you're thinking about, and somebody somewhere else thinking about something else. How do we push it all together and then ask a bigger mind? Do you see any through ways here, between all these different ideas?
Speaker 1 24:58
I think there's a lot of potential for. AI, and I know it's already being used in in some settings to try to bring things together. Like you said, we need to have more contact. I think. What has you know, in my limited time in the field, I've seen this. I know a number of other colleagues I've spoken with have seen this and have served this over the years, just that, you know, it's so easy to be very siloed in science, academic researchers are notorious for having pet ideas or concept. They don't want anyone to steal it. They don't want anyone to know about it, and they want to kind of work on it in their own isolated little bubble. You know, well, that's just not the way that sciences can be done and be effective in the 21st century. We really need to come out of our silos and share data, share information. And AI is definitely one of those ways that we can do that. I think a lot of effort is being placed on this from major consortia, and we see some of that happening, a lot of that happening in the US with what's called the human pancreas Analysis Program, or H path, as we like to call it. This is a huge data gathering consortium where they're basically saying, Well, hey, if we can study, you know, this aspect and this aspect and this and put it all together from, you know, hundreds of deceased organ donor pancreas and, and people who had type one and, and, you know, get blood samples and, and do all of this stuff and bring it together, we would have this amazing resource for the community. And then you, you do have, you know, a bit of a way of of collective, collectivizing people's thoughts, and so that you, you do get people being able to crowdsour things in the way, I guess you could say it's and then making that freely and publicly available, and an interface that that anybody can use, you know, they, they've done an amazing job with this, and not just them, there's, there's others who are doing this. So I think things like that are really changing the game. And they're they're bringing academics out of their silos, which I think we need to do more
Scott Benner 26:48
of. It just makes sense to me that if you started this nine years ago, just using you as an example, and this thing I heard, I heard 12 years ago, you haven't heard that now, maybe it's useless, right? But maybe it's not, and I don't know that the human mind can hold all these ideas at the same time and try to see the connections. I think you need a bigger thing to say, like, here's all the research we've done on type one diabetes and all the theories that people have had. You know, can you AI, hold them all at once and try to see if there's something from Chicago that, when I link it up with the thing from San Francisco and, you know, and Manitoba, to come up with some something that none of us have thought to think about yet. Like, it wouldn't surprise me if the researcher that figures something big out comes at it from that angle, instead of just picking their pet project and running after it. That's my thought, absolutely.
Speaker 1 27:42
Yeah, absolutely. I think that's where the fields headed. And, you know, I think we need to see, we need to have more investment put into that. And, you know, AI is a bit of a sensitive subject. I think maybe there's a lot of concern around, is it going to take away some of the things that, you know, we as humans can bring to the equation. But I don't think it has to be that way. I think there's responsible and effective ways to use it, and at the end of the day, it's a technology that, you know, technology can go either way, right? So
Scott Benner 28:08
listen, if AI puts you out of business, come to my house. I'll make you dinner for a week. Okay, sounds great. Scott, I love that. I love that. We'll get you going again. Don't worry, I find just something else to do. So my other thought was, gosh, that was not my first thing that oh, don't worry, Peter, I found my idea if I said to you that I received a text this morning from a person who's been on the podcast previously, the mother of a child with type one comes on the show last year. In this year, we've done a lot of GLP conversations this year, Dr Blevins out of Austin, talking about glps, lot of different things. Some people coming on. So this woman comes on. She's the mother of a child with type one at the time. I think the child's 15. She's got diabetes for, I think about four years at this point. Definitely has type one, you know, auto antibodies, markers, etc, using about 70 units of insulin a day at that time, Omnipod, CGM, both being used. The mom had PCOS symptoms earlier in life. Ended up on some we go, V, helped the mom with the PCOS, a little bit of weight loss, that kind of thing. The daughter starts to develop the PCOS pretty badly. Weight starts to come. So they follow suit, put the kid on. We go, V, and today, this morning, I got a text from her to tell me that her child is now down to just one unit of basal a day. It's injected. She took her pump off six months ago, stopped bolusing for meals, started just injecting basal insulin. Think it was five units at one point, then four, then three, two. Now today, just one. So now a kid, probably 16 at this point, had type one diabetes for four years, gets put on a GLP for something else, you know, they say for weight loss. But obviously her doctor was trying to help her with the PCOS, but it's not on the label. So, you know, you do it the way you do it. She goes on that and now today, she's down from 70 units of insulin a day to one unit of. Basal lens on a day not covering meals. Is that an example of the conversation between the T cells and the B cell and the beta cells being interrupted? Is that even a thing you've ever heard about before?
Speaker 1 30:12
I'll say, I've never, I've actually never heard about that before. I think that that's, I mean, that's phenomenal. That's nothing short of of, you know, wonderful. I mean, I have no clear explanation for that. I mean, I'll say I'm not an expert in the GLP one receptor agonist space, but I know there has been a lot of excitement about, you know, anecdotal evidence. Mainly, I've heard of people using people with type one using these agents to help control their sugars, and seeing really good results. And so, you know, in this case, you have, you know, there's, there's PCOS going on, and other things that that might have been computing, you know, but disrupting that communication between the T cells and the beta cells can take a lot of different forms. And I don't think this is maybe a really clear example of in the future what we might be able to think about that. We, we have all of these sort of tools in our tool belt. And in some cases, it's going to be something like a GLP one receptor agonist that's going to be really powerful and really effective for somebody. And in another case, it's going to be something else, you know. And so I don't think, I think this is an example of, you know, we, we often think about type one diabetes, oh, we got to find the cure. And I really, really rail against that language, and I think we all should, because I don't think there is going to be one cure. I think there are multiple ways. And, you know, it's about finding the way that is going to work for for that individual person, and really moving towards what we could think about is maybe, I don't know this, this term is thrown around a lot, and maybe it's lost its value. But personalized medicine, you know, just the idea that we can tailor things better and not just do a one size fits all sort
Scott Benner 31:48
of approach. It's awesome that you said that, because I didn't think you were going to be like, Yes, Scott, that makes perfect sense, and we've been looking into it. I brought it up so that I would put it on your radar. Because that's not the only conversation I've had like this. I've also had a man on. I'll send you these later. I had a man on in his 50s, diagnosed type one, and he's, you know, managing it with insulin for years. You know, he's having a rather slower onset, but he's, you know, more and more insulin. And one day, his doctor just says to him, Hey, how about we try to use this GLP to get some weight off of you. And so they go for it, you know. And the guy loses weight, and he's not using insulin right now, like now, he still has type one and, and I, my expectation is, is that he is probably in the bros of a very long, slow onset, maybe, like, a lot of situation, or something like that, but hell, if it keeps them from using insulin for a couple more years, then great. Like, I want people to understand, like, I'm not saying glps, like, cure type one diabetes, or that if you have type one, you take a GLP, you suddenly won't need insulin anymore, because there are plenty of people who are on a GLP and have type one, and their insulin needs don't change that much. But that's why I loved what you said about thinking individually, because for the people it works for awesome. You know what? I mean? Like, it's not going to work for everybody, but if this little girl is 16 years old, I mean, she's injecting a unit of basal a day, that's it. And who knows how long that'll last for. But you know what, if it lasts for five years? Like, how great is that? And what could doctors learn from that in the meantime? Like, if we look up, like, I'll tell you right now that my daughter uses a GLP with her type one, and it does pretty significantly bring down her insulin needs, maybe by 20% right now, yeah, she lost 15 pounds. Like, is it because she lost some weight? Is it because she changed how her her eating worked, like, you know what? Maybe, maybe she's just taking in fewer carbs, and her body mass is lower, and so she's using less insulin. That's fine, but here are the things it's also doing. My daughter also has PCOS symptoms. Her stomach pain significantly decreased on a GLP My daughter has had since her period started, and she's 20 now, she's had trouble with acne. Her acne almost completely gone on a GLP medication. Is acne? Is that inflammation? Right? Is, is the GLP lowering her inflammation like I think we need people to pay attention, is what I'm saying. That's all
Speaker 1 34:18
absolutely, I 100% agree, and I think it, it just points to that, yeah, that idea that we need to take note of these cases and these situations where we're seeing benefits. And also, I would add that, yeah, we don't always necessarily need to know every single detail of exactly how these things are doing, what they're doing. As long as we understand that they're safe, we understand what they should be used for and what they shouldn't be used for. I think there's a lot of space in that gray zone that, if you will, of you know, we Hey, you talk to someone who's an expert in this field, they'll say, Yeah, we understand X, Y and Z about what GLP, one receptor magnets are doing. But then there's this whole other alphabet of things that they could say that we really don't understand why it improves this and. And the next thing it just does, and maybe that's enough, right? Yeah, right. Oh,
Scott Benner 35:04
so Peter, this is off the topic, and then we'll get back to your thing. But the reason we knew to try the GLP for my daughter is because I tried it for weight. So I'm probably 57 or 58 pounds lighter today than I was almost two years ago. Wow, which is awesome, and it changed my life in a million different ways. But moreover, throughout my life, I was a person who, no matter how well I ate, I gained weight. I always used to, I would joke with people that, like, if I if I decided that today I was going to have a sandwich with bread, then tomorrow, I would retain water like a pregnant lady, like I'd wake up, like, I'd wake up like three pounds heavier, like you and I could eat the same thing, and I'd gain three pounds, and you'd be like, I don't understand what happened to you. I also, through my adult life, was having to get iron infusions because my body would not absorb iron like through my through my diet, and even if I took supplements, it just didn't work. But you know, I haven't had an iron infusion since I started using a GLP medication. And to that, I would say exactly what you just said. I don't know why, and I don't care why. Yeah, yeah, right. It just it helped me. So if someone can figure it out to explain it to somebody one day, that'd be awesome. But for me, personally, I don't care. I'm doing better now today. So anyway, I'm sorry, so tell me a little more about what your the research you're doing. So
Speaker 1 36:20
in our research, we are really trying to develop ways to better understand and then better target the stress responses that beta cells experience for type one diabetes develops. So we, you know, we use animal models, as I mentioned. We use deceased organ donor tissues as well, because some of these responses, you know, we don't, they're quite volatile, if you will. So, you know, we kind of, kind of study them in a dish. You know, the cells won't behave the same way that we think they're behaving when they're in the pancreas. So we can sort of trigger them or manipulate these pathways to sort of mimic those responses in a in a dish or in a test tube. And then we can, you know, kind of gain insights into, okay, if this is what it looks like in a dish or in a test tube, well, how does that correspond to what we see in the pancreas, and what could be happening at this particular stage of, you know, the development of diabetes and and so we're doing a lot of work in that sort of early stage space. Because I think kudos to the my colleagues who are working on stem cells and islet replacement therapies, I think there's amazing, groundbreaking work that's being done in that area, but I think they would be the first to also recognize that, you know, there's a lot of hurdles, there's a lot of challenges, and these types of therapies are not going to work for everybody. And more to the point, we need to move beyond just, you know, dealing with a disease once it happens, to understanding why it happened, and then hopefully eventually one day, being able to completely head it off at the past so that nobody ever develops it again. And I think that's where our research is really looking to the future, and saying, you know, we have these tools and approaches and medications, and maybe it's transplantation as well that can be done when people develop type one, that maybe even one day it could be safe for kids who developed type one. What could we do that? Would, you know, head things off at the pass and prevent the development of type one for, you know, people who will go on to develop it, and if we understand more about what's happening in those early stages, then there's things that we can do. So where I'm really excited about that part, I think that there's a lot of questions we don't have the answers to yet, but I think this is where as a what I would like to call a fundamental or basic research scientist. So, you know, there's this kind of divide between people who study things in a cell model or in a in a dish, versus people who are studying things in, you know, clinical setting with patients and things like that. Clinical basic science divide. Basic researchers need to do better at engaging with people who have diabetes and with clinicians. And I think for too long, I've seen in my own experience, there has been a big divide, if you're, you know, doing fundamental research, sometimes it's very difficult to build connections with clinicians. For a lot of clinicians, they don't have the time to spend to think about research. They're dealing with a patient case load. They have to get through that right. They don't have time to go beyond that. And then, on the other side, you have a lot of basic researchers who are just so focused on their cells in a dish that they don't want to look beyond that, to sit, to ask the question, you know, to even to have it as part of them. What is what I'm doing? Even important for people who have diabetes, do they even care? You know, that I'm doing this, is it going to make any difference to them? You know? And so I think that's where I've started to really take cues and learn from a lot of my, my the partners that I've been able to develop, partnerships we've developed here in Manitoba, you know, we've got a family advisory group that's really helped to shape some of the research direction and giving us feedback and ideas. And we, you know, we go to them a lot, and we exchange knowledge, you know, the idea that somehow, as a basic researcher, because I have a degree and I've done this research that I know more than. Someone who doesn't about diabetes is, I don't think is accurate, and I think we need to get away from, you know, recognizing that one person's knowledge or thinking that one person's knowledge is better than another. It's not. It's just different knowledge. I had a really dear friend, and she's a patient partner on one of the team grants that I work on, who had to really drill this into us. And, you know, everybody's at a different stage with this. There's some basic researchers that have been in the field for so long, and this is so new to them, but she had to really drill it into us and say that, you know, like, I and she's lived with type one diabetes for over 50 years. She has a daughter with type one, and she's like, Look, I am an expert in what it means to have type one and then manage it and and manage it for my daughter, like I've gone through this, I have this experience that's so valuable. We need to be recognized as experts in our own right in this area. And I was just like, that's exactly what we need to recognize and hear. I've been really learning from that and trying to change my perspective and recognize that, you know, different types of knowledge can be brought together. And when we do that, we are we're all better off for it. Yeah, that's kind of where I think we've been going as well, is that we don't want to just to be developing these questions in an isolated bubble, this idea that we don't want to be just thinking about things without any sort of communication or interaction and being able to share that knowledge. So seeing it as a two way street, what do you
Scott Benner 41:20
think the best way is to because you're it's interesting, because we don't know each other. But I'm on this idea as well. So I started off by saying that I've had, you know, 1000s, you know, by the time this podcast is over, to have 1000s of episodes of people coming on here and saying, you know, telling their stories, or, you know, anecdotally, explaining how they handled something. And I one day said to myself, I used to tell people, Peter, just go listen to the podcast. You'll know how to take care of your diabetes, right? Like, that's when I started, like, I was two, 300 episodes into it, and I was like, I don't know how to explain it to you, but if you start at the beginning and listen your A, 1c, will just come down to the sixes, which, by the way, worked for people, which made me think that therein lies the answer. I don't have a wide enough lens to tell you exactly where the answers are. I just know they're in there. So eventually I figured out that I had a plan for diabetes. I just I never had called it anything. So I put together this Pro Tip series. Right now, I think it's maybe 25 episodes, I'll tell you now, if you don't want to listen to the whole podcast, listen to the Pro Tip series. Pro Tip series, I think you're able to come down into the sixes. Then I started expanding and thinking like, I bet you the answers to most people's diabetes questions lie in these episodes, but how do you say to them, Go listen to 1300 hours of this, and I guarantee you know you'll be okay. So I started as AI got better and better. I started thinking, like, can I just feed the podcast into AI and let it pull out the nuggets? Yeah, I think in that same vein, which, by the way, is the thing I'm working on behind the scenes, and because it's my goal that when I'm done making this podcast, that I leave it behind as a searchable repository. Like, that's my goal, right? So, fantastic, yeah, but as I'm listening to you and thinking big picture about the world, it occurs to me, like, I don't want to say something like, you know, crazy, like, the answer is already out there. We just don't know what it is. But isn't it like, isn't it possible that all the research being done everywhere, if you could smoosh it all together and find, again, something smart enough to go through it and say, here are the connections that you're missing because you're busy, you're tired, or also someone's father, or, you know, mother, or, you know, like just a human being, you're never going to see this or never hear that story like that. Just to me, makes sense that if you want to get to it more quickly, there has to be a repository somewhere and a brain that's in charge of going through that repository and looking for connections that we're missing.
Speaker 1 43:44
Yeah, I love that idea really. I think that that's going to be really impactful. And I would love to see something like that put together for, you know, your with your with your podcasts, you're doing that, but also, you know, in the in the research space, something that really would bring everything together. I think there's just so much out there. And I mean, I'm always, I'm always baffled when I I try to keep up with reading the current literature in the in even just in my sort of sub, little, tiny sub field of of type one research, and I, and I still can't keep on top of it, because there's just so much of cool stuff coming out all the time. And how would so, yeah, the idea of being able to bring it all
Scott Benner 44:22
together is really remarkable. Pete, if I asked you about a movie that was coming out, you might say I didn't hear about that one. There's no way for you to know about everything that's happening. And if you're doing the important work of drilling down on something focused and small, you can't see big picture little picture. At the same time, we don't have the capacity for that. It makes me wonder how many things in the world have gone right, and if you could go back and watch them happen, that you wouldn't learn that it was just by dumb luck or happenstance that it actually worked out.
Speaker 1 44:52
You know what I mean? Absolutely, yeah, yeah. I think it's a lot like stuff like that.
Scott Benner 44:56
Well, probably everything like that's probably what life is. So I don't want to wait. For happenstance to happen. It probably will, like, probably some guy's gonna wake I mean, you know, somebody's gonna wake up 50 years from now and go, Oh, huh, no kidding, I got it. This is how you cure type one diabetes. It just so happened that all these things happen. Like, can't we force that to happen more quickly? Is my point, and I think it's here now. I think we can actually so, yeah, I need one of you to start thinking about that. That's all. I don't know which one. I don't care which one of you. Your mentor, he seemed willing to pivot on a dime. Yeah,
Speaker 1 45:33
no, exactly, and ironically, I'll maybe I'll add that he actually pivoted pretty much out of the field himself. He's working on something completely different. He's just, you know, he's one of those people. I think he just saw something, he went with it, and it created something new. And then he was content to kind of say, okay, you can, I mentored you. I figured you're gonna go and take this into the next thing. And so then he's moved on to something else now. So I think that there's something, there's something really wonderful about that. And the way that science can advance is and train the next generation of researchers. You know, I train graduate students and a postdoc in my lab as well. And that's the idea, right? Is that there's no way that I can follow up on every single thing that we do. So I'm hoping that of the people that I train, there's gonna be someone who's like, hey, yeah, this is gonna be cool. I'm gonna take it in this direction and think of things that I never thought of, and that's what I've been able to do in my lab from the training that I
Scott Benner 46:26
received. So when you work with clinicians like when you do have connections with them, what are your takeaways from them that have helped you with your with your work? I think
Speaker 1 46:35
one of the biggest takeaways is, you know, it's trying, it's, I guess it's getting more specific with the questions that we asked. Instead of saying, Well, does, you know, X happen in type one diabetes, we can say, Well, does x happen in children with type one diabetes at this stage, you know, and really drilling down on some of the things that we don't think about, because we don't, we don't really, we don't work with people in our in our research, we're working with cells in a dish, or we're working with, you know, sections from a pancreas, or we're working with animals, you know. So it just, it opens your eyes to things that you just so quickly overlook, and you'd be surprised at how easy it is to make generalizations about the work that you do that that turn out to be inaccurate. You know, I think that part of our human brain wiring is really just to try to find shortcuts, right? We're always trying to simplify the complex information that's being inundated to us every day, and that, you know, you do that by making assumptions. Well, this is this was this way today, and it's been that way yesterday, so it's probably going to be that way tomorrow. And we do that in so many different areas of life, and so it does come over into the side of research, where we we just made generalizations about what we're doing, and we're not careful to sort of nuance those. And you'd be you'd be surprised at how many research papers you read that you when you read some of the things that are done and the conclusions that are made, you have to be very careful that we're not over generalizing or making the conclusion so sweepingly broad that we're missing the ways that it actually might be relevant very specifically, but not relevant in other ways. And so I always try to tell my students, you know, it's not just important that you show that you know whatever the process happens in this particular context. It's also important to show when it doesn't and when you know if you have a negative result that is very important and very valuable too. There's a
Scott Benner 48:23
parable about a pot roast, and you'll maybe stop me, but little girl and her mom are making a pot roast. Mom takes out the pan. She takes out the pot roast, she cuts both the ends off the roast, puts it in the pan, puts in the oven. It strikes the little girl as odd. She says, Mom, why did you cut the ends off the pot roast? The mother says, That's how my mom made it. So the little girl queries the grandmother, and you know, she says, Grandma, you know, my mom did this with the pot roast. Why? And the the grandmother says, well, that's how my mom made it. So they go to the old folks home, and they find the great grandmother, and they tell her this story. And, you know, take grandma, you know, Why'd you cut the ends off the pot roast? And she thinks and thinks and thinks, and she says I had a really short pan. I just think that's we end up doing a lot of things and we don't know why we're doing them.
Speaker 1 49:08
Absolutely. Yeah, I would totally agree with that. Yeah.
Scott Benner 49:11
So if that's the case, then you're making big decisions about things you're putting your life's work into. It made me think of what you said, like, you generalize and to like fill in the gap. You know you're like, Well, this must mean that, because that makes sense to me, but that doesn't exactly right. Doesn't mean it's true. Yeah, how many generations of people will do research the way you're doing it now? Do you think it'll shift at some point? You
Speaker 1 49:38
mean shift towards more, towards the team science, or is it
Scott Benner 49:42
going to be Star Trek when you're going to start telling the computer I'm trying to figure this out today. Help me figure this out. You understand the world's information. I
Speaker 1 49:51
think it could probably be, you know, if I'm, if I'm, you know, fortunate or lucky enough to have a long standing career, maybe, you know, 30 or whatever. Your career, I would say, you know, at some point along this road, that that's things are going to start to shift in that direction, yeah, the students that I'm training today, when, you know, some of them do choose to, you know, do a career in diabetes research, I think that they're going to be the ones that maybe those types of tools are just commonplace. And it's like, yeah, this is just what you do. And then we save our very precious human brain power for the things that that we can do best, rather than trying to assimilate all this information that we can never do, right? But, yeah, it's a good it's a relevant question, because I think it also has to do with, you know, how are we training the next generation? Are we are we training them how to think in a certain way? Or are we also complimenting that with you know, here are the Here are the tools that are going to be essential for us to do our job better, right? And some of these things are things that we're just learning how to use. We don't really know the best way to implement them. We're starting to see how they could be beneficial. But in the future, you're going to probably be relying on these things, because there's just going to be so there is already, and there will be, continue to be so much information that you can have a process,
Scott Benner 51:03
right? I think that the day to day life of people, in short order, 100 years is going to look so different than it is right now. Person from today won't, wouldn't recognize what a what a day in the life looks like. Anymore. It's possible we get back to everybody, you know, growing tomatoes and hanging out and chatting and, you know, like, because, like, maybe the, maybe the Terminator doesn't kill us all, Peter, maybe it, maybe it actually helps us. Like, right? So, yeah,
Unknown Speaker 51:30
wouldn't that be wonderful?
Scott Benner 51:35
Seriously, like, you're not going to stop this process now. Like, it's, it's in motion, and this is the way it's gonna go. I'm hopeful that with the limited, you know, I don't, I don't reach that many people, but with the people I reach, I would like it if you guys would all think about, like, how can I use these tools to make the thing I'm doing better, more accurate, more valuable? You know, not so much about like, limiting your own effort. I've said to people before, like, one of my favorite pastimes is to think to the end of my knowledge and wonder what's on the opposite side of that. Like, because I when I get to what I don't understand, I know there's more I just don't understand it. I hope people can use technology to wonder beyond that, because I think you're all asking yourselves a lot of important questions that you just don't know the answers to. But what if we can come up with bridges to those answers, and what will that do for people? Because, like you said, it very well may turn out that if I hold 10 people in front of me with type one diabetes, that they all aren't going to get to a world where they don't need man made insulin the same way. You know, there might be different, different pathways for those people. It's awesome. You're thinking about it that way. Yeah, that's definitely,
Speaker 1 52:47
I think, a key takeaway for me from our conversation today. I'm going to really look into that more and think a lot about that more, because whenever I can have conversations like this and then come away with it, with something that I didn't think about, or something a way that I could apply knowledge in different way. I'm really grateful for that. So, yeah, yeah, thanks
Scott Benner 53:04
for that. No, please i Listen, but hopefully it helps you. But I sit here, I think about your job, and I think, what if someone trained a large language model with just the research papers from the last, I don't know, 15 years about type one diabetes and people who were trying to cure it. What if there was an AI system that could only think about what was in that information, and that you could sit down at a terminal and ask it questions? That'd be awesome, trust me. All right, we just need somebody to get on that. I just need a few, maybe a million dollars and a lab and a couple of couple of guys who understand Python or something, I don't know. I don't know a lot about, I don't know a lot about the computer side of it, but it just makes sense to me, like that, if there's a pathway that this is it, because to go back to how you started this, we've been on this for 100 years, and all we got is it's synthetic now, not from beef and pork, and it works a little faster. That's how far we've gotten in 100 years. Now, that's awesome. Don't take me wrong. I think it's awesome. But if that's the pace we're on, then are we another 100 years to it? What? Like? What you know, what I mean? Like,
Unknown Speaker 54:15
yeah,
Scott Benner 54:18
you need to connect the through lines like and Pete could work his whole life, and five years later, someone could start over, and no one would know a damn thing about what you spent your life on. And that's not how we're going to build on ourselves. I think, yeah, geez, this is a turn into a bummer at the end. Pete, I didn't mean for
Unknown Speaker 54:37
Well, we had fun along the way, I think, didn't we? Is
Scott Benner 54:39
there anything that I didn't ask you about that you about that you wanted to talk about?
Speaker 1 54:43
No, I think that that kind of covers it, I mean, but yeah, I'm always excited to share about what we're doing, and hopefully this is you know, for your listeners, they're interested, or they want, they have further questions, they have. Any of them can feel free to contact me, my contact information. I can. I can give that, or they can just google me. PM, we have a lab website. You know, one other little point there is just like, how important it is now, in again, the 21st century, you'd be surprised how many researchers don't have any sort of online presence, and it's very difficult to actually figure out what they do. So when I started my research lab, I was like, That is like, so fundamental. I need to make sure I have that in place so that everyone can kind of see what we do, what our research is about, and if they have any questions, we can get in contact and we can have a conversation. Because to me, that's that's really where the rubber meets the road. That's why this work is going to be meaningful and important and impactful. Happy to feel any questions or have any further discussion with anyone who might be interested in
Scott Benner 55:38
listening today. It's awesome. Well, I'll tell you, you can easily if you Google Peter Thompson, P, H O M, P, S O n and diabetes, it will take you to a University of Manitoba link that you'll be able to find them very easily that way. But also, Pete, if you send me a link, I can put it in the show notes to the podcast so that people can click on it. Sounds great. Scott, that's perfect. I want to finish by saying this like I understand why people, so many people suggested you for the podcast because you have a really good energy. Can I ask how old you are?
Speaker 1 56:07
Yeah, I'm 40 years old. As of August 18, I turned 40. I did the big got the big four. Oh, so I made Yeah, well,
Scott Benner 56:12
congratulations, but I only asked because I assumed you were about that age and you feel like you're 23 Wow. Seriously, oh my gosh. I mean, no, seriously, like, oh, 1,000,000% like, you have the energy of somebody who just got out of school and was like, I'm gonna do this. And I guess that's my last question. Is, like, where does that come from? Do you know, or do you think it's just natural?
Speaker 1 56:31
I don't know. I think it's, it's part of just how I approach life. I guess I really, I really try to bring a positive attitude to everything I do. I mean, it's very easy to get discouraged and but, you know, I think there's all these little silver linings all along the way, and I didn't get to, get to say anything about it, but, you know, I did start my lab during the COVID pandemic, and that maybe that's a whole topic for another, another episode of, how do you, how do you do research in a pandemic situation? And many people could weigh in on that, but you know, I've had these things that I've had to deal with, and, you know, some of that is just my own personality. I'm a person of faith, so my faith factors into that too. And I think you just have to find things that keep you going. And some people, it's friends and family. Some people it's, you know, their belief system, whatever it is, you have to find something that's worth fighting for and why you you're, you know, find your why. And so for me, that's, those are some of the things that help me. And the research I do is so exciting. I just, I'm still I still pinch myself every day. I love the job I have. I love the work I get to do. I love the people I get to interact with, and really feel like we can make a difference. So for me, that's, that's all I need.
Scott Benner 57:37
Well, that it genuinely comes across when when I'm speaking with you. So I appreciate you taking the hour and doing this with me. Thank you very much. Fantastic.
Speaker 1 57:45
Thanks so much for the invitation. Scott and really was happy to be on the the episode today.
Scott Benner 57:55
I'd like to thank the ever since 365 for sponsoring this episode of The Juicebox Podcast, and remind you that if you want the only sensor that gets inserted once a year and not every 14 days, you want the ever since CGM, ever since cgm.com/juice, box, one year, one CGM, earlier you heard me talking about blue circle health, The free virtual type one diabetes care, education and support program for adults. And I know it sounds too good to be true, but I swear it's real. Thanks to funding from a big T 1d philanthropy group, blue circle health doesn't bill your insurance or charge you a cent. In other words, it's free. They can help you with things like carb counting, insurance navigation, diabetes technology, insulin adjustments, peer support, Prescription Assistance and much more. So, if you're tired of waiting nine months to get in with your endo or your educator, you can get an appointment with their team within one to two weeks. This program is showing what T 1d care can and should look like. Blue circle health is currently available in Florida, Maine Vermont, Ohio, Delaware, Alabama and Missouri. If you live in one of those states, go to blue circle health.org to sign up today. The link is in the show notes, and please help me to spread the word blue circle health had to buy an ad because people don't believe that it's free, but it is. They're trying to give you free care if you live in Florida, Maine, Vermont, Ohio, Delaware, Alabama and Missouri, it's ready to go right now. And like I said, they're adding states so quickly in 2025 that you want to follow them on social media at Blue circle health, and you can also keep checking blue circle health.org to see when your free care is available to you. Okay, well, here we are at the end of the episode, you're still with me. Thank you. I really do appreciate that. What else could you do for me? Uh, why don't you tell a friend about the show or leave a five star review? Maybe you could make sure you're following or subscribed in your podcast app, go to YouTube and follow me or Instagram. Tik, Tok. Oh gosh. Here. One. Make sure you're following the podcast in the private Facebook group as well as the public Facebook page you don't want to miss. Please do not know about the private group. You have to join the private group as of this recording, it has 51,000 members in it. They're active, talking about diabetes, whatever you need to know. There's a conversation happening in there right now, and I'm there all the time. Tag me. I'll say hi if you or a loved one was just diagnosed with type one diabetes and you're looking for some fresh perspective. The bold beginning series from the Juicebox Podcast is a terrific place to start. That series is with myself and Jenny Smith. Jenny is a CD CES, a registered dietitian and a type one for over 35 years, and in the bowl beginnings series, Jenny and I are going to answer the questions that most people have after a type one diabetes diagnosis. The series begins at episode 698, in your podcast player, or you can go to Juicebox podcast.com and click on bold beginnings in the menu, the episode you just heard was professionally edited by wrong way recording, wrong way recording.com, you.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#1430 Blue Adjacent
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
A firsthand account of overcoming diabetes mismanagement, kidney transplant, and the power of community support.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Hello friends, and welcome back to another episode of The Juicebox Podcast.
Christie 0:14
Hey, Scott. I'm Christy, and I've been type one for 31 years before all the wonderful technology we have here. My grandmother had type two but ended up using insulin and was on dialysis for many, many years before she passed.
Scott Benner 0:30
Nothing you hear on the Juicebox Podcast should be considered advice medical or otherwise, always consult a physician before making any changes to your health care plan. I know this is gonna sound crazy, but blue circle health is a non profit that's offering a totally free virtual type one diabetes clinical care, education and support program for adults 18 and up. You heard me right, free. No strings attached, just free. Currently, if you live in Florida, Maine, Vermont, Ohio, Delaware, Alabama or Missouri, you're eligible for blue circle health right now, but they are adding states quickly in 2025 so make sure to follow them at Blue circle health on social media and make yourself familiar with blue circle health.org. Blue circle health is free. It is without cost. There are no strings attached. I am not hiding anything from you. Blue circle, health.org, you know why they had to buy an ad. No one believes it's free. This episode of the juice box podcast is sponsored by the Dexcom g7 the same CGM that my daughter wears. Check it out now at dexcom.com/juice, box. You Juicebox, friends touched by type one's walk is coming up quickly on March 8 at the Saturday at Lake Eola Park in Orlando, Florida. Go now to touched by type one to sign up and register. It's completely free. You're gonna have a wonderful time. Touched by type one.org. Go to the Programs tab, click on Steps to a cure. Hey,
Christie 2:03
Scott, I'm Christy, and I've been type one for 31 years before all the wonderful technology we have
Scott Benner 2:09
here, 31 years. How old are you now? I am. I'll be 36 in October. Wow. You were five. Okay, almost five. Oh, not quite five. A birthday? Not quite five. Yes. How nice? Any other type ones in your family?
Christie 2:26
Nope, my father's mother. So my grandmother had type two, but ended up using insulin and was on dialysis for many, many years before she passed type
Scott Benner 2:36
two. So much so that she was on dialysis. Got you? Do you have insulin resistance? Do you think, like, do you when you look at your needs, you're like, wow, these seem aggressive. Or no,
Christie 2:47
some days it's more what I'm doing throughout the day than what I'm eating and how much insulin I'm taking for it. The other day, you know, I was at 300 and dropped to 54 while working just because of how much movement I was doing. Wow, you know, so it, it just depends. But I have had a kidney transplant myself, so it, you know, my teen years weren't the best. Oh,
Scott Benner 3:12
hold on. We're going to get listen to you laying it out for me. Thank you. We'll do that in a little bit. How about other autoimmune issues in your family, hypothyroidism, celiac, it allowed. There
Christie 3:25
are three of us in my immediate family that have hypothyroidism. You ever
Scott Benner 3:31
get tested for the antibodies to see if it's Hashimotos? No, I have not been tested. Okay?
Christie 3:38
So it's controlled with medication very well. My endocrinologist seems to just be happy with the medication as of now. Do you know what that means
Scott Benner 3:46
when they tell you they're happy and it's controlled well? Do you know what your TSH is? For example,
Christie 3:51
my last one was horrible because I had actually added a new medication to my regimen of things that I take with all of my anti or sorry, immunosuppressants. Immunosuppressants,
Scott Benner 4:05
yes, what are you taking those for? But I was
Christie 4:09
immunosuppressants are for the renal transplant. Gotcha, okay. But I had added we govi to my regimen to try and help me lose weight so I could get a pancreas later on.
Scott Benner 4:21
May I say, Can I guess? May I get? Let me guess. Christy, let me guess. Come on, let's, let's have some fun with your health issues. Of course, it slowed down your digestion and threw off your medication. I'm
Christie 4:30
not quite sure if it was a mixture of things. I ended up having what I was on it for two months, and then I went to get month free, and I just had awful symptoms, so they told me to hold off. But my TSH was way off, my immunosuppressant levels were off, and my kidney function had dropped dramatically, and then I had ketones with perfectly good blood sugars because I just wasn't having the insulin needs because I was hardly eating. How
Scott Benner 4:59
does it. Doctor not say, Hey, you're a person taking a number of medications orally. They're very important to you. This medication is going to completely change your absorption, your digestion. Maybe we should pay attention to that. That's fascinating. I know that doctors are still getting used to glps and everything, but, you know, I've told a story recently on the podcast. I don't know how recently, because I don't know when these come out exactly, but person with, like, fairly aggressive medications for, you know, depression and mood disorder stuff, and they're losing weight on a GLP, which is great, but their mood stuff is going haywire, and immediately their doctor said, oh, yeah, this is probably through, you know, because absorption, and it certainly was the medication that you're taking, especially orally like that, right? It gets changed. The absorption gets changed. That's interesting. So people using glps and thyroid medications should take a look, because you might end up needing a larger dose or who knows what, but it was really working for you, huh? You were barely eating. Yeah. Did you lose weight?
Christie 6:07
I lost 15 pounds in the two months that
Scott Benner 6:10
I was on it. That's excellent. But then you had to come off it, right? Yes, I
Christie 6:14
am indefinitely off any sort of medication like that. I'm not going to take the risk of losing my kidney to lose weight.
Scott Benner 6:21
Oh, sure, no, that's an obvious trade off you don't want to make. But the
Christie 6:25
funny thing is, is I had four different teams sign off on me taking it. Yeah?
Scott Benner 6:30
Well, because people can't think that was my original point. Chrissy, you get people here you think are helping you. Just
Christie 6:36
yeah, my primary care, and then my primary care is Ma, three,
Scott Benner 6:41
yeah. Okay, well, did you figure it out, or did they eventually you can manage diabetes confidently with the powerfully simple Dexcom g7 dexcom.com/juice box. The Dexcom g7 is the CGM that my daughter is wearing. The g7 is a simple CGM system that delivers real time glucose numbers to your smartphone or smart watch. The g7 is made for all types of diabetes, type one and type two, but also people experiencing gestational diabetes. The Dexcom g7 can help you spend more time in range, which is proven to lower a 1c The more time you spend in range, the better and healthier you feel. And with the Dexcom clarity app, you can track your glucose trends, and the app will also provide you with a projected a 1c in as little as two weeks. If you're looking for clarity around your diabetes, you're looking for Dexcom, dexcom.com/juicebox, when you use my link, you're supporting the podcast, dexcom.com/juice, box. Head over there. Now you
I did because I had awful
Christie 8:08
symptoms, and so after two weeks and the symptoms didn't subside, I ended up having lab work done, and found that all of my numbers were off, so I immediately panicked and called my team, and I'm like, what's going on? So my endo was just like, you have ketones. Your sugars are fine. You're not eating enough, so let's take you off it and see what happens. And then I got my kidney function test back, and I was like, Nope, I'm not going back on it. I'd much rather live with a healthy kidney than losing a few pounds.
Scott Benner 8:45
I don't want to blur lines here between me knowing something and me being an idiot on the internet, the ketones could have just been like starvation. Ketones not necessarily to do with diabetes. So right, right. You might have wanted to keep those ketones because they were probably an indicator that you were burning fat, losing weight, but if your medication is not absorbing correctly. Now, the thing that I get confused about, and of course, not with your, I mean, your for your kidney stuff, it's such a different thing, I'd want somebody to study it and have an answer. But there's got to be an amount of that medication you could take that would offset the absorption issue. But who knows what that is, and you don't want to be the testimony for that, for certain. No,
Christie 9:24
no, definitely not. Yeah, especially since my sister ended up donating in the paired program for me to receive my kidney,
Scott Benner 9:31
you don't want to let her know that you, uh, you trashed it, yeah,
Christie 9:35
sorry. And there's no extra spare parts just lying around. Yeah,
Scott Benner 9:38
you don't have one in the closet. Not that I want to go down this road, but to complete the thought. I mean, I think everyone who's listening knows that Arden's taking GLP for PCOS, symptoms, insulin resistance, stuff like that, that it's helping her significantly. But she lost an amount of weight that we looked at her when she got home from college after her sophomore year, we were like, Oh, you lost two. Much weight, and, you know, got together with her doctor very quickly. By the way, no messing around, like, put her doctor right on a phone call on video, stood her up like, here she is. Didn't even wait to get into an office, and said, Here's her weight. What do you think? We think she's too low. Doctor agreed. Said, love to see seven more pounds on her maybe. And so we just discontinued the GLP so that she could eat more readily. Gain the weight, and it would give us time to figure out what to do, because the GLP was helping her so significantly. But of course, we can't have it to the point where she's not eating well. So Right? Took a couple of weeks. She gained the weight back. That wasn't much trouble when she, you know, when all of her appetite came back, and then we just started dosing ourselves like Christy. This is probably where I have to remind you that the beginning of every episode there's a disclaimer that said nothing on the podcast is, you know, medical advice. This is something we decided to do on our own, along with our with her doctor. We're buying vials, like clean, you know, new vials, injecting the manjarno pen into the vial and then drawing out an amount of medication with an insulin needle and delivering it that way, but not as much as the pen holds, right? So we're right. We're changing. Yeah, yeah. Well, she's not doing it every day, like I do. Know people who are doing that, by the way, who are taking little bits daily, or every other day, or whatever, but Arden's not a huge fan of the needles, so once a week, but significantly less. It's only been two weeks now, in the first week, she had tonsillitis, really badly. Like, she What's that? When it gets infected, it's called strep throat, right? Yes. So she had that, so I couldn't figure that week. I was like, I don't know what's going on. Just more insulin, and she's feeling better this week. So we're, we're, I'm starting to already see the impacts of the glps on meal spikes and everything. It's kind of crazy, but my point is, is that I think that over time, we're going to see doctors understanding better that, yeah, the pen comes in two and a half. It comes in five. But that doesn't mean that that's what you need, especially if you're not taking it for weight loss. I wish you luck. I hope somebody figures something out with it, because 15 pounds in two months. I'm assuming you were pretty happy, right?
Christie 12:21
Oh, yeah, definitely, because it was, let's see, I had two, two different doctors appointments for transplant stuff, and then they finally said they're like, well, we see an incline, and we wait. We want to put you on hold for pancreas. Need you to lose like, 50 pounds, and then we'll talk about it again. I only lost 15, but I did start this new job, which is my first physical job since having my transplant. Okay, so I'm hoping that the activity, you know, doing it the old fashioned way, Scott activity, and watching your your diet, okay, so I can get back on active on the list would be great. Yeah, yeah. It would be. It would be amazing, of course.
Scott Benner 13:06
I mean, you're already taking the the immunosuppressant drugs, right? So why not grab a pancreas? Is that the idea? Yep, yeah. Okay, so let's go backwards a little bit. You're four, almost five years old. You're diagnosed. This is definitely like regular and mph time, yes, if
Christie 13:23
I remember, right? Yes, that was, it was in 1993 Okay, so, and then a few short years later is when I think they changed me to like Novolog. Which one's the orange one? I never remember. They're the same thing to me. Is it humologue? So I have human log and Novolog, and I can use them interchangeably, which is nice, because I do know some people that are like, Nope, they're not the same. My body doesn't absorb it the same. I have to take more of one over the other, yeah. But of course, insurance dictates which one we're allowed to have, so
Scott Benner 13:57
takes the one they give you situation, yeah. Okay, so you start off very young, probably for a little while doing it really old fashioned. Eventually you get faster acting insulin. But what did you mean when you said things didn't go well when you were younger and it led to your kidney issue? Like, what was your life like? What did you understand about diabetes and what was your daily management like? So
Christie 14:17
when I was four from my diagnosis, the only thing I remember is the blood draw and my dad wanting to knock the guy out because he stuck me like six different times. But after that, you know, my parents had reached out to my friends parents and said, Hey, daughters, diabetic now, but she would still like to do normal kid things. Do you have interest in learning about it. So my parents actually taught a few of my really good friends, parents all about how to help, how to dose, I can inject myself. So that was one of the things that I was really drilled into my head, was Do it yourself when you're this young, that way you don't struggle with it later. Or not. But
Scott Benner 15:00
did you actually struggle with it? No, no, no. Okay, so
Christie 15:04
I, you know, we had one of those. It looked because I was using injections. Obviously, I had one of those little injectors that looked like an airplane that you could put it in, the needle into, and then you do the button on the side, just like you would place an infusion set nowadays.
Scott Benner 15:19
Oh, interesting. I have never, nobody's ever brought that up. Do you know what it was called? I
Christie 15:23
couldn't tell you. I don't even have it anymore. If I had it, I would gladly send photos for
Scott Benner 15:28
you to post. Oh, that'd be crazy. Yeah, no, I've never heard of that. Actually, it was wonderful. So you could do your injections, but is it possible you weren't using the right amount of insulin?
Christie 15:39
Well, when I was first diagnosed that was all on my parents, like they would tell me what to do. In my teen years, I had a rebellious stage where I said I'm over it. I want to be normal, and I just quit pretty much taking care of myself. And the Medtronic pump that I was on at that time was pretty much the only insulin I was getting was throughout the day, but not meal Bolus or anything. You
Scott Benner 16:03
were just getting your basal through the pump. Yep. How long do you think you went on like that? Did your parents know it was happening? My
Christie 16:11
parents knew some of the neglect that I had for taking care of it myself, obviously, being a rebellious teen, they can't really force me to do it without holding me down. But that was never a road we went down. They said it's your choice. But at the same time, they would always ask me, have you taken your insulin? Are you checking your sugar? And that was another thing I wasn't doing because I did not have a CGM back then. You weren't using a meter. Maybe once or twice a month, I would check myself just dosed up of how I felt. It was awful, right?
Scott Benner 16:44
You're keeping up with the pump and it's running your basal profile, but you're not bolusing at all from food sometimes, but very rarely. Yeah, can you, in hindsight, tell me why sometimes you wouldn't, sometimes you wouldn't. Or do you not know
Christie 17:02
the way I felt? If I knew that I was getting too high and my stomach started to get sick with the ketones and all of that, I would finally take an injection. But it would take getting to that point before I would do you
Scott Benner 17:15
remember ever having conscious, like internal dialog about this, like, if I just did this sooner I wouldn't feel sick or I'm trying to understand, like because you're doing something, why not do something that stops you from feeling bad, instead of something that stops you from dying? Because that's kind of what you were doing, right? I
Christie 17:35
actually had an experience at the hospital where they my sugar was too high, they freaked out. And they were like, well, you're not taking care of yourself. You're pretty much committing slow suicide. We actually want to put you in intensive therapy program. I'm like, I'll do outpatient, but I'm not staying here. So it was about eight years that I was doing this, that I was hardly taking care of it myself. But finally, you know, I grew up and, you know, turned 21 and I could drink. And I figured at that point I'm like, Well, I'm not going to be stupid and drink and drive, so I might want to take care of myself the same time so I don't make stupid choices. You know, your sugar gets too high. You get the cloudy, foggy brain. And you know, you just, I have mood swings when I'm high. So I was always angry, yeah, so I finally started taking care of myself. And then, you know, my a 1c was back in an almost normal range. I was at an eight when I was getting there, but it took me getting pregnant with my 11 year old son now for me to actually, like, step up and do everything I needed to
Scott Benner 18:46
fascinating, Christy, I'm never gonna stop being fascinated by the same story coming out of like humans mouths over and over again. I didn't take care of myself. I couldn't find the, I don't know, the motivation to care whatever it was, right, like I was angry, and then all of a sudden, it's I either want to have a baby. I'm having a baby. I met a person. I want to be healthy for this, it's always for someone else that people seem to be able to pull it together. You ever talk to a therapist about why I'm so sorry, it's gonna come out weird, but why you didn't care enough about yourself to do it? No,
Christie 19:20
at that point I was I'd been on antidepressants since I was like 13, and now we're talking about drinking age. And you know, when I was pregnant with my son, I was 24
Scott Benner 19:35
would you say that you were depressed? Or would you say that your blood sugars were so high, that's how you felt like could you have gotten lower stable blood sugars and that wouldn't have been how you felt? Or do you not think that definitely depression? Okay, does that run through your family?
Christie 19:50
I know of one person in my family, immediate family, that it also affects but she's doing well with her medication, and I'm doing well with my. Medication. So it's not like we're two peas in a pod sitting here going, well, we could do this and feel better, better about ourselves. So
Scott Benner 20:07
when you start taking the medication at 13, did depression lift? I don't know the right phrasing for it, or did you still have it? It just wasn't as bad. Just wasn't as bad, okay?
Christie 20:18
But finally, you know they did. I don't even know what the exact term of the test she did for me, but my primaries ma did a, like a gene test to figure out what antidepressants work with you, and what doesn't they they're in, like, red section, yellow section and green section. So by the time she had done this for me, which was just recently, in the last few years, you know, I had been through three or four different medications that absolutely did nothing to me but make me want to jump off cliff. But I finally, at the time, using Lexapro, and that worked for years, yeah, until finally, one day, I just wake up and I'm like, this isn't helping anymore. So that's when we did the the gene test to figure out what ones will actually work with me. So I'm on a new medication, and everything is back to normal, and I've actually been able to decrease my dose. Would
Scott Benner 21:14
you go to Wellbutrin? Cymbalta? Cymbalta,
Christie 21:18
okay, and I know there's a lot of drama about around symbol. So because it's such a strong medication that has a couple of different uses, and they say that the side effects are not worth
Scott Benner 21:30
the outcome. Are you having side effects? I am
Christie 21:33
not, which is wonderful, because there's people that are in a Facebook group that I'm in, that people are literally counting the beads that are inside the capsule to wean themselves off of this medication, because they're having such strong reactions. Wow, I'm like, I'm a lucky one that, no, I don't need to come off it. I've been able to reduce my dose, and everything's working great for me. Did
Scott Benner 21:58
you notice during the two months you were on week ov, did you notice any extra alleviation of your depression? By any chance? No, no, it actually went the wrong way because the medication wasn't working for you, correct? Yeah. I only asked because there's a recent episode where someone talked about glps lifting a lot of of the mental illness impacts that their child was having, and I was wondering, but even if the GLP was helping, somehow, the impact it was having on the other medication was was too significant, you wouldn't have even noticed. Yeah, yeah, I'm so sorry. Gosh, I there's part of me that just wants to pick through that part of your adolescence and try to understand, but I know it's such an unfair question, because I don't think people really know what was happening to them when they were making decisions like that. You know what I mean? And there's part of me that, like you said, your parents couldn't make you, but I mean looking back now with, you know, your sister's kidney inside of you, don't you wish they would have made you. That
Christie 22:56
is why, when I had my transplant, they suggested therapy, because of the regret and the guilt and all of the feelings that come with a major life change. Yeah, I had worked through it, and we were doing well, and then I had a change in insurance, and it's difficult to find somebody that I actually click with that takes my insurance certainly. Yeah, it's tough again. You know, insurances suck, they
Scott Benner 23:21
do, don't they? They really do. Well, listen, you see that you were having issues, right? That different parenting or therapy or something like that might have helped you with as a child, you didn't get it. You figured this thing out a little too late, and you end up with your kidney I'm just failing. Is that what happened? Pretty
Christie 23:42
much, yeah, yeah. During my pregnancy, I ended up with pre eclampsia and noticed my vision changing a lot and having a lot of floaters, and I was diagnosed with retinopathy at that point. And a month after my son was born, I went in and had a little bit of laser in the office, but because I was so young and my nerve endings were so fresh that I couldn't handle it, so all of the procedures I had for that were in an operating room, and that's where I finally realized,
Scott Benner 24:14
hey, you
Christie 24:17
like you could have had a happy, healthy life, but you decided just to give up on yourself and not take the medication, because I didn't know any better. I didn't you know I was diagnosed at four. And I see all my friends doing all of the friend things, and I'm like, I can do it, but then I have to put in the extra effort for the medical side of it, like going to dinner at a new place. How do I carve count this? I don't know,
Scott Benner 24:43
so just don't do it. Yep, it was a lot of that
Christie 24:48
and and then the retinopathy happened, and I I spent the first eight months of my son's life not being able to see very clearly. I couldn't drive until he was born in 2013 August. And in September, I started my treatments. I couldn't drive again until March of 2015
Scott Benner 25:07
so you think the extra stress of the birth and gestating the baby and everything put a lot of pressure on your eyes and your kidneys. Probably,
Christie 25:14
Yep, yeah, because when they they observed me for observation and had admitted me to labor and delivery just to see because I was having symptoms at the same time every night that wouldn't subside. And so, you know, I would go to labor and delivery, and they're like, everything's fine. Your blood pressure is normal, duck, but my I ended up having a maternal fetal medicine doctor because of the type one. And she was like, hey, it sounds a little weird. So let's let's admit you. Let's see what's going on. They did a 12 hour urine, and at hour six, they were like, Okay, your kidneys are shutting down. You have the diabetic retinopathy. Your blood pressure when you were admitted was 199, over 99 we're gonna have a baby either tonight or first thing in the morning. So it was, it was all quick, and
Scott Benner 26:06
were you using your insulin properly during the pregnancy? Yes, you
Christie 26:11
were. As soon as I found out, I absolutely I made an appointment with my doctor, and ended up having to switch because he wouldn't coordinate care with the hospital that I was delivering it. So I ended up switching to a doctor out there. And, you know, we got me on a Medtronic pump and one of their very first sensors that they came out with, but it didn't work with me being pregnant. No matter where I placed it. It wasn't accurate readings.
Scott Benner 26:38
For context, what was your a 1c prior to pregnancy, you know, prior
Christie 26:43
to pregnancy, I was in the nines. When I was pregnant, I was down in the sixes. And then after pregnancy, with all of the treatments and everything, and trying to establish a normal set, you know, after pregnancy, you're still hormonal and all of that, and trying to get levels where they should be was not easy. Yeah. So it took a couple years after my son was born to actually get back to staying in the sixes. Do
Scott Benner 27:15
you know what your highest a once he ever was. Highest was 15.6 you know how many times that happened? Is it like, once or countless, multiple in my teens, multiple in your teens? So you were in the double digit a one sees a lot. Oh, yeah. Okay. Is there anything I want to move forward in the story, but before I do, is there anything that hindsight tells you would have helped you? Like, not like, woe is me, stuff. Like, I wish somebody would have helped me. But like, is there anything that you think right here in this moment, if this would have happened, if someone would have said this, if a doctor would have, if my parents would have, have you had those thoughts? Have you gone through that in your mind?
Christie 27:56
Sometimes I wonder, because when after my son was born, you know, I had seen that doctor for a few years, but she was just like my first doctor. That was, you know, he was my doctor when I was diagnosed, up until I got pregnant, and he was awful because he he would spend time answering his pages while in the room with a patient who has to literally sit there all day long, because they make you see the social worker as a kid. They make you see the dietician as a kid. They make you talk to the nurse and this person and that person. It literally would take me from 10am to 4pm to get out of that office, and I would have to fight to get my doctor's attention to actually do anything. And I felt like he didn't really give a and then I felt similar with the doctor that I switched to while I was pregnant. I had a nurse that was part of my local endocrinology team who had gone to endocrinology clinic about 45 minutes away from where I live, and so I had reached out to her, and she got me in, and I seen a doctor there, and things were great for a little while the health system, when you're calling to schedule appointments, when it's a giant facility, like a university hospital, that you get lost in the system, and that's what I found to be My deterrent from going back there, but ended up there, and I couldn't be happier, because the guy I seen just a few years ago who happened to not retire from seeing patients and the endocrinologist that I have now, they are complete night and day from my previous doctors.
Scott Benner 29:37
You just found the right doctor. Yeah, yeah, that
Christie 29:41
that is exactly how I feel. Is if I had found a doctor to give a and not tear me down every time I walk into the office, because my a 1c, is 15, like, I understand you hate me because I'm a diabetic, but at the same time, give me some freaking encouragement. Man, yeah, I. To live with this, and you don't, I literally wake up and do math to save my life.
Scott Benner 30:06
You have any idea why you were treated that way? Like, do you have any even like feelings like, Is there something I don't mean this this way, because this would not be a reason for a doctor not to do well for you. But is there something about your personality? You visually like anything at all that you think would have rubbed somebody the wrong way and, like, sent them like, I'm not I really want to be clear. I'm not blaming you. This is not like, it wouldn't matter what anybody acts like, looks like, etc. Doctors should give the same care. I mean that I'm trying to figure out, like, why would someone walk into a room see a kid and then just suddenly be like, I'm not going to give them the care they need. He was
Christie 30:44
stretched too thin. Yeah, at the time, there was him and one other endocrinologist in town. And there were many, many, many, many, many diabetes who they had two doctors to choose from, unless they wanted to drive 45 minutes. You know it was they were stretched too thin. And I don't think we had another endocrinologist come in until my original doctor talked about retirement. Do you
Scott Benner 31:09
think it's like Battlefield theory, like, I'll save the ones I can and the ones that are too hard or will take up too much time or too much of my bandwidth, I'm going to skip? Like, is that possible?
Christie 31:19
No, because I, the friends that I have that are t1 in town had similar experiences, whether it was him or the other doctor in town. You
Scott Benner 31:28
know, other type ones in your town that have gone to those doctors that are having significant health issues now, oh yeah.
Christie 31:36
Oh my, if they didn't take care of themselves, the doctor really didn't care. And, you know, I have another friend who, and she's a big, big, big advocate. She, you know, she's in charge of our local What is it now? Breakthrough, don't go changing
Scott Benner 31:52
your name. Expect me to know the new name, but the JDRF chapter is that, right?
Christie 31:57
Yeah, she's in charge of our one want, and she has so many resources. And she then started a support group in our town for the parents of children who are diabetic. And I've gone to a few of those meetings just because I was their kid. You know, at one point, like I was newly diagnosed, this is what I did. This is what I failed to do, and this is how my life has turned out when I did it, it was all without the technology. And now I see like I'm not bashing anybody but the parents that I see comment about, like, the 504 plans, or the IEPs, or, you know, all of that, or having a nurse in the school to take care of it. I didn't have any of
Scott Benner 32:37
that. None of it. Well, it doesn't mean they shouldn't, does it, right? I get that, but to do it without, it's possible, it's possible, but you're making a case that it might not be that possible. So I, you know, like it's, I get your point. Like it's hard, probably to see people complaining about what seems like concierge level stuff when you didn't have basic stuff, right? Correct? Yeah, no, I hear you. I It's got to be difficult. Literally,
Christie 33:04
I went to the office to see the secretary, and she would hand me my little kit with my vial of insulin and my thing. I would call my mother, and she would tell me what to take. Yeah, so she had to be phone available at all times of the day. You know, if my sugar was high and I didn't feel right, I would have to be able to get a hold of her to go, you know, what is my correction? What do
Scott Benner 33:29
I do? I mean, it's just it sucks. I'm, you know, the whole thing sucks. It does. Yeah, your kids, how old now? Like 11. Do you say? Yeah, yep, He's 11. So is it fair to say that for 11 years, you've known how to take care of your diabetes. Yeah, have you been doing it the entire time, except
Christie 33:45
for the first few years after he was born? Because of the hormones and everything, I was doing my best, but I couldn't perfect it. Okay, like right now after my transplant, they want my a 1c under seven, but I'm also on steroids. On the daily I take prednisone every night, and it's really difficult to try and figure it out, to the point my doctor has told me to take ghost carbs because my sugar spikes, but it doesn't spike for long, so having a different basal rate at that time doesn't really help, and it's not always the same time at night. Because of my work schedule, you
Scott Benner 34:21
have a variable work schedule. Your weight is not optimal. You're taking steroids. You're on immuno blocking medications. You're on medication for depression and for thyroid. Am I missing anything? Blood pressure,
Christie 34:38
cholesterol, okay, all of the things, the blood pressure medication right now is just a preventative because of the kidney. Sure. You know, my blood pressure had gone back to a normal baseline after my transplant, but you know, I'm just now getting to year two in November, so it's taken some time for my body to readjust, and lately, I. Been going to the doctors, and every time they check it, it's low. So I reach out to my cardiologist. He wants me to do the daily checks and write it all down for a few weeks and then send it in, and he'll
Scott Benner 35:11
make adjustments. Are you willing to say how much weight you think you need to lose when I
Christie 35:15
started? We'll go v here. Let me preface this by saying my entire life, until I got pregnant. I was under 140 and I got pregnant, and I gained the baby weight, and it took a little while for me to get it off, and I was back to my baseline. But after my transplant, I gained almost another one of me. I was at 221,
Scott Benner 35:40
when we started with govi and I was at 205. Yesterday. How tall are you? Five? Four. Okay, so you feel like you have 6070, pounds to lose. Oh yeah for sure. Okay,
Christie 35:55
I would prefer to get back down to my baseline of under 140 but with the prednisone and the fact that I'm still struggling with energy after my transplant, that I don't know if I'm ever going to get back there, but I will be happy enough to be under 200 but definitely want to get back to where I can get a pancreas so I have to lose the 60 to 70 pounds for sure.
Scott Benner 36:19
Yeah, I'd like to get back to where I was when I was 15, but I don't know how that's gonna go. So your problems right now, this is what you wanted to talk about on the podcast, right? So we're good to, like, pick through this. Is that right? Yeah, whatever. Yeah, all right. So actually, before we start this, how'd you find the podcast?
Christie 36:35
I don't 100% remember, I believe that I had joined another T, 1d group on Facebook, and you've actually interviewed the girl that I became friends with, blue.
Scott Benner 36:48
Oh, of course. She lives in I know we're shooting, yeah, yeah, of course. So we have
Christie 36:55
hit it off. We talk all the time. You know she if I have questions, because, like, I switched to the Omnipod, and I knew she was on it, you know, I had questions. I was like, well, I could go to my friend who lives local, but hasn't been on it very long, and didn't take a whole bunch of care of herself. She was kind of in the same boat as me, but now she's doing very well. She contributes her great blood sugars to using Plexus products. Okay, so to each their own right, I hear, well,
Scott Benner 37:28
blue is terrific. First of all, she's lovely. Yes, she is, yeah, and she shares the podcast with a lot of people, which I really appreciate. I didn't realize that's how you learned about it. Has it helped you? You see it as like, listening to people's stories, which is valuable? Or do you see it as like, there's management care in here, and I, I like to learn about that. There's both.
Christie 37:49
And I'm the type of person that I don't want to learn just one thing. I want all the tips and tricks. Yeah. So what works for you might not work for me, but I still want to know about it, because it could help somebody else that I know that's got t1 you know?
Scott Benner 38:03
Yeah, I feel the same way. I I was surprised one day, this is years ago, when someone said that guy thinks if I do exactly what he does, it'll work for me. And I thought, I don't think that. I thought I'm just sharing what what I'm experiencing, you know what I mean? Like you could, you should pick from it a la carte. Maybe it all works for you, but you don't have to do everything. It's such a weird thing that that somebody would think that I that's a perfect idea to me. Like hear things and decide for yourself. You know, you had your a 1c down for pregnancy with help with the doctor a couple years after the pregnancy, you think you were fighting with your hormones? Does that mean you were having trouble, like focusing on yourself.
Christie 38:41
It was a lot of different things. It was the fact that, you know, I had been going through the retinopathy treatments and being a brand new mom, throw divorce in the mix a year after my son's born, and then, you know, just trying to get back to being baseline with everything in my life. Wait,
Scott Benner 39:01
wait, some guy knocked you up and then watched your kidneys and your eyes explode and left you. Yeah, yeah. He's great.
Christie 39:12
He's a real winner.
Scott Benner 39:15
Oh, my goodness, I'm sorry. You know, every day I get up, I turn this microphone on, I think someone's gonna tell me something that's gonna make me feel good about the world, and then it doesn't happen. Usually, that made me I'm angry. Now I could feel my body temperature go up like, you know what? I mean? Never mind. Okay, well, Jesus, God damn, that made me upset because you're in the middle of a medical issue, and you just had a baby, he couldn't handle it. He couldn't handle it. It's not that hard to be, like, supportive. It just really, isn't you just sort of like, stay there and go, Hey, is there anything you need? Can I do something for you? What would help you want to talk right? Like, isn't that really kind of it? You. Yeah,
Christie 40:00
yeah, it would be great. But people suck. Jesus, all right, some, some, yeah, no, there's no good ones out there. They're lovely
Scott Benner 40:08
people suck. Yeah, there are lovely people everywhere. But, I mean, my God, like, I don't, I don't know. I'm sorry. It's just okay. Couple years after the birth, you kind of like everything starts to coalesce for you. You keeping your a one, CS, they told you under seven. Is that what you were doing?
Christie 40:26
Yes, yes. And I have had it under seven since my transplant. Actually, yesterday I seen my Endo, and I was at exactly seven yesterday. That's excellent. And my my Dexcom clarity tells me I was 7.5 so I've noticed there's a little bit of variable between the clarity app and what actually results.
Scott Benner 40:50
Yeah, like your a 1c can be weighted towards more recent. So if you over the last three months, were more like 7.5 for two months, then in that last month, were more like 6.5 I could see where your a 1c would look more like seven as an example. Yeah, yeah, yeah. Tell people what you're doing right now to keep your a 1c at seven. Like what I mean, like functional steps.
Christie 41:11
I'm actually taking care of myself. I mean, I Not gonna lie. I do still indulge in some chocolate now and then, but I am watching my portions. I'm watching, you know, are they the complex carbs? Are they simple? You know, do I need to extend this Bolus, which I never used before, and I know that with the OP five that we have to put it back in a manual mode to be able to extend a Bolus, which on nights that I eat a ton of pasta or a lasagna. Obviously, I'm going to do that. But you know, even when I order pizza, now, I'm ordering a thin crust with armed garlic sauce instead of marinara, and I take half the insulin I would for a regular pizza, yeah,
Scott Benner 41:55
just little less dough, little less cheese. Big difference, right? Yeah,
Christie 41:59
yeah, I'm taking my medications. I have to take them at a time to interval because of the immunosuppressants. So every 12 hours, you know, I wake up, I get things around. I take my medication, typically between 930 and 1030 in the morning, and then at night, I take them as soon as I can, if I'm home, if not, I'll take just my immunosuppressants to work. Take them between 930 and 1030 okay, but at the same time, I'm also trying to focus on I have to take the prednisone that's at the 12 hour mark, so I need to take a couple extra units of insulin. I know it's not practical, but the doctor was like, there's not really much else we can do but the ghost carbs to try and combat that. And it's not every night that I shoot up to 300 with the prednisone. It's a lot to try and figure out. Like, what did you have for dinner? Is your blood sugar going to spike in a little while because of dinner? And then do you need extra on top of that for the prednisone? Or, you know, if I just eat lunch meat and a piece of cheese, you know, just to keep myself steady for the night, I don't have to worry about that giant spike to 300 it might only go to 215 Okay, with the prednisone. So there's a lot of overthinking everything. To do it, I have to be thorough and continuously make sure that I'm doing it properly, and getting everything in on time, and then assessing how things, you know, might go from there, right? Because, obviously, it's not an exact science. The wind is blowing from the west, you know, there's it rained for a whole two seconds earlier, and my blood sugar wants to spike just because
Scott Benner 43:41
of that sort of sounds like, right? It just, it just feels like everything, yeah, everything's making it move. Yes. You're seeing where the food's impacting it and how your medication is impacting it, and you're trying to combat it. You're not just staring at it and going, well, I guess this is what happens, right? What's the prednisone for? Again, I think you told me, but I don't remember,
Christie 44:00
prednisone is part of it's the steroid that's part of the immunosuppressants that I take, okay,
Scott Benner 44:07
and without them, just so people who don't know, your kidney is going to fail. Without those drugs, my
Christie 44:12
body will reject my kidney. Yes, yeah, okay, the main one is called Tech row. That's the short term for it, because I can't pronounce the whole word, but that main one has to be between a certain level. And if it's not, you can have something called Tech or toxicity, which, when I was dealing with, we go V, and my labs being off with that number was way too high, which is what drove down my kidney function at that time. Yeah, but has since, you know, they changed my dosage and has since gone back to normal. Okay,
Scott Benner 44:44
so your goal here? Well, let me say this, first, did you go back to work? Had you not been working and you're working now? Right?
Christie 44:51
Yep. So I had my transplant in November of 2022 and it was through the paired program, so my sister didn't match me. But she matched somebody who had a donor, who matched somebody else, who had a donor, who matched me. So there were three donors and three recipients that day. The
Scott Benner 45:08
best basketball trades are made that way. By the way. Christy, you ever noticed that you're like, we need a center. They've got a Ford. That guy over there needs a Ford. I have a set. And you just sort of do that horse horse trading well, so your sister donated a kidney to a stranger so that a stranger would donate a kidney to you, correct?
Christie 45:26
Oh, that's right. The thing is, is my sister is six years and exactly one week older than I am, and so when I was diagnosed with diabetes as a young kid, you know, she always knew that someday I could potentially end up on dialysis, which, thank God I never did. There's a possibility I could turn out like my grandmother, who had type two where, you know, she she lost some toes, she was permanently in a wheelchair, she was on dialysis and still taking insulin, but still had a bowl of Skittles on her table every day.
Scott Benner 45:57
How long did she live? She
Christie 46:00
was in her late 60s, early 70s, if I remember, right, I'll
Scott Benner 46:05
tell you for a living like that. That's a that's not a bad run, you know, right? Yeah, yeah, you would. I expected you to say she passed more than her, like, mid
Christie 46:14
60s. When she was doing dialysis. She still didn't really take care of herself, but she was on dialysis for, I believe, about 10 years before she passed. And that's a long time for somebody to be on dialysis. Yeah, yeah, no kidding, so, but she was never eligible for a transplant, so Well,
Scott Benner 46:36
jeez. Okay, tell me why you wanted to be on the podcast. Just
Christie 46:40
one more person to learn from. You know, this was my experience, and this is the possible outcome if you don't take care of yourself. You know, I know there's millions of parents who have T, 1d kids, and they're like, What could possibly go wrong? Hi, I'm that bad example.
Scott Benner 46:58
Hi, I'm Christy, and this is what happens if you don't take your insulin?
Christie 47:01
Yes, yes, exactly. But the thing is, is I hope that people can learn from my story, because everybody told me my grandma's story and tried to scare the shit out of me, and I still didn't take care of myself.
Scott Benner 47:13
Yeah. Do you think that you thought, oh, that happened to my grandmother. It's going to happen to me. So there's no sense in trying, no, no, you just
Christie 47:23
don't rebelled the idea never pictured, Yep, exactly. I never pictured needing a kidney transplant. I was gonna eventually be okay, but no, You never get out on unscathed. Never. It's
Scott Benner 47:37
like, I say all the time. It's like smoking. Like people always they smoke cigarettes, and they're like, it's not gonna happen to me. It's somebody else. Somebody else gets lung cancer. It's not me. And, you know, once it happens to you, it's too late. And then you're like, oh, okay, well, it happened. And then you feel like you need to tell somebody else so it doesn't happen to them. That's where you're at, yeah, yeah. Well, it's nice of you to do. I appreciate it. And you certainly haven't done it in a scary way, and I appreciate that as well. You're just telling your story about what happened. Well, you were never on dialysis. Is that correct?
Christie 48:07
No, so I was lucky enough to catch it in time to where I wasn't having a whole lot of symptoms, like I had a little bit of the leg swelling, but it wasn't to the point where I couldn't stand all day and, you know, have divots in my legs from from the swelling.
Scott Benner 48:26
Yeah. What's that called? Pitting edema? Yes, yes. You know, he
Christie 48:31
put me on the preventative medications to kind of help what function I had left. And then was like, Okay, it's time to refer you to transplant that way. When you need one,
Scott Benner 48:42
you'll already be on the list. Okay, so I was on the list,
Christie 48:47
and it was 100 and 144 days from the time I was listed, active to the time they found a potential match in the paired program. Not bad at all. No, not at all. I was extremely lucky. And in that, you know, it was, it was really fast. And I, you know, I always worried, like, Okay, I can't get my sister's kidney. She's got antibodies that I don't have, or I have antibodies fighting her. I don't remember which one, but she got a phone call, actually, on my birthday in October of 22 and she text messaged me, and she's like, it's not 100% confirmed yet, but happy birthday. I got your kidney. I found
Scott Benner 49:31
a lady who has a kidney for you. I'm gonna give it to her somebody, and she can Oh, well, it's good birthday. Yeah. So Christy, I don't know how much of the podcast you've actually listened to, but I grew up with a friend who was diagnosed with type one when we were in right at the very end of high school. He's gone now, you know, he was on dialysis the end of his life. He died of a heart attack, like as you're telling your story. I think Mike was taking his insulin, but he just didn't know how to do it, you know? And. He is a bright guy and a thoughtful, lovely person, and everything else that you would want in a, you know, in a friend. And he shouldn't have been overwhelmed by this, but he definitely was. And I think that the more time that goes past, and the worse your health gets, and the more you're foggy when you're high and irritable when you're low and nobody's helping you, you don't know what to do. I can see how it could be like, like getting knocked over in the surf, you know, and just being tumbling through the waves and not knowing which way is up and and just maybe giving up. And, I mean, I guess thank God that that neck got you pregnant, because it sounds like it might have saved your life, you know, I wish somebody would have got Mike pregnant, is what I'm saying, and he would have thought that was very funny. So I don't have any trouble saying that. It's such a shame, you know. And I put out the Grand Rounds series this year to try to impact this, and I know it's not going to help as much as I needed to, but doctors don't understand that a couple of bad words or a weird look or disinterested, you know, checking your your messages during a during a, you know, a conversation with a kid could mean that 30 years later, that kid doesn't have a kidney and is on prednisone and can't lose weight. And you know what I mean? Like, I don't know that they know that, but I wish they would listen. I wish they would hear your story, you know what I mean, and say I got to do better at this, or I can't have a bad day. Like, I don't get to go to the doctor's office and be distracted today, like this kid needs this, and if I can't give it to them, let's find somebody that can, because otherwise this is a real possibility, you know, down the road.
Christie 51:49
And I think a big help in a lot of my experience anyway, is that the follow, the follow app that we have is amazing, like my mom used to hound me all the time. What's your blood sugar? Are you taking your insulin? But I'm almost 36 like, that's not her job anymore, right? But I have a best friend, Caitlin, who has actually been a life saver if she gets an urgent low for me, if I don't contact her within, you know, 510 minutes, she is on the phone, calling my mom, saying, what's going on? Where is she? She needs help.
Scott Benner 52:27
That's excellent. I swear to God, it's it. People need support. Without her
Christie 52:33
doing that like ever in my life, I've only been unconscious twice, and once it was once when I was seven, and once, two summers ago, and she had messaged me and said, You're really low. Are you okay? I messaged her back, but it didn't make sense. But because I had messaged her back, she thought I was okay, and I ended up waking up to, I think there were two paramedics and two firefighters in my room sticking me with Dex 50 in an IV, and that's when we came up with the plan. Like, if I don't make sense, if I don't answer you in a certain time, call somebody who knows what's going on and where I'm at. Okay, my parents know where I'm at because they help watch my kid when I'm not out and about with him.
Scott Benner 53:20
I think that support, I don't care how old you are, and anybody who would say you're an adult, take care of it yourself. Like, honestly, for me to go yourself right? Like, some people need help and and even if they don't need help, helps nice and it alleviates a lot of this, like excess pressure and stress on people like Arden just moved into a different dorm room this weekend, and it's a key card to get into the room. And then once she's in the room, it's a two bedroom, then she goes into her bedroom, and her door closes automatically and it locks every time, oh no. And I'm like, my wife and I are driving home. We're like, that's not okay. Is there something we can do about that, or is she just locked in a box every night by herself? You know what? I mean, she's trying to assimilate to the new school, and we're letting her, obviously, like, have a couple of days, but this is the thing we can't, like, we got to get back to this, right? You know, we absolutely have to figure out what to do about this, because she needs those other two girls in that other room to know how to like, to be able to get in there if they have to. And you say that to her, and she goes, No, I'll be okay. And I know she thinks that, and she probably will be, unless she's not. And then what, you know what? I mean, it's scary. Yeah, it just sucks. Like it sucks. You have to think about it, and it's nice to have somebody else helping you think about it. Now you have to be willing to let them, you know what I mean, right? But that's another story, I guess that's just right, yeah, that's growing up. Honestly,
Christie 54:54
it's literally been since my divorce was finalized that she was like, Okay. Let's, let's do this. I am now your person. You know, I'm gonna download the app and we're gonna have this plan, and now, you know, if I notice that I'm dropping I'll message her and be like, This is my treatment plan. This is what's happening. You know, I've got fruit snacks on board. I've got juice, I've got a thing of glucose tabs. I have my G VO, you know, I've got all of this handy, but this is what I'm treating with right now. You know, if I end up treating and I'm okay, but I'm still lagging a little bit where it continues to drop before I actually stabilize, I will message her and say I've already treated. It's just waiting to catch up. This is what my finger poke says, excellent, you know. And she, she works three jobs, and she still does this for me, like she, she is my person. Always will be, always has been. It's life changing to have somebody who actually cares, who wants to learn, like I've taught her how to carb count, you know, certain things. Or this is why I take this much insulin for this meal, or this is my correction factor. I'm at this number. We want to be at this number. This is how much I take. And she always asks questions. Yesterday, I was talking to her about the will go be in the transplant for the kidney, and then, you know, possibly getting a pancreas later on down the road. And she's like, but do all diabetics struggle as much as you do? And I said, No, there's people who have, you know, they're got tight control. Their tir is, you know, 97% and they eat a keto diet, and I'm like, I work different shifts every day. I have a 11 year old that does not like healthy and I'm not going to make two different meals. I'm just going to watch my portions, and it's a lot, but you do what you got to do, and not everybody has the same experience. And I think that some people don't understand, like, oh yeah, my grandpa's type two. And, you know, he he changed his diet and exercise, and, you know, you eat a spoonful of cinnamon, or, you know, some okra water, and you'll be just fine. It's not the same. I don't have the crayons to explain to people how it's not the same, yeah, but it did need a t1 in the wild the other day. He was great. He's a bread Benner. He was wearing the g7 with the bionic pump. And I'm like, I know you're working, but can I ask you questions? Yeah. So we sat there and talked for 15 minutes about his pump and his experiences. And you know, he's like, Well, how long? And I was like, I was 31 years and I've had a transplant, and just make sure you take care of yourself. It's
Scott Benner 57:46
very nice of you to share that with him. Very much. So So tell me what's going on now you went back to work, and so now you have activity, and you didn't have this activity before, but you're seeing low blood sugars at work.
Christie 57:59
Yeah, like I said, I had even gone to work the other day at 300 because I had just eaten and didn't Pre Bolus, and I still tanked down to 54 and I'm like, but I was on the register for two hours, or I was bagging for two hours, or I was doing a mix, you know, and it's like, it just came back From break, I sat down, my number was fine. I even eat like, two glucose tabs. When I noticed that I'm trending down, and I get to a certain point, it doesn't help. And it's, I think a lot of it is, is the pump is used to me just doing minimal things and not long periods of activity. But then again, when I would do laundry at home before I started working again, I noticed that, you know, if I'm doing two or three loads, I'm dropping at the end of it, and that's because I'm carrying everything going down the stairs back up the stairs, and, yeah, it's a lot of movement that I didn't have after my transplant. So
Scott Benner 58:57
how many days are you working a week? It depends
Christie 58:59
on what they have available for shifts and what needs to be covered for days off. But typically I'm three days.
Scott Benner 59:08
My thought is, obviously you're on Omnipod five, and it's probably right about the time it's getting used to you sitting around the house more you're going off and working for a few days, and then you're getting low right? Because it's, it's like you said, you're set more sedentary. It's giving you more insulin. Now suddenly you're moving. You don't need all that insulin. You're getting low. My thought here is, why don't you exercise on the other days that you're not working, so that your insulin needs get matched up? Still minimal? Yeah, right. Because the alternative, Christy, I don't love the alternative for you, which is go the other way with it, which, you know what I mean, like go into manual mode when you're working, or because it's also not going to help you. You know it's not going to help you if you go high then, then the algorithm is not working right. Most of the time, we hear this problem, and we try to find a way to fit the insulin around the problem. Um, I don't know if that makes sense or not. I think you should just do more exercise, because it doesn't sound like it would be a ton. You need it anyway. It's something you're trying to do, right? So do some minimal exercise every day that mimics working, and then let the Omnipod five catch up with your new insulin needs. And then you shouldn't get low while you're at work, is my thought,
Christie 1:00:19
right? And I have plans to do that, but still, I'm building up my stamina to be able to work eight hour shifts, like I went from just doing laundry at home or dishes to physically being active every day. Yeah, that I'm working, and so the days that I'm not working, my body is sore and I am exhausted, and I know that I need to continue keeping up with the moving and everything. I just have to do it in smaller increments. Nothing wrong with that, either. My energy level since transplant has not come full circle. Yeah, and it doesn't help that I've had the weight gain and all of the medication changes, but it's no excuse. I still need to be active. But I did see my endo yesterday, and she was very pleased. And I'm still at seven, and she is fine with that for now. And now that I'm back doing work, she is glad, because obviously we're seeing the lows, but at the same time, being active is going to help me lose some more weight, and all of it. So she made, she made some changes.
Scott Benner 1:01:26
You don't have to lift them out. And I'm not saying that, but Right, just get up and walk. You know what I mean? For 1015, minutes a day, and then try 1520, minutes a day, a week or two later, I understand the necessity. I mean, my wife had long COVID, and probably still does. To some degree, you have to learn to change your idea of what exercise is. Exercise is what it is for you. Like, nobody's saying, like, go run five miles or lift for two hours. Like I'm saying, Get up, move around. Like, if doing the laundry is a thing, then great, spread out the laundry. So you do a load of laundry every day, instead of three loads one day. Like, if that's activity for you right now, then great. Then do just try to do some a little bit every day. And then, not only I think, will that help you, you know, build up quicker, but I think it'll help your insulin level out as well, right? That makes sense. Yeah, yeah. I would try that first honestly, but explain to people, what does exhausted feel like? Like you work for a couple days in a row, and then what happens to you? I
Christie 1:02:27
feel drained of energy like, you know how you see the Energizer Bunny, and he's got the battery in his back, and, you know, with the off brand, he ends up dying in the middle of the commercial. That is how I feel some days. Yeah, where I get off work and I'm like, Oh my God, my body absolutely aches and my feet hurt, and I am exhausted and I can hardly hold my head up. There's nothing there. But right at the same time, I'm also experiencing two to three lows per shift, if I'm working in eight hour shift, you know? So it's like, I'm treating, and then I'm dropping, and then I'm treating, and then I'm dropping. It's a mix of both.
Scott Benner 1:03:03
Sucks. It does. Yeah, I actually have to leave for work here shortly. Do you Oh, I'm gonna have to let you go. Yeah, okay. I don't want to get you I don't want to get you in trouble.
Christie 1:03:13
I'd ask for some time off, but they scheduled me a little sooner. Can you still imagine going
Scott Benner 1:03:18
to work and be like, I was recording a podcast, they'd be like, we don't care.
Christie 1:03:23
They know what I'm doing this morning. I was like, I might be a minute or two late. Wow. I don't want you to be like, well, that's awesome. They are so supportive where I'm working, right of, you know, getting me off of register if I absolutely need to. And, you know, do you have all your low snacks? Do you need anything? You know, it's, it's really amazing when it you come to a new employer and they just understand, I actually found another t1 that I didn't know worked. There
Scott Benner 1:03:50
more support. That's what you're seeing. Yes, yep. She's like, Oh, by
Christie 1:03:54
the way, I've got low snacks if you ever need them. I was like, I've got a pouch full of them too. So, you know, same goes for you.
Scott Benner 1:04:01
We also want to get you not going low, because no reason for extra calories. You know what I mean? Like with this, with the lows, like, not that, don't get me wrong, stop your lows. But we want to get you to a point where you're you're not getting low, so that you, you know, continue to lose weight. Have you ever been through the Pro Tip series, or there is also a series for Omnipod five about how to set it up. Have you seen that content? There's a couple
Christie 1:04:24
of them that I've heard from that series, but I don't have a lot of free time, so usually I'm listening at night, time before I go to bed. Yeah? So I get bits and pieces. Well,
Scott Benner 1:04:36
there's a Omnipod five Pro Tip series about setting up the Omnipod five that's worth listening to because it talks a lot about how it works. And there's also, you're in the Facebook group, right? Yes, of course. All right. So here's this, I like how you said, of course, because it's the only Facebook group to be in if you have diabetes. That's what you meant. If you go into the private Facebook group, go into the featured tab, there's lists of C. Series in there, so you can see what episodes they are. The Pro Tip series is in there, which is a lot about using insulin might might be valuable for you. There's a lot of Omnipod five stuff in there, in the algorithm pumping. There's conversations about Omnipod five with users. There's the Pro Tip series that I made in conjunction with insulin. There's an Ask Omnipod five expert series I also made with insulate. There's a lot of good information in there. It might, it might help you, just like you said, just to have bits and pieces that you can build on,
Christie 1:05:28
right for sure. And you know how blue tells all of her friends, I tell all of my friends, like my new friend in the wild, I told him, I was like, You have to listen. If you don't listen, at least join the Facebook group, because there's so many different resources and questions and answers, and even if something doesn't work for you, you still have that tidbit
Scott Benner 1:05:49
and knowledge. Yeah, no, I
Christie 1:05:50
agree. And that's what I enjoy about being in the Facebook group, is that I see so many posts that are different.
Scott Benner 1:05:56
Yeah, there's no better way to I mean, right now, I don't see through technology. There's no better way to make a community, especially out of a situation with like type one diabetes, where you're just not going to meet that many people in your real life that have it. So you know, to be able to see people from all walks of life, from all areas of the country and the world come together and talk about it, and to see the similarities that they all are experiencing very similar things. I just think it's incredibly supportive and necessary, honestly, to have that kind of community around
Christie 1:06:27
you, exactly like I said, I've met quite a few being in that group that my friend created for the parents and, you know, a support group for adults would be great, but it's just not something that everybody can make time for. You know, everybody has kids in school and work, and it's been difficult, but I actually made a new friend who actually on Tik Tok was sharing her kidney transplant story, and her name is Natalie, and she lives 45 minutes from me. Found
Scott Benner 1:06:53
her like that. You know, I have to tell you, I disagree with people are like, well, there should be an adult group and a parents group into this group, into that group. I'm like, I don't think segmenting you is a good idea. I think I get like you mentioned it earlier, right? It can be frustrating to see a parent complain about something that you know would have looked like icing on top of your cake when you were a kid. At the same time, seeing other different perspectives, but still in the same arena, I think is helpful. It's irritating to you, but if you're not angered by it, and you know what I mean, and maybe it teaches you to expect more for yourself, like those people want everything they need, and they're gonna get it. And maybe that rubs off on you a little bit. You say, You know what? I'm gonna get everything I need. Who knows? Like, who knows how that interaction is going to end up helping you or helping them. Maybe you end up saying back to them, my gosh, like, when I was growing up, like, this would have been a luxury of all luxuries. And maybe they'll think, yeah, we're lucky, you know, like, who knows how that helps? But I think having a ton of people with diabetes, I also like there being type twos in there. People have gestational whatever, right like or loved, loved ones, even like, Forget caregivers. There's a ton of grandmoms in there who's like, grandchildren have type one. They don't have it. They don't take care of their grandchildren that often, but they get to understand it better. I love that about it. I would always make an argument for being integrated and and welcoming and letting everybody who's touched by diabetes be in that space. It's kind of how I think about it. But I want to get you to work. I don't want you to be late, and don't forget to charge your phone again. You said for this, I don't want you. I don't want
Christie 1:08:29
your phone dying. Oh, no worries, it's not gonna die. And then I've got my PDM for the Omnipod if my phone doesn't work, so it's not like I'm not gonna miss my alerts, and I've got my watch on. Look at
Scott Benner 1:08:40
you. All right, excellent. Go get them. Christie, thank you so much for sharing this with me. I really do appreciate
Christie 1:08:44
it. Yeah, no problem, Scott, thanks for having me on my pleasure.
Scott Benner 1:08:53
Today's episode of The Juicebox Podcast is sponsored by the Dexcom g7 and the Dexcom g7 warms up in just 30 minutes. Check it out now at dexcom.com/juice, box. Guys, you want to go for a walk with touch by type one in Orlando, you can do it and you can have a great time. Meet a lot of wonderful people touched by type one.org Go to the Programs tab, click on Steps to a cure and get yourself registered right now for the beautiful walk that's coming up on March 8 in Orlando, touched by type one.org Earlier you heard me talking about blue circle health, the free, virtual type one diabetes care, education and support program for adults. And I know it sounds too good to be true, but I swear it's real. Thanks to funding from a big T 1d philanthropy group, blue circle health doesn't bill your insurance or charge you a cent. In other words, it's free. They can help you with things like carb counting, insurance navigation, diabetes technology, insulin adjustments, peer support, Prescription Assistance and much more. So if you're tired of waiting nine months to get in with your endo or your edge. Cater. You can get an appointment with their team within one to two weeks. This program is showing what T 1d care can and should look like. Blue circle health is currently available in Florida, Maine, Vermont, Ohio, Delaware, Alabama and Missouri. If you live in one of those states, go to blue circle health.org to sign up today. The link is in the show notes, and please help me to spread the word blue circle health had to buy an ad because people don't believe that it's free, but it is. They're trying to give you free care if you live in Florida, Maine, Vermont, Ohio, Delaware, Alabama and Missouri. It's ready to go right now. And like I said, they're adding states so quickly in 2025 that you want to follow them on social media at Blue circle health, and you can also keep checking bluecircle health.org to see when your free care is available to you. The Diabetes variables series from the Juicebox Podcast goes over all the little things that affect your diabetes that you might not think about travel and exercise to hydration and even trampolines. Juicebox podcast.com go up in the menu and click on diabetes variables. Thank you so much for listening. I'll be back very soon with another episode of The Juicebox Podcast. If you're not already subscribed or following the podcast in your favorite audio app, like Spotify or Apple podcasts, please do that now. Seriously, just to hit follow or subscribe will really help the show. If you go a little further in Apple podcast and set it up so that it downloads all new episodes, I'll be your best friend, and if you leave a five star review, ooh, I'll probably send you a Christmas card. Would you like a Christmas card? The episode you just heard was professionally edited by wrong way, recording, wrong way recording.com, do.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!