#1447 Diabetes Pro Tip: Insulin Resistance
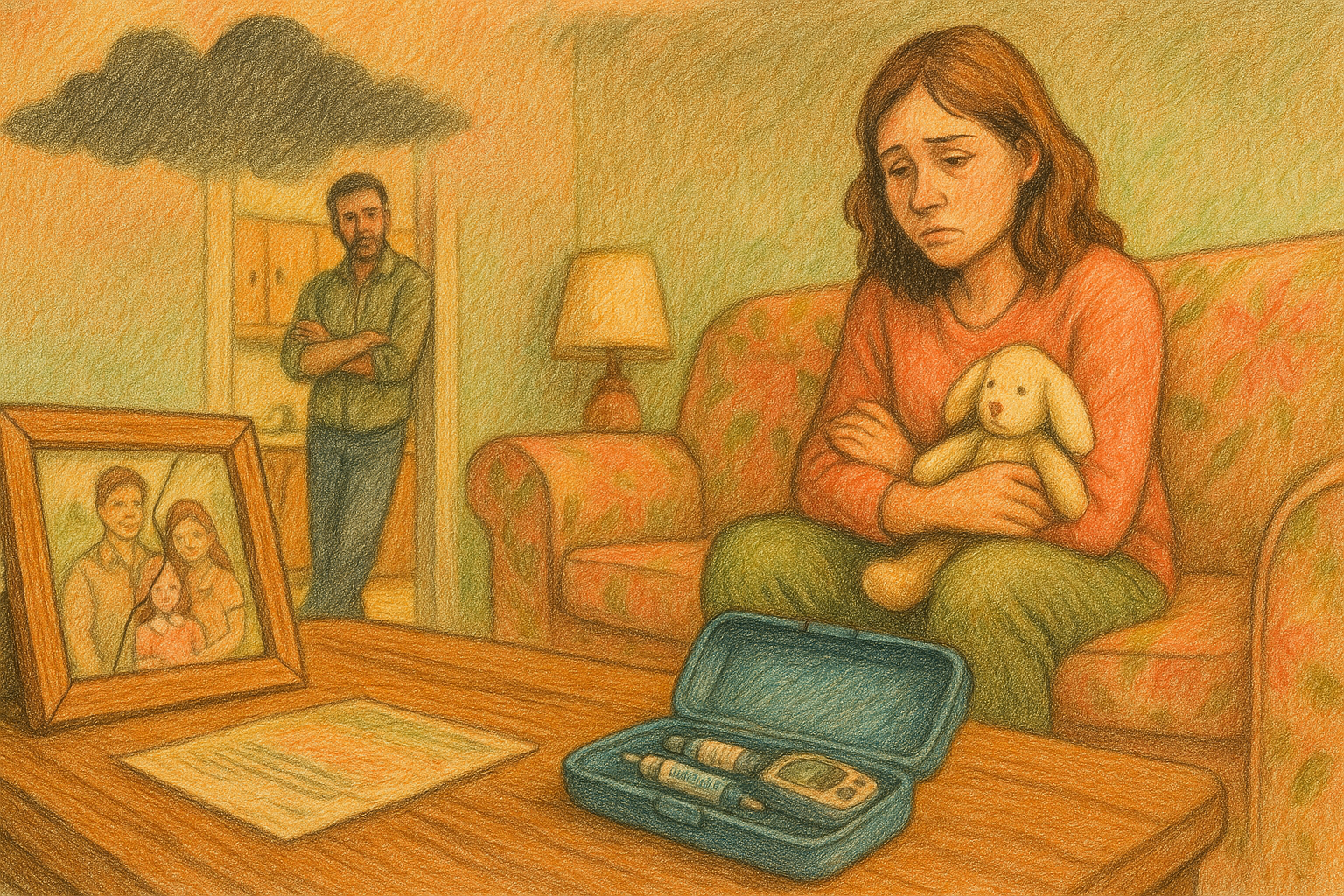
Jenny and Scott break down what insulin resistance and diabetes.
You can listen online to the entire series at DiabetesProTip.com or in your fav audio app.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - Radio Public, Amazon Alexa or wherever they get audio.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 00:00 Here we are back together again, friends for another episode of The Juicebox Podcast. Today I'm adding to the Pro Tip series. The rest of the series runs from episode 1000 to Episode 1025 it's also available at Juicebox podcast.com, up top in the menu, look for diabetes. Pro tip, please don't forget that nothing you hear on the Juicebox Podcast should be considered advice medical or otherwise, always consult a physician before making any changes to your health care plan or becoming bold with insulin. When you place your first order for ag one, with my link, you'll get five free travel packs and a free year supply of vitamin D drink. Ag one.com/juicebox, don't forget to save 40% off of your entire order at cozy earth.com. All you have to do is use the offer code juice box at checkout. That's Juicebox at checkout to save 40% at cozy earth.com. Are you an adult living with type one or the caregiver of someone who is and a US resident? If you are, I'd love it if you would go to T 1d, exchange.org/juice box. And take the survey. So if you'd like to help with type one research, but don't have time to go to a doctor or an investigation and you want to do something right there from your sofa. This is the way this episode of The Juicebox Podcast is sponsored by Medtronic diabetes and their mini med 780 G system designed to help ease the burden of diabetes management. Imagine fewer worries about mis Bolus is or miscalculated carbs thanks to meal detection technology and automatic correction doses. Learn more and get started today at Medtronic diabetes.com/juicebox the episode you're listening to is sponsored by us. Med, us. Med.com/juice, box, or call 888-721-1514, you can get your diabetes testing supplies the same way we do from us. Med, Jenny, we're going to do something that we don't do that often. We are going to add to the Pro Tip series today. Yay. Right? We are gonna talk about insulin resistance.
Jennifer Smith, CDE 02:23 Oh, the fun of insulin resistance. Did you hear all
Scott Benner 02:27 the clicking? Everyone's like, reaching for their phone. They're like, Oh, I don't notice this.
Jennifer Smith, CDE 02:32 Turn this off. Let's fast forward and see if they talk about something. Guys
Scott Benner 02:34 say, insulin resistance. Did she pretend to be excited about it? What's happening right now? But we think this is very important and very important to add to the Pro Tip series. So we're just going to jump in with, you know, starting at one, what is insulin resistance in type one and what drives it? Let's talk about that first, make sure we understand awesome.
Jennifer Smith, CDE 02:54 So I think it's important to again, define kind of insulin resistance as what's happening in the body? Like, why are you using a ton of insulin? That's what I think most people on a very like, just low statement level, I use a lot of insulin. I must have insulin resistance. That's not necessarily true, and I think that begs definition as well. Overall, the definition of insulin resistance is the body is impaired in response by some specific tissues in the body to actually using insulin, well, which then decreases glucose uptake or movement of glucose out of your bloodstream into those cells, right? And the main sort of tissue receptors for insulin that become resistant are your liver cells, your skeletal cells, and then your fat cells. You might also see them called adipose tissue, but it's just fat cells, essentially, and it really means that your body just isn't it's not allowing the insulin to open the doors on those cells and allow the glucose to come in so our body doesn't essentially dispose of glucose the right way. I mean, it's the defining piece of type two diabetes. And while we really want to talk about type one, I think that's the piece that is misunderstood, because it's happening in type one and type two in a in the same way, but potentially and potentially for some of the similar reasons, right? But type two, we may eventually get to insulin resistance by not really seeing blood sugar changes, right? Because the body is actually trying to compensate for those cells not using insulin. Well, the beta cells just put out more and put out more and put out more insulin, and eventually they kind of get pooped out, right? So in type one, I think it's important to then define we can have insulin resistance in type one, but there might also be times where insulin. Needs are very high. And that doesn't mean you have insulin resistance that is long term a problem, right? So to defining those time periods really insulin resistance for time specific could be puberty, your child or teenager may use an excessive amount of insulin because there is a lot of growth and a lot of stuff happening. But unless your child is also obese, has elevated blood pressure issues, has issues which with low HDL levels, kind of the metabolic pieces that we're looking for that coincide with insulin resistance or metabolic syndrome, right? You may just need more insulin steroid use. You need a lot of insulin for using steroids and some other medications or other medical treatments. You may have excessive use of insulin, but there's the resistance in the picture, then, because of something that will not be long term, okay? Does that make sense? And you type, you know, pregnancy with diabetes as well, gestational diabetes, those are all instances of insulin resistance that they can be managed. And once those hormonal shifts are out of the picture, the resistance typically isn't as excessive or and, or just goes away, right? It
Scott Benner 06:19 could be language with type ones too, because, like you said, insulin resistance is a very specific thing, but you could be at times resistant to insulin. That's the feeling right, like it doesn't matter how much insulin I give myself, it's not moving. I'm resistant to the insulin. I'm insulin resistance. And then those two things just get blended right together, correct? That's just Yeah. And now it all means the same thing, but it doesn't mean the same thing. Does not again, weight gain, sedentary lifestyle, hormonal changes, medications, illness or stress, lack of sleep. These are all reasons why you might find yourself requiring more insulin than you normally do, right? Doesn't necessarily mean well, the weight gain does, though, right now weight gain is that would be insulin resistance.
Jennifer Smith, CDE 07:04 It would be especially if it's weight gain that goes well outside of a growth parameter, or expected growth, right? Kids, teenagers, we expect them to grow, and usually growth happens in weight and then height, and then weight and then height, right? It doesn't typically all happen at the same time, give or take the kid, right? But we wouldn't expect a child to grow really, really slow or not much in height, but continue to pack on the pounds. That's not what we would want to be happening. That's not normal growth. And so then if other parameters are in the picture, especially, you know, more sedentary lifestyle. I there is, you know, one of the potential risk factors when we talk about type one with insulin resistance is a family history of type two. So there's the potential, then, that the body is more from a genetic predisposition to have the potential for problems with weight management and whatever. And again, there are people that would beg to differ with that, but there's enough research out there. I've
Scott Benner 08:07 had a doctor on from Joslyn. He's also on staff at Harvard, and he said that, you know, the term double diabetes is just, you know, going to take on more and more prevalence, maybe in the zeitgeist coming up, probably because of how glps are working. For some people with type one, which then, you know, you ever see somebody with type one, go, I tried a GLP. It didn't do anything for me. And I thought, oh, yeah, you don't have any insulin resistance, you know what I mean?
Jennifer Smith, CDE 08:33 And or the other factors that the GLP ones, I mean, they're, they've been used for a long time. The newer versions now are definitely like the steroid version of what we had years ago that really didn't do what the new ones are doing.
Scott Benner 08:46 Glps on steroids, right? I mean that inflammation, weight loss, it tamps down hormonal issues for some people, also just constantly high blood glucose, just chronic hyperglycemia, can increase your insulin sensitivity. You've probably heard me talk about us Med and how simple it is to reorder with us med using their email system. But did you know that if you don't see the email and you're set up for this, you have to set it up. They don't just randomly call you, but I'm set up to be called if I don't respond to the email, because I don't trust myself 100% so one time I didn't respond to the email, and the phone rings the house. It's like, ring. You know how it works. And I picked it up. I was like, hello, and it was just the recording was like, us. Med doesn't actually sound like that, but you know what I'm saying. It said, Hey, you're I don't remember exactly what it says, but it's basically like, Hey, your order's ready. You want us to send it? Push this button if you want us to send it, or if you'd like to wait, I think it lets you put it off, like a couple of weeks, or push this button for that, that's pretty much it. I push the button to send it, and a few days later, box right at my door. That's it. Us, med.com/juice, box, or call 888-721-1514, get your free benefits check now and get. Started with us, med, Dexcom, Omnipod, tandem freestyle, they've got all your favorites, even that new eyelet pump. Check them out now at us, med.com/juice, box, or by calling 888-721-1514, there are links in the show notes of your podcast player and links at Juicebox podcast.com to us Med and to all the sponsors. Today's episode is sponsored by Medtronic diabetes, who is making life with diabetes easier with the mini med 780 G system. The mini med 780 G automated insulin delivery system anticipates, adjusts and corrects every five minutes. Real world results show people achieving up to 80% time and range with recommended settings, without increasing lows. But of course, Individual results may vary. The 780 G works around the clock, so you can focus on what matters. Have you heard about Medtronic extended infusion set? It's the first and only infusion set labeled for up to a seven day wear. This feature is repeatedly asked for, and Medtronic has delivered. 97% of people using the 780 G reported that they could manage their diabetes without major disruptions of sleep. They felt more free to eat what they wanted, and they felt less stress with fewer alarms and alerts you can't beat that. Learn more about how you can spend less time and effort managing your diabetes by visiting Medtronic diabetes.com/juicebox
Jennifer Smith, CDE 11:31 it can actually, yeah, it can increase high blood sugars. Can increase your insulin needs, not your sensitivity, but yeah, exactly, it can
Scott Benner 11:39 give you increased insulin resistance, is what I meant,
Jennifer Smith, CDE 11:41 right? Absolutely. And what, what does that boil down to? It boils down to an inflammatory, you know, nature. I mean, we've talked before when we've talked about the different things that high blood sugars do in the body, right? And it is. It's kind of like, I think you've said, like a sand blaster to the outside of a painted building, right? The more sugar you have circulating, the more damage it creates inside your vessels and your tissues, thus all of the complications that we know about and have been told about, but if we leave that high, it's just chronic inflammation, and that's really hard for the body to get over. I think it's interesting that the doctor you talked to actually commented on what we kind of call now we're really aiming for the ability to have a dual diagnosis. And there is now in the ADAs, I think I brought this up before too, like an 88 standard changeover, the 2025 standards of care in diabetes does have a specific kind of statement within their document that notes that although type one is the diagnosis, some people with type mate one may have features that are associated with type two, things like insulin resistance, the obesity factor, metabolic abnormalities, inclusive of things like PCOS and all of those, and in terms of managing their life the best that we can, we're going to need to create a category for those people who have features of both type one and type two, almost a new diagnostic code or a new not just type one or type two or Lata or type 3c, or, You know, any of those things, but it translates then into the ability to access medications that can be an advantage. And as of yet, we still don't have any. We don't really have anything that's type one outside of insulin. And maybe, you know,
Scott Benner 13:36 my daughter's endocrinologist gave her a double diagnosis, and it was accepted by our insurance the first time. She didn't have to argue about it.
Jennifer Smith, CDE 13:44 And there are some specific parameters, like, if you're looking at that dual diagnosis, because you've gone through it with your doctor, it's not just your, you know, Google searching, or whatever it's you've gone through it with your doctor, and you've got at least, I think it, think it requires at least three specific areas to be check off points of determining insulin resistance. It it's based on how many units of insulin per kilogram of body weight you're using in a total daily amount of insulin. If it's over that amount, check box, right? Obesity is another indicator, right? So if you're looking at BMI from that indication, the threshold for the GLP ones is at least a BMI of 27 and above, right? So if you've got those factors, blood pressure that's elevated more than 130 over 80, I think it's a HDL that's low, especially for for men and for women, you've got high triglycerides higher than 150 all of these are their check offs to proving that there's a metabolic condition or a metabolic piece despite the initial diagnosis of type one, that dual diagnosis can be really beneficial.
Scott Benner 14:55 I know for sure, after talking to Dr Hamdy, I'm gonna have to be digging more into what a cytokine is, because. Because he kept bringing it up a lot. He also talked about a oral GLP medication that's in the pipeline that will not only help you with weight loss, but minimize muscle loss. So very he was very excited about that, I will say, he seemed very sure that injectable glps are a flash in the pan, and that the oral ones will be the way it happens much sooner than you expect. So I have my fingers crossed for that. I wonder,
Jennifer Smith, CDE 15:27 did he comment anything about the reasoning? I know a lot of people have asked for a long time about, why can't we just take an insulin pill? Right? And it has relevance to what the digestive system does to that it just breaks it down, and it digests it, and you really get nothing out of it. Then, right? So either it's an injectable or it's an inhalable and then the body doesn't break it down too quickly, and you get nothing out of it, right? He
Scott Benner 15:53 didn't mention how it's getting accomplished at this point, but if people are interested, it's episode 1411 it's called GLP essentials, with Dr Hamdy is very thoughtful on the subject. I'll have to listen to that too. Yeah, very involved for a long time. Hey, I just want to say that if you have type one and you're not experiencing what seems like actual insulin resistance, some reasons might be genetics. You may have, like Jenny said, not be in one of those hormonal impact signs. You could be younger because, for reasons, you know, younger people don't experience it always as as frequently as older people, and you might just be more active, like, you know, we talk about that all the time the Pro Tip series and other places. Why do people struggle with a ID systems? Sometimes, because I'm super active on the weekend, but not during the week or vice versa. And you're like, oh, this thing can't keep up with me. But the truth is, is that your lifestyle is greatly impacting your insulin needs, correct? Yeah. So that's another way to think about it,
Jennifer Smith, CDE 16:50 and therein lies a you then don't really, you're not really classifying that as insulin resistance. That's a lifestyle impact or unlike chronic inflammation, which can also come from other health conditions, they could be impacting your body's ability to use insulin the right way or efficiently. And so then inflammation is more of a long duration, and you are likely to then have true insulin resistance, whereas high blood sugar is from a really stressful job. I have so many you know now working with a lot of women who are kind of moving past menopause, moving into sort of retirement stages, right? What we see is really high stress, high energy jobs. They retire, and come January, they're like, I don't know, I'm low all the time, like, well, let's take a look.
Scott Benner 17:41 I would curse right now and tell you that Arden's been off of school for a number of weeks. Might be six, eight weeks, she takes a GLP medication that helps with her insulin. You know, resistance, because she probably has PCOS. And you know, her settings are much lower right now than they were back in college. And today, she went back for just a day, like, to go back for a day to do this thing. And since she woke up, and now three hours later, her blood sugar is 175 like the algorithm, can't it. Can't get her down, like, because now our settings are for Arden at home, not stressed out. Arden, not Arden's at school, thinking about all the things she has to do art. And knowing
Jennifer Smith, CDE 18:21 the algorithm you're using, I know that it takes a little bit of adapting to actually, yeah, nudge it back, yeah.
Scott Benner 18:27 It'll keep up a little bit eventually. But the truth is, is that the person she was on her graph yesterday and for eight weeks prior to that is not the person she is today. So, and I'm telling you, that's exactly what it's from anxiety life, you know, foot on the floor, that doesn't go away. Basically,
Jennifer Smith, CDE 18:45 kind of going back to the doctor's comments about the cytokines you're like, I have to look that up. There's a lot of really good cellular investigation as to insulin resistance and what's not happening right in the body, and what are some of the lifestyle things that we can get to beyond adding extra medications that could, you know, again, help. So I don't
Scott Benner 19:15 want to get into it now, because we'll get off track. But he had an interesting take that I'll share with you privately, and people can go check on it, the livers role in insulin resistance. So how could the liver be impacting people? Yeah, I mean,
Jennifer Smith, CDE 19:31 you know, your liver is a really interesting organ, right? What the liver does a lot of things. It's a detoxifier. It helps with management, not only of blood sugar, but a lot of other systems in the body. And so if your body isn't using insulin the right way, there's a disconnect to the liver. For you know, ease of explanation, there's a disconnect to the liver, then about what it's supposed to do for. You and it gets off balance. That's the best way to really, you know, simplify it overall.
Scott Benner 20:04 So I have a little bit of language here. I want to know how you feel about this. Under normal circumstances, insulin suppresses the liver release of glucose. When there's insulin resistance, the liver doesn't always receive the stop message, effectively Correct. That's what I said. It gets what you said, Okay? Because I was like, Oh God, I'm not sure if I'm understanding, nope. So I just wanted to make sure. Okay, awesome. Moving on. Because these are also, I should point out, these are questions that were sent in by listeners specifically about insulin resistance. Oh,
Jennifer Smith, CDE 20:33 awesome. Well, they were very well thought questions, honestly, very well worded and well put together. If you really wanted to get into the science of the liver and all the things we could use big, fancy words, you know that talk all about glucose uptake and fatty acid oxidation and like all of these. But right? People are gonna be like, I don't know what that word means. Like, what does that have? I don't understand. Just tell me why my liver isn't doing the right thing,
Scott Benner 21:00 doing the right thing. How does insulin resistance impact long term diabetes management beyond just needing more insulin? Are there complications that are associated with it? That was the question that we got from a person. What do you think? I think
Jennifer Smith, CDE 21:15 the deeper question is, with insulin resistance, it creates a problem with overall glucose management, that's the bottom line. And so really the question there is, if I don't get on top of the resistance, meaning really, I'm not managing my blood sugars because I'm not able to get my insulin to work, well, down the road, you have all of those long term complications that we're really trying to prevent, right? And the biggest ones really being heart conditions and those micro vascular things like in your eyes and the nerve cells and all of those things are relative to the bottom line being your blood sugar management. But if you're doing the best that you can, and you're using a lot of insulin, it's not quite controlling everything yet, then the real issues with resistance are the downline of what does that mean with blood sugar?
Scott Benner 22:12 It's funny, as I thought about this one, what popped into my head was a well maintained classic car. It's gonna sound strange for a second. But I have a friend who drove a Camaro, you know, built in the 60s. Not just beautiful car, but like original three speed transmission, 326 motor. It was convertible, had the headlights that uncovered and like the covers, came off and slid into the car, all run by air. And 4050, years later, the car looked brand new and worked brand new, and it made me think about people who say, I'm fine. Like, look at me. I have type one diabetes. But, like, I know you're saying my a 1c should be this, or my variability should be more like this, or maybe I should eat like this or that, but I'm okay. And to them, I would say that in 1965 that car looked brand new, and the reason it still looks brand new is because of the meticulous way he took care of all the little parts and features of it that you don't recognize are even happening day to day. Like, yeah, I know this is an old timey idea, but there's a big piece of plastic that like, flipped out and slid into the car, all off of air pressure that still worked. 50 years later, you have little functions inside of your body like that, and they're just really important to keep up. And so if you're wondering why, sometimes you buy a car, and 15 years later, it's garbage and you basically throw it away, it's because you ignored some of the little things that day to day seemed like they were okay, but could have used a little tender, loving care. So
Jennifer Smith, CDE 23:40 you made me think of my dad. He and honestly, I It's like you were talking about him truly, because he had a 68 Camaro. Oh, no kidding, dad. I should say it's actually my brothers now. I mean, my dad's been passed away for a number of years already, but he willed it to my brother, so my brother now is the one who maintains it. And you're right. I mean, my dad, if anything I learned from him beyond just exercise, it was you take meticulous care of the things that you really want to last. That was his bottom line. I mean, he waxed our bicycles. Scott, so it sounds like the same guy you're talking about, like all the care that you give, but you have to think about yourself. It's like the advice that's often given to parents. If you have a child you're taking care of you have to take care of yourself too, or you're not going to be there to take care of those who need you, right?
Scott Benner 24:31 My friend eventually sold his car. Oh, that he bought from the first owner, which was an old lady who literally, just like the story goes, like, put it in the paper. And he got there, and she's like, I can't handle this thing anymore. And he bought it for $2,000 and sold it many decades later for $60,000 and I think if you want to still be valuable many decades from now, you gotta polish the chrome a little bit. You know what I mean. And that's not a euphemism. Yeah. But no, not
Jennifer Smith, CDE 25:00 at all. If you want yourselves to be as healthy and lovely and at 90, you want to grocery shop and carry your bags in the house and all of the things there's maintenance to your body, you have to do, right?
Scott Benner 25:11 Yeah. I mean, it's the difference between whether you go to the junkyard at the end or you gracefully, you know, drift off. Here's another question for people, many type one struggle with unexplained high blood sugars despite pre bolusing and adjusting insulin. How can someone tell if this is insulin resistance playing a role? I think this gets into management. I think this is more about settings, right?
Jennifer Smith, CDE 25:34 I do and because I think the question just begs more discussion, really, it does, because it's not defining all the time. I sit high. No matter how much insulin I dump in, I sit high. It's specifically around meals and going high. And so with the idea that this person feels like their Pre Bolus has been worked on, and that that's potentially not the issue, then maybe there are there some some other components within the meal time and or maybe the ratio has changed, right? Maybe they've grown. Maybe they've gone through a life change of some kind, and so maybe the ratio has changed, but they haven't changed that. They've just been playing with the Pre Bolus.
Scott Benner 26:13 I tell people all the time, because people all the time say, I don't know what's going on. My Pre Bolus time is 30 minutes. I have to Pre Bolus an hour before I eat. I'm like, well, that's not a Pre Bolus issue. Like, that's something else. So I always tell them to go back to the beginning make sure the basal is okay. Yep. You know, has anything huge changed in your life about your activity? You know, the things you're eating, right? That kind of stuff, you're sleeping, etc, essentially,
Jennifer Smith, CDE 26:36 the variables, that's what you're you know, I mean, looking at at those variables. Maybe the person was used to walking their dog three miles in the morning before they actually got to breakfast, and that was a benefit, and now all of a sudden, they're not doing that. Or you know what I mean? So absolutely. So
Scott Benner 26:54 I'm going to read now five questions in a row that are all part of a bigger conversation. Okay, there seems to be two schools of thought, one focusing on low fat, high carb diets, like the mastering diabetes diet, and another one, low carb approach. What does the research say about the best dietary approaches to improve insulin sensitivity in type ones? The next question is, are there specific foods or micronutrient ratios that have been shown to improve insulin sensitivity. The next one is for someone who's insulin resistant. Should they be focusing on cutting carbs, reducing fats, or prioritizing protein? And there are mixed opinions on intermittent fasting. Can fasting improve insulin sensitivity type one diabetes, or does it pose a risk? I'm going to throw in this one as well. Some people say that processed foods contribute to insulin resistance, what specifically in processed foods makes them problematic for blood sugar control. So we'll go through them one at a time, but I think they're all part of this conversation. They are,
Jennifer Smith, CDE 27:54 and I think we'll, we'll kind of mush them together, even though trying to kind of go through them separately, it's probably going to answer
Scott Benner 28:02 a lap, yeah, they're gonna go for a lap, yeah, yeah. The first one is the tough one, because, you know, people who are very strictly low carb, that have a lot of success with it are just going to tell you, you know, love, like, what do they say? Low numbers, right? You know, little bit of
Jennifer Smith, CDE 28:18 car, the rule of the rule of small numbers, right? A little bit of carb, a tiny amount of insulin, you've got an easier, kind of a little easier control mechanism, because there's not as much overage there from an insulin, but you also don't have a heavy hitting macro nutrient being carbohydrate that you're really trying to step on top of and keep managed. Right? The big thing behind this main question of the two schools of thought from a dietary standpoint, or like my background, it really boils down to looking at what each of these fueling plans provides. Has science that does suggest it can work. They both do the vegan, low fat diet, plant based absolutely has research that suggests you can reduce insulin resistance, you can bring your medications down, you can help to control the heart issues, even things like PCOS end up being better managed and navigated. Weight loss is something that happens in the picture. Those are 100% the same thing that the low carb approach also is able to prove that they can achieve, you know. But the bottom line is, you decide on it, and you don't falter from the plan. That is it in a bottom line picture. If you're going to do something like all plant based, low fat, then do it. Figure out. But you have to stick with it. It doesn't mean every week you will go out for your 16 ounce steak, because you can't 100% give that up. This is a plan, right? You choose it, you follow it, and 100% Your metabolic things, they clear up. They do the cholesterol levels, the blood pressure issues, again, even the metabolic things, the way that your body cells use food, they are changed. Yeah,
Scott Benner 30:12 I think it's, it's such an important thing to say, because I think that's probably where people go wrong. They're like, they dive in, like, you know, I'll eat super low carb. But then on Saturday, you have a slice of pizza with a bag of Cheetos, and forget, right? Two steps forward, one step back. It was probably two steps forward, 10 steps back, right? It's about whether or not you can really commit to it. You think I
Jennifer Smith, CDE 30:33 really do? Because there is when I look at the data, and people ask me the questions all the time, well, should I should I go this way? Should I go that way? I have to say. But what? What do you know about both of those plans? They're almost like opposite ends of the spectrum. Yeah, which one are you most likely to be able to stick with long term? Because if you can, here are the 10 different research articles I can give you. They're not even based in, like, the big ones that a lot of people have problems, like believing in, right? These are really good, defined references that suggest it can work. And we've got communities that are centered on both of them with discussion about why they work, and all the people that that they definitely help. Right?
Scott Benner 31:19 Is there any scenario where following any of these ideas strictly won't work for somebody? Is there somebody who's just genetically it doesn't work for is that not a thing? Because it's part of the little questions? Question, yeah, like, I mean, is there someone out there just eating low carb exactly the right way? And they're like, how come this isn't working for me or vice because I've heard it for the more the vegetable, like fat one. I've heard people say I've done it specifically well, and it hasn't worked for me, but I'm watching other people do it, and there's got to be something there that's, I'm
Jennifer Smith, CDE 31:49 sure that there is. And so that also suggests that maybe either you're not following it to a T so really, get the reference materials. Get the books. I mean, there's, there are books on, you know, the mastering diabetes and also on the low carb end of every their books that definitely give you very well defined this is your plan of action. Yeah, you haven't quite done and you've really only been following with some online person who tells you what they're doing. Maybe there's a little piece in there that's not quite what your body is working with. The best way
Scott Benner 32:19 that takes me to the micronutrient idea. Like, how would an average person who's like, I'm going to make sure I'm giving my body exactly what my body needs? Like, how do they figure that out and put that into play? Yeah? I mean,
Jennifer Smith, CDE 32:30 it also goes into lifestyle, right? If you are somebody who has a really excessive amount of movement in your life compared to somebody who is more sedentary, we would look at what is your overall need to be able to break down macronutrients. And then the lovely thing about the macronutrients is that if you are getting a fair variety of foods, you're going to take in all the micronutrients that you need, both the fat soluble and the water soluble vitamins, the antioxidants, all those things that help on a cellular level, change things like inflammation. It's not as simple as people often think, cleaning up the diet, yeah, just
Scott Benner 33:11 pouring in the right stuff, yeah. I mean,
Jennifer Smith, CDE 33:13 it really does behoove people to sit down with somebody knowledgeable, and I'm not going to say that, you know, find the right person right away. It might take, just like looking for the right endocrinologist. It might take a little bit of navigating through some people to find somebody who kind of fits with you and that you can work really well with, but they should be evaluating your life, what type of stressors you have, what kind of energy level or exercise plan do you have, and then building into that well to meet your need as well as address this insulin resistance and overall help with insulin sensitivity. Let's play with adding this, taking this away, cutting back here, adding this in. You know, somebody who is an endurance athlete is going to have a different macronutrient need profile than somebody who is in the lifting gym three hours every single day and they're bench pressing. I don't know a large amount of weight that I can't even probably live. Does that make sense, though it
Scott Benner 34:19 does. I want to go to intermittent fasting and then go back to processed foods. So the intermittent fasting, what I have here says that, you know, for some people, it might improve insulin sensitivity, but then it warns against hypoglycemia. But what I would say is, from my own personal experience with Arden, is Arden can fast almost for freaking ever, but she's also on an algorithm that's taking away your insulin at times. So if you're using, like, jacked up, heavy settings, and then all of a sudden, like, I'm gonna start intermittent fasting. I mean, you're probably gonna get low. But if your settings are there, and your system can bob and weave with the fact that there's nothing in there, I've seen art at night eat for 1824, hours. To not get low, like, as a matter of fact, like, I would tell you, if you can get all that straight, and you're a person who's like, oh, I can't exercise without getting low. Wake up in the morning, don't eat with great settings and single move workout in the morning. Yeah, so
Jennifer Smith, CDE 35:13 no, it's a, I think it's a quality question. Whoever asked about intermittent fasting, the risks, as you just said, can be minimized, especially with the type of technology that we have today. At it at our disposal, right? Not everybody, but a lot of, a lot of people have access to at least a CGM, great, right? If you have access to an A I D pump system, fantastic. That moves you up the mark to avoid risks if you're trying to do some fasting, but even those who do multiple daily injections, you can strategize your insulin and your dosing in order to be able to do intermittent fasting. And there are, you know, by definition, there are a lot of different kind of ways you can intermittently fast. Some people do fasting two days in a row, then they eat for two days and they fast for two days, right? Then there are people who do what's more common, and I think in terms of navigating the real metabolic reason, which I would encourage people to really look up, because it's quite fascinating the cellular level and the reasoning behind intermittent fasting and how it really benefits insulin sensitivity and weight management and everything. Is the idea of time periods of the day where you will designate, this is my eating time, yeah, and then time periods of the day where you will be done eating, let's say by 7pm and then you don't eat again until 10am the next day, right? Or noon the next day, and there are a lot, especially from a women's health perspective, there are a lot of good referenced research in what that does from a hormonal level in women's health. Not enough of it. I think that goes into real type one diabetes. But if you can read into the research, you can understand how it could impact your diabetes management, because most women complain about the fluctuations around their monthly cycle or moving into perimenopause or even menopause, right? And if we can harness that energy burning piece of our cells in the right way, and also clean up our intake with the food that we are eating. It makes an enormous difference on our overall ability to use insulin the way that we're supposed to. I'm going
Scott Benner 37:33 to jump to this last piece here, processed foods. You know, can processed foods really blah, blah, blah, like, I think, I think in the information age, we're very used to people saying things, and we just accept them, right? We don't really dig deeper into them. And so some people can also hear that in just this recording, like, oh, processed foods are bad for you. Like, ah, I've been eating it all my life. I'm fine. Like, it's great. Yeah, you're because your car is not 50 years old. Yeah, your body's still able to make it through a ho ho without you dying. But one day, you'll put the wrong gas in and it's just gonna shut off. But I'm gonna keep a lot of this for the nutrition series that you and I are gonna do, because I think we should do an entire episode on why exactly processed foods are doing what they're doing to you.
Jennifer Smith, CDE 38:14 Yes, it's on my list, and I have not organized for us yet, sorry. Give
Scott Benner 38:19 me a high level overview of processed foods and how they can, you know, make insulin resistance their car make it worse.
Jennifer Smith, CDE 38:26 Yeah, and actually, it ties into that first question in this little kind of segment that we're talking about is the focusing on either the really low fat high carb intake or the more low carb or ketogenic type of plan. One thing that's missing from both of those plans, for the most part, if you're doing the plans the right way, you are eating food that looks like food, what has that done then, behind the scenes, whether you're low carb, high carb, whatever you've cleaned out. I mean, the question here, what specifically in processed foods makes them problematic. Have you ever read the back of most of the packaged things that you buy? I mean, outside of maybe you bribe brown rice. It's brown rice, right? There's nothing problematic in that unless you're low carb, then you won't eat it. When you look at the back of many packaged items, they are full of things that I guarantee you can't pronounce, nor do you know where they came from. Why are they in there? Outside of things that have parentheses after them, since this anti caking agent or you're like, great, but why does it have to be in my food? Then, yes,
Scott Benner 39:35 it went your mouth and came out your butt. But it does. You don't know what it was doing. What was in there. Maybe you could swallow stuck. You could swallow a nickel and it can come back out again. It doesn't mean you want it there. I'm just high level, rapid breakdown of refined carbohydrates, added sugars and metabolic overload, inflammation, oxidative stress, unhealthy fats interfering with insulin signaling, nutrient deficiencies and lack of fiber, chronic overeating and weight gain. Because of calorie density and hormonal dysregulation, on and on and on. Like, yes, processed foods are bad for you, but we'll dig in later about why. And yes, they can listen, if you just ate food that you, like, Jenny just said, like, you lift it up and go, this is broccoli. I see chicken like, you know, and yeah, then eat it right. Don't take the chicken and dump some sauce on it that you bought from somewhere and go look. It's orange chicken now. Now it's chicken with nickels all over it. Think of it that way.
Jennifer Smith, CDE 40:29 It's a good brain, like you're eating
Scott Benner 40:32 aluminum foil or whatever. Like, maybe it'll make it out. Maybe it won't. Right? Can we jump to how are you on time? You good? I have about five minutes. Okay, let's go to medication, supplements, options. What can people take? Type one to help with insulin resistance, if they've changed their diet, if they change their exercise, and it's just not working,
Jennifer Smith, CDE 40:54 sure? I mean, there are prescription meds, and again, early on, I talked about how you can potentially get that dual diagnosis to improve the ability to get these covered with really good, well written letters from your doctor, things like the GLP ones. GLP one gi P is things even like old school Metformin is another potential one that you do not need a prescription for, and I can definitely say is visibly beneficial, not to the impact of things like a GLP one, but definitely beneficial in the here and now, because it gets used up pretty quick, is the Berberine that is definitely one that is beneficial. It helps attack kind of around that meal, but not necessarily long term, okay, right? Thank
Scott Benner 41:38 you for doing this with me. That's a great topic. Now it's awesome. I'm going to send all the information over to you, and we'll you know, so we have everything for next time. But before we go, how does hydration impact insulin sensitivity?
Jennifer Smith, CDE 41:52 That's a really simple one, right? Because if you are not well hydrated, all the things that are circulating in your system that are supposed to get to the cells to allow them to work the right way, one of them being hydration. If you are dehydrated, it's like moving mud or molasses through your system instead of like water out of a faucet, right? It's supposed to fluidly flow at your cells are supposed to have access float around in your body, kind of like, you know, really low leveling biology explanation. But hydration is huge, and hydration, along with which, I think often gets missed, people say, okay, they told me to drink more water. I'm drinking more water. I'm drinking like, two gallons of water a day, great, but now you're probably flushing out a lot of good electrolytes. So there is a fine balance, I say, you know, easy, simple electrolytes on a day to day basis with your water intake, are also very valuable from a balance of things in your body, you know, and the eight cups a day, give or take the person, it's probably more. If you're an athlete, it's probably more. If you're sitting in sauna for three hours a day, right? Based on size person athletics, you can kind of go up and down from there, but if you're going to try a baseline, great, stick with the eight.
Scott Benner 43:13 And what about anybody who's going to say, I'm incredibly well hydrated. I had two liters of Diet Coke today, same thing as two liters. No, okay, not at all. No, not, not at all. There is drink juice boxes all day. No, no,
Jennifer Smith, CDE 43:28 not. Hydration. Okay, are you sure? Let's look at let's look at water. Water is hydrating. There's nothing wrong with it. Just
Scott Benner 43:38 drink some water. Okay, what if I take water and I put something in it back in the day when I was a kid, but Crystal Light, I don't even that exists anymore. Now I put Crystal Light in it. Am I still drinking water? Or am I am I negating the benefits you're still
Jennifer Smith, CDE 43:50 definitely drinking water? Again, that goes back to processed foods, and what is in the thing that you're adding to your water to make it taste like you want to be able to actually drink the two gallons of water a day,
Scott Benner 44:02 Crystal Light Water with three nickels, yes, at least you're getting water. Hopefully they won't grab onto an artery on their way through, or whatever. I know arteries are not in your digestive system. I'm just saying no. Okay. What are your thoughts on supplements like Berberine, Metformin or a GLP like ozempic or Manjaro for addressing insulin resistance in type ones. That's a question right from a listener.
Jennifer Smith, CDE 44:24 No, I think it's great. I also think it needs to be differentiated, right? Because a supplement is something that isn't technically regulated, at least not most of the time, versus a medication that has approval, is on the market, is available through prescription. Like, you can't get it otherwise, right? So when you talk about things like Metformin or the GLP ones, GLP one Gi, P, the Metformin is a little bit different, but all of those are prescription you talk about Berberine or some of the other ones. Like, I mean, there are a whole list. Of things that help, from the standpoint of even optimizing your own GLP one system output, right? Your gut output which isn't working, which is why the GLP one meds do work in people with diabetes. So there are a whole host of those. I once
Scott Benner 45:16 got listeners to send me all the supplements that they take. And I thought just like, tell every like, let them just tell me everything that they take, and I'll weed through it. Maybe I'll find some like thing, and I can't figure out a way to be certain about any of it. And so like, you know, it's hard to just jump on here and start saying, like, you should try this or that, or this lady said this helped her. And part of me wants to put it out there so people can decide for themselves. And part of me is like, God, stuff could be expensive and maybe not do anything. And, you know, and many
Jennifer Smith, CDE 45:44 of them are, many of the supplements are, but you also with anything, I think, even with the prescription meds, you should be doing a little bit of your own research. Yeah, you should be doing information searching, because many of the supplements do have good research backing to them, but the information is important to look at, what was the population that was tested most often for some of the supplements we're looking at tests being done mostly in type two diabetes. Does that mean it's not relevant to type one? Not at all, but they're really only doing most of this stuff in type two, and then what's the concentration that's being used? What's the healthy concentration to use that you can get on the market? You already said, what's the cost of using that? What impact should I see? And a lot of people, I think, with supplements, to go down that kind of road, first is you end up getting a list of six things. And you think, Well, great. All of these are supposed to be wonderful for my weight and for my blood sugar and for my my gut health. I'm just going to throw them all together and see what works. Well, if it does, fantastic. But some of them may not be doing much at all, purple, right?
Scott Benner 46:59 Five at once, if they all so then I think the problem becomes then, because I've gone through this myself or with people in my family, you say to somebody like, look, we're just going to take one of these a day for three months and like, and people are just like, What are you kidding me? And if you don't see a pretty instantaneous like, change or value, it's hard to remember to even do it. It's hard to Shell out the money. And then people tell you what's got to be a quality, you know. And then you look and quality means $40 for a jug of them, and you're like, oh, you know. And so I don't know how to talk about, I wish there was, like, an easier way now what I can tell you about, what I've learned about glps Over the last couple of years, taking them for myself, using them for my daughter with type one. Listen, I'm not obviously a doctor or researcher anything like that, but I know a few things to be true after the last couple of years, if you're using a GLP medication, as Dr Hamdy said in Episode 1411 and you are not doing muscle training and taking in enough protein, he says you should not even be using them. It's just too dangerous to lose muscle, especially as you get older, and it's just something you don't get back. So you have to maintain and build muscle while you're using a GLP. It's very important. The other thing I've learned is some type ones are like, Oh my god, I jumped on a GLP and it changed my life. Like, I use significantly less insulin. I like, you know, my spikes are lower. Like, oh, all these good things are coming. Then another type one will say, I tried it, and honestly, I tolerated it well, but nothing happened to my insulin needs. And I guess I've come to believe that some people can have, you know, what I've heard called, like, double diabetes, like they have type one diabetes, but they also have insulin resistance. Correct the dual diagnosis, yeah, without type one, they'd still have insulin resistance. And I don't know if I'm right about that or not, but just watching people, it's the only like explanation I can come up with why some type ones would take it and have such a reduction in someone, and some type ones don't have any So, right? Yeah. I
Jennifer Smith, CDE 48:56 mean, this actually gets into, I think, another, another question somebody had asked within the same line of questions, it's about like lab values and testing for insulin resistance. So again, if you're looking at supplementation or pharmaceutical type of prescription, it would behoove you to know is what I'm seeing growth in my teenager and they just need more insulin? Or is this truly insulin resistance? Because there are some markers that you could look at that could move you to a diagnosis and again, now with ADA standards, suggesting that people with type one could have these other pieces that are more type two, and so you could have a dual diagnosis, making it quote, unquote easier to potentially get the prescription option
Scott Benner 49:48 right, right. I'll mention too in that episode that Dr Hamdy, who is, I think, on the the arrows tip on this stuff, says that he thinks double diagnoses will be actually common. And acceptable very soon. So I it sounds like behind the scenes, the people who push for this stuff are pushing for that.
Jennifer Smith, CDE 50:06 And it sounds correct, given all of the information that we have and some of the newer, like real research that we are looking at coming from use in type one specifically. And hopefully that's a turnaround for prescribing and not having to sit to get six letters of approval from your doctor stating this, this and this are the issues. Why won't you approve this? But
Scott Benner 50:31 if you saw a type one like you see type ones who use glps, right?
Jennifer Smith, CDE 50:36 100% yes, not 100% of them. But yes,
Scott Benner 50:39 absolutely so. If people are interested in learning more, they should talk to doctors. And if you can't, I'll tell you this, if you can find a doctor great that understands it, but if you find one that doesn't seem to understand it at all, like look around a little more, because they're just going to throw their hands up and go, I don't think you should do that, which I think is code for, I don't know what I'm talking about, and I don't want to get involved. So right, yeah. Speaking, yeah. Many people say that losing weight improves insulin resistance. Is this true even in a person with type one diabetes is not overweight, even if the person is not overweight. So if we have a person with type one who doesn't I don't know score as overweight, could losing some weight help their insulin resistance? It could. I want to say that I think there are a number of things happening. I'm going to go back to glps for a second, even though we're not talking about them when they first came out. And I had a bunch of conversations with a bunch of different doctors, they would all just harp on the idea that people are using less insulin because they've lost body weight. And they would just keep saying that, keep saying that. And I mean, after having enough conversations, even like with Arden who did not have like, you would never have looked at Arden and thought like, Oh, that girl should lose weight, but she did lose weight, and that's part of why her insulin needs went down. I believe they just are
Jennifer Smith, CDE 51:52 besides the true effect outside of weight loss, the true effect of GLP ones is it goes beyond just loss, and that's the reason that somebody who doesn't have a weight based issue but has high insulin needs, if something else hasn't been identified, such as a normal weight person, lifestyle doesn't suggest that they should be using as much insulin as they actually are. It's very difficult for them to control their blood sugars in the after meal time period, then we're looking for things like PCOS. Is there an undiagnosed thyroid disorder in the picture? Right? I mean, there are, there are pieces that I see over and over. They stand out to me. As soon as I talk to somebody, I'm like, have you had this checked? Did somebody ask you about this? Did you get No, nobody's what is that? Nobody's ever mentioned that. I'm like, let's get these checked first. So
Scott Benner 52:42 if you lost a lot of body fat and your insulin resistance didn't change, then look for other impactors. But in a lot of cases, losing that body fat should change your insulin resistance. It should. What about other body composition ideas like, what about adding muscle? Would that help? It should. Is that because you added muscle, or because adding muscle reduced fat? Well,
Jennifer Smith, CDE 53:04 you can add muscle and still retain fat, right? I mean, fat is stored energy, right? I mean, we have a lot of stored energy in our body.
Scott Benner 53:11 So if I'm like one of those guys that, like lifts tires and throws them over walls, like, for example, I was just that size, but not that strong, had insulin resistance, and added that muscle, I could see a reduced impact.
Jennifer Smith, CDE 53:23 You could see exactly because, again, muscle is it's harder for your body to keep healthy to maintain. So the more muscle you have on your body, the more revved up your metabolism is. And that's kind of the like the baseline explanation to that, right? But that's essentially what happens. And we know that when we move our body, even people with insulin resistance, can say, I can take a walk, and I can see the impact of that. I can move my body, and I can see that my insulin does start to work better, probably not as good as if they were a lower weight, brought their, you know, brought their body weight down, or somebody of the same height, but a leaner body type with more muscle on it, but they're still going to see impact. So if you now lose weight, add muscle, and you maintain a movement, you're definitely going to see an improved a lower amount of insulin that you need. So
Scott Benner 54:16 I'm looking at all of the questions that led us to this bigger idea, and I moved to say there's a person here asking, How much does walking after a meal impact insulin sensitivity? He's had this long conversation privately with somebody I've known for a long time who has type one, and he's in his 20s, and has recently put on a bunch of muscles, started doing like jiu jitsu and stuff like that, and and went to a little more of a lower carb lifestyle, but everything's a mess because his job is very active, right? And he's on Omnipod five, and he's like, I am getting low every day at work. Like, I'm low constantly, like, blah, blah, blah, like, on and on. And I we just kept talking and talking and talking and the the first two things I. Said to him, I ended up going, No, no, no, not that. And then eventually I said, here's what we're gonna do. And I figured out that he was getting low after meals, and that seemed to be the biggest problem, but he was so sure about his insulin to carb ratio, he said it was one to 10. And I said, Listen, let's just make it one to 20. And, like, see what happens. And I got a text the next day. I didn't go under 100 and my spike was only, like, 160 I said, Okay, make it one to 18 tomorrow. Like, keep changing that until we get there. I think that was your problem. But what he was seeing was, is that he was eating and then he was going to work and walking, walking, walking and tanking every time if he didn't walk after he ate, it wasn't nearly the same. So, right? What's the functionality there?
Jennifer Smith, CDE 55:46 Right? Any activity Walking is one of the best. In fact, years ago, during diabetes month, I can't remember what organization they used to have, something called the Big Blue Test, Manny. Would say, who was Manny? Yeah, it was Manny. It was essentially check your blood sugar. Go do 15 minutes of movement, come back and check your blood sugar. And 99.9% of the time, you're going to see movement down in your blood sugar. I don't care what body size or type you are, you're going to see why, because muscles require energy to move, and we know that exercise is, I call it free insulin, right? Your body needs the energy it's moving faster than it normally is. Your muscles are now primed. The doors on those muscles are now they're more free to open at will, and they don't need as much insulin to unlock the doors and let the glucose flow in.
Scott Benner 56:39 We know that works. You and I know that works. Is that actually impacting your insulin resistance, or is it just changing the function of the insulin that's inside of you over and
Jennifer Smith, CDE 56:49 over exercise is going to at some level, it's going to impact your resistance, right? It is okay, but in some people that exercise every day, it's basically holding you at a level. If you stop doing that, you're going to climb in insulin resistance. It's holding you out of stability. The insulin resistance is still there. And if you are the type who needs the GLP, one type, or the Metformin or something to assist further, then all you're doing is holding things where they are with your exercise. Don't stop doing it. Keep doing it. But if you're not finding you're not reaching your goals of weight loss or post meal blood sugars or as much as you really want to, then you're looking at needing to add something to help the lifestyle stuff that you're trying so hard to do. Follow
Scott Benner 57:39 up questions from people is, how does muscle mass influence insulin resistance, which I feel like we just talked about. But can lifting weights really make a difference? Yes, right,
Jennifer Smith, CDE 57:47 it can. And weight lifting is interesting. It actually many people who lift weights find no change immediately in their blood sugar. In fact, those who really go to some of the more the boxes, right, the gyms that are just all lifting, you have your workout of the day. It's very resistance based. You might actually see a rise in
Scott Benner 58:07 your blood sugar right during the lifting itself. During the
Jennifer Smith, CDE 58:10 lifting itself, right? It's an adrenaline based kind of thing, sort of like a sprint runner. You might see from the adrenaline of a sprint or hill repeats going up and down. You're going to see a rise in your blood sugar. But in the aftermath, just like weight training, you're going to see that your muscles are now recouping. And in weight training, you're building the muscle that you broke down during the workout right to build that back up, your body needs to use energy so you become more insulin sensitive in the aftermath, if you do enough weight training or resistance training, lightweight to high weight, whatever is good for your body, what kind of muscle you want, you're going to see that retained long term. Okay, that's the benefit of daily exercise.
Scott Benner 58:55 Okay, all right, let's move to like beyond diet and exercise, hormones, stress, sleep, steroids, that kind of stuff. When people see a greater insulin need because they haven't slept enough, they're under stress, the doctor gave them a steroid for an infection or they have a hormonal impact. Are they seeing an actual change in their insulin resistance?
Jennifer Smith, CDE 59:16 It's momentary. I think, yeah. I think it's momentary. I think it's more right, right now, this is what's impacting my insulin. Need hormones in females, obviously, that's more in the moment, or depending on where they are in a monthly cycle can go up and down, right? Somebody who has a big business presentation to do, they may be stressed for a couple of days while they prep for it, and they plan it, and they work with their team, and then they get to it, and as soon as it's done, if you've changed your insulin doses to accommodate and keep your blood sugar managed, you're likely to need to remember what your doses were before the stress, right? Because it should come back down. That's momentary insulin resistance, which isn't, I wouldn't even. Call it resistance. It's just the effect of a variable here and now.
Scott Benner 1:00:04 Do thyroid issues impact insulin resistance? Yes, they do. Okay, absolutely. Hyper, hypo doesn't matter. They both
Jennifer Smith, CDE 1:00:11 have impact on your overall insulin need. Yes, both to the extreme of needing a lot more, as well as a they're both a little bit opposite. We actually see in hyper that because your metabolic rate and the turnover of all different types of medications is a lot faster, you're ending up needing you're clearing that, and you're needing to use a lot more insulin, right? Whereas in hypo, you've got metabolic slowdown until it's regulated. And so you might actually find that while your weight isn't being managed well, and that you feel like you need more insulin, sometimes there is dysregulation in dosing, because you feel like you're taking more but you end up with a lot more lows because of the lagging effect of the amount of insulin that you're taking. So there is, I mean, thyroid is, it's huge to get optimized if you're having issues with your insulin.
Scott Benner 1:01:06 Okay. Do you know how sleep impacts insulin resistance, like lack of sleep? You know the function of it, or just that it does. It's
Jennifer Smith, CDE 1:01:14 just, I mean, baseline is, it's, it's a stress, right? Especially quality sleep. You might have something that tells you you're sleeping seven or eight hours a night, but we have enough watches and Rings and Things now to take care of. Looking at what was our sleep quality light, how many times did we roll over in bed? Even some of these devices measure what would be like sleep apnea, kind of dysregulation of oxygen intake during the overnight times. You might think you're sleeping, but you're really not getting quality sleep through all of the different cycles of sleep, deep sleep, REM sleep, all of those things, right? And in the end, it again, is just baseline. It's stress on the body.
Scott Benner 1:01:57 Since you mentioned stress at the end, there's these like sub questions under our headings here, how do I manage stress to improve blood sugar control? I'm going to assume that me telling you to calm down is not going to help. I mean, is it just one of those things, like, you got to figure out how to manage your stress, really? What are you going to
Jennifer Smith, CDE 1:02:12 That's right? I mean, it's like a it's like a blanket statement, because I think everybody needs something that's going to be a little bit different to manage stress. I manage stress by working out. I run. I do yoga several times a week. There are different types of yoga, some as meditative. Some is more active yoga. I use weights. So exercise is really my like stress reducer. I also like to cook. So, you know, find your thing, and if that helps you, and you have time to build it in. It might be enough to keep your stress levels at bay. Some people stress, though, is not only their own life stress, but it includes their family's stresses, right? So then you have to navigate it all. Yeah,
Scott Benner 1:02:54 I noticed a hot shower makes hardness, blood sugar go down, and I know that it's, it's like, people are like, Oh, hot or cold or this. I'm like, I honestly just think she gets in there and she chills out, she sings and she relaxes. The water hits her head, and I think she just relaxes a little bit. So, okay, identifying, let's see IR insulin resistance on lab work and early warning signs. What labs or markers should someone ask their doctor about if they suspect that they have insulin resistance, and for those who don't realize they have it, what are the early warning signs to look out for? Are there lab value? Can I get there
Jennifer Smith, CDE 1:03:32 are like somebody, and this goes the route of really talking about maybe somebody who has some of the physical identifying markers like you're overweight, you have a more sedentary lifestyle, you may not have the cleanest food intake, maybe you don't work out those kinds of things. Are there markers that someone could be looking at with not knowing that you have diabetes? There are, I mean, obviously one test would be an A, 1c right? It's going to give an overall evaluation of is your body not regulating your glucose like it should in people who don't have type one, something like an overnight fasting insulin level, can also be a method of managing your body's output, and it's a way To sometimes also identify pre diabetes, before type two diabetes, because, again, early stages of type two, your body is over producing insulin to make up for that insulin resistance that's there. So that is another piece that could be managed. Obviously, somebody with type one doesn't need a fasting insulin.
Scott Benner 1:04:38 I went to our friend online to ask this one so fasting insulin, Homa IR, homeostatic model assessment of insulin resistance, a fasting blood glucose, hemoglobin, a 1c triglycerides to HDL ratio, a ratio higher than 2.5 to one is linked to insulin resistance. Your C peptide, of course, postprandial blood glucose. Insulin, checking glucose and insulin one to two hours after a meal could let you know if you have form of glucose metabolism and liver enzymes. Elevated levels may indicate fatty liver disease, commonly associated with insulin resistance. It says uric acid. High levels correlate with insulin resistance and metabolic dysfunction. Some early warning signs could be frequent, fatigue, increased hunger and cravings, difficulty losing weight, dark patches on the skin, skin tags, high blood pressure, brain fog, PCOS, dizziness or shakiness between meals, increased waist circumference. There you go. That's from
Jennifer Smith, CDE 1:05:36 our most of what's on my list. So you you got to all of that. Jenny's
Scott Benner 1:05:40 like, am I going to get supplanted by a prompt? I hope,
Jennifer Smith, CDE 1:05:46 I think it was a valuable question, honestly, because while some of these may not necessarily be in the realm of type one looking, some of them are even things like your cholesterol levels. I mean, the LDL especially, is one that we end up looking at your triglyceride levels, the relevance of the liver enzymes. All of those, whether or not you have diabetes, can be Hallmark identifiers for yes. It's
Scott Benner 1:06:13 funny, because I just had this thing I wanted to say, and then I looked down at the next question, and the next question encompasses the thing I wanted to say. So I was like, Wow, this must be building to the right place. I, honest to God, didn't know that this was about to happen. So this next bit is misconceptions, reframing frustrations, vetting information, and the questions that came in from people are, what are some common misconceptions that you hear from people with type one regarding insulin resistance? And I'm going to tell you that my question was, do you think we talk about insulin resistance correctly? Or do you think it's a catch all phrase that we use in a bunch of different places?
Jennifer Smith, CDE 1:06:47 I'm going to say that that this about insulin resistance, what we're putting together. I think it's really valuable, because I think we're defining the difference. But I do feel like it can be a catch all. It can be a place where, my goodness, this is a lot of insulin. Like I see a lot of questions often, like, my child, is this this age and uses this much insulin? How old is your child? Who's this age? How much insulin do they use? Right? And again, our insulin needs are our own insulin needs. They are how to know if it's resistance, I think we've defined quite well here. And when it's not, is it a time in life that there's a variable happening that's not resistance? It is the hit of what's happening right now? Yeah,
Scott Benner 1:07:35 I feel like there are sometimes where there's variables at play. There's sometimes where it's, you know, a steroid, or sometimes it's you just became sedentary, like your kid used to play soccer, and now they don't anymore, or you've got a job, or you're walking around all the time. Then on the weekends, you sit and watch football like whatever that thing is, no matter what, when someone needs more insulin, they're gonna say, I have insulin resistance, right? And I think the GLP conversation has shown me that some people just need more insulin. They're not necessarily insulin resistant, but at the same time, is that just a heady conversation between you and I That's meaningless to the end user who just either needs it or doesn't need it, right?
Jennifer Smith, CDE 1:08:12 Well, and I think to clarify, you need more insulin, what that says to me is without all of the other pieces that you think that you have insulin resistance. It really isn't. It boils down to have you looked at your setting, right if you're needing more around meals, but your overnight is sitting flat at 83 and you haven't really adjusted anything there, and there aren't any big pieces in the picture, and your hits are around meal times, probably not insulin resistant. You probably just need to navigate meal coverage. You
Scott Benner 1:08:43 might not be covering your carbs. Well, your ratio could be off, even if you are counting them correctly, or something like that. Yeah. In the end, I just want people to cover what they need, but I don't want them to ignore the other things that may be happening. Right? If it's as simple as taking an acetal to help with your PCOS and lowering your insulin needs. I don't want you just feeding the PCOS with a ton of insulin when this other thing could be valuable to you correct or something like that, or going for a walk or eating better, or that kind of thing, right? How does someone separate helpful advice from misinformation when it comes to insulin resistance? What do you think the misinformation is that they're getting like, maybe it's just the misunderstanding of the implications like we've been talking about. It's a vague question. It
Jennifer Smith, CDE 1:09:25 is a big question. Well, I think it boils down to you have to look at what your experiences are that's leading you to consider, is this resistance, or have I not considered what could be going on right now as a point in time adjustment that needs to be made, okay? Is it some of the things that we've already gone into? Are there lab values? Are there symptoms? Are there other things you know that you're looking at that are an issue that are leading you to consider some of the helpful advice? This is actually pointing you to think this is insulin resistance. I should get further checks or talk to somebody about this, or does none of the information that someone's bringing in fit what you're seeing? Does that right? Does that make sense?
Scott Benner 1:10:17 Yeah, yeah, it does. But I'm gonna ask another vague question though. I'm sorry, no, you ready for the last one? Yeah. Where should people start if they feel overwhelmed by trying to lower their resistance? Is there a simple first step that someone can take to put them on a path to figuring this out? Do you start with food? You start with your weight. Because you hear people talk all the time, like I can't lose weight. Type ones are going to say to you, all the time, I can't lose weight, because every time I try to exercise, my blood sugar falls and I end up eating to bring it back up again, and it feels like I'm just losing weight on one hand and eating it on the other hand. And I would tell you, if weight is your issue, then getting your your settings right so that you can work out would be step one. It wouldn't just be, hurry up and start working out, correct, you know? But also, if you don't start working out, you won't see that your needs are lesser. So it's, it's a chicken or egg thing, a little bit like, do you start working out and adjust your insulin as you go? Do you adjust your insulin? Get it really rock solid, and then start working out and keep adjusting I think maybe that's it, right? Yes, yeah, yeah. And
Jennifer Smith, CDE 1:11:24 I think in terms of resistance, let's say you've you've taken all of the advice, right, especially like from the podcast, let's say all the pro tips, you've applied them, you've tested and you've done the best that you possibly can, and with all the adjustments, you've actually found, gosh, my insulin needs are a lot higher than I actually thought they were, and it is, no matter what lifestyle piece I put into place, it is really hard to keep my blood sugar at the target that I'm aiming for. Great. Now you've got all this information to go to your physician, to your nurse practitioner, to your educator with and say, Look, I've done all this work, and I still feel like I'm using a lot of insulin to actually navigate despite all the things I'm trying to do. Yeah, great,
Scott Benner 1:12:13 Jenny, I get worried that the the actionable items all fight with each other. For example, we learned in this episode, that a sign of insulin resistance might be hunger. And then you're gonna go to your doctor, and they're gonna say, Well, if you lost some weight, your insulin resistance would get better. You should lose some weight. And you go, but I'm hungry all the time. And then they say, Don't be. And you go, but I can't not be because I got insulin like, you don't mean like, you get caught where? Like, hey, go work out. You're like, I work out. My blood sugar gets low. Everything seems to have it's like a bad cartoon, like superhero movie, like there's a bad guy for every moment that you have. And I can see how it would stop people from it gets frustrating. Yeah, right. I mean, listen, between I don't have type one diabetes, I don't have type two diabetes. I've never been I don't think I've ever been pre diabetic, but I have lost like 60 pounds on a GLP medication, and the hunger going away was a huge help. It just was like, you know, like it was such a big deal that helped me get over the hump. I will tell you,
Jennifer Smith, CDE 1:13:16 that's the biggest thing that I hear from most people who start using it, is the food fog. People call it the constant draw of I even have some people who have said, you know, I work from home. I leave my office and I have to walk through the kitchen. And since using the GLP one, I can walk through in the refrigerator or the cabinet the cupboard, I can pass it without even a thought of opening it at this point. You
Scott Benner 1:13:44 have no idea how well it works to the point where you have to remind yourself to eat. I had to remind myself to eat. Like I would get up and be like one two in the afternoon, but God, I feel lightheaded. And then I'd go over and I go, Oh, I didn't eat. I did no hunger whatsoever, like none I forgot to eat today. Easily. I could have gone 24 hours not eaten, and never would my brain have said you're hungry, or my stomach have grumbled. That's the crazy part, but it's also a huge boost. Now, I'm not saying run out and use a medication. I'm saying listen to this. Hear the ideas about what'll make it better, but then identify what's stopping you, because you may have to conquer that before doing the other thing that's all right. They're
Jennifer Smith, CDE 1:14:23 all really like valuable things to keep in mind. Because, as you said, people may go to the doctor and say, but I can't he says, stop eating, or don't eat many snacks. Or I can see how much you're in taking cut it back. And for those who really struggle with some mental stuff around food to begin with, that can be a road to nowhere to just tell them something that the doctor doesn't know. What they feel like, yeah, and it stinks.
Scott Benner 1:14:51 Well, the and the other side of it is too. And I have personal experience with this, with what happened to my wife is she went to an endocrinologist and said, like, Look, I'm just gaining weight. Eat for like, no reason, and lose weight, lose weight, lose weight. And they tested her thyroid, and her TSH was high, but in range, so they didn't give her medication. So for seven years, they yelled at her to lose weight as she gained weight. And then one day, it just took one of us to, like, you know, I guess you people call it advocating for yourself, but I basically just, like, said to the guy, like, just give her the medicine for God's sakes. Like, if it doesn't work, like, take her off of it. But like, what's the harm at this point, right? She starts taking Synthroid, and, boom, oh, what do you know? Look at that. Yeah. And so, like, even when you figure the problem out, sometimes there's another roadblock. And I see that with people all the time. They go through this horrible thing to figure out their problem. And they get to the person, they're like, hey, gatekeeper, give me the thing. And they go, No, you can't have the thing. And it's tough. You know, finding a doctor who understands what you figured out is a big deal, and I it's a whole other process to talk about how to explain that to a doctor. But, you know, I just don't give up. Is my is my message? I guess, yeah, yeah, no. All right, Jenny, this was awesome. Thank you very much. Of course, yes. Thanks for tuning in today, and thanks to Medtronic diabetes for sponsoring this episode. We've been talking about Medtronic mini med 780 G system today, an automated insulin delivery system that helps make diabetes management easier day and night, whether it's their meal detection technology or the Medtronic extended infusion set, it all comes together to simplify life with diabetes. Go find out more at my link, Medtronic diabetes.com/juice box. This episode of the juice box podcast was sponsored by us med. Us, med.com/juice box, or call 888-721-1514, get started today with us. Med, links in the show notes. Links at Juicebox Podcast com, if you or a loved one was just diagnosed with type one diabetes, and you're looking for some fresh perspective. The bowl beginning series from the Juicebox Podcast is a terrific place to start. That series is with myself and Jenny Smith. Jenny is a CD CES, a registered dietitian and a type one for over 35 years, and in the bowl beginning series, Jenny and I are going to answer the questions that most people have after a type one diabetes diagnosis. The series begins at episode 698, in your podcast player, or you can go to Juicebox podcast.com and click on bold beginnings in the menu. Hey, thanks for listening all the way to the end. I really appreciate your loyalty and listenership. Thank you so much for listening. I'll be back very soon with another episode of The Juicebox Podcast. The episode you just heard was professionally edited by wrong way recording, wrongway recording.com, you.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#1025 Diabetes Pro Tip: Transitioning
Scott and Jenny Smith, CDE share insights on type 1 diabetes care
You can listen online to the entire series at DiabetesProTip.com or in your fav audio app.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - Radio Public, Amazon Alexa or wherever they get audio.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:04
Hello friends, and welcome to the diabetes Pro Tip series from the Juicebox Podcast. These episodes have been remastered for better sound quality by Rob at wrong way recording. When you need it done right, you choose wrong way, wrong way recording.com initially imagined by me as a 10 part series, the diabetes Pro Tip series has grown to 26 episodes. These episodes now exist in your audio player between Episode 1000 and episode 1025. They are also available online at diabetes pro tip.com, and juicebox podcast.com. This series features myself and Jennifer Smith. Jenny is a CD and a type one for over 35 years. This series was my attempt to bring together the management ideas found within the podcast in a way that would make it digestible and revisit double. It has been so incredibly popular that these 26 episodes are responsible for well over a half of a million downloads within the Juicebox Podcast. While you're listening please remember that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise, always consult a physician before making any changes to your healthcare plan or becoming bold with insulin. This episode of The Juicebox Podcast is sponsored by assenza diabetes makers of the contour next gen blood glucose meter and they have an amazing offer for you. Right now at my link only contour next one.com forward slash juice box free meter you can get an absolutely free contour next gen starter kit that's contour next.com forward slash juice box free meter. while supplies last US residents only. The remastered diabetes Pro Tip series from the Juicebox Podcast is sponsored by touched by type one. See all of the good work they're doing for people living with type one diabetes at touched by type one.org and on their Instagram and Facebook pages. This show is sponsored today by the glucagon that my daughter carries G voc hypo pen. Find out more at G voc glucagon.com. Forward slash juicebox. What I would like to talk about today is transition. Just a an overview concept for this one, but transition from just finger sticks to CGM transition from MDI, to pumping, transition from pumping to algorithm. Sure, can we do that? Yeah, I thought we could all thank Isabel here for having her finger on the pulse of the people in the Facebook group and knowing exactly what people ask about and what they seem most confused about. Why don't we start with MDI, because everybody starts there, right? After you're doing it for a while, like let's put ourselves in that place. We've been doing MDI for a while it's working pretty well, or at least at a baseline. We're shooting a Basal insulin once a day, and we are shooting a meal insulin to correct blood sugars and to cover our carbs. That's the basics of MDI. Okay, correct. So then we're in a doctor's office, but it make up yeah, I'm gonna make up some numbers. Let's, let's say our Basal it's like, I don't know, let's say our basil is 10 a day. And let's say we're, I don't know, one to 10 for carb ratio. Okay. All right. Let's say our correction is one to 100. Let's keep it all very like, like that, so that it's easier
Jennifer Smith, CDE 3:53
to talk about. Okay, round 10 numbers
Scott Benner 3:57
and numbers, we're gonna do that. So the math makes sense when people are listening. So we're in the doctor's office, and the doctor says, you know, you might like a pump. Is he gonna say it just like that? I mean, if it's a lady, she might be like, You made like a bump? I don't know, like, exact. or anywhere in between. There's some women have more masculine voices. Jenny, this isn't the point of what we're talking. Oh, yeah. So they see you might like a pump. You are. I'm guessing. Gonna have a couple of different reactions. I see a lot of people scared. Oh, no, don't change something. I see a lot of people are like, Yes, please. Because this isn't working. And maybe this will they don't know why they think that just right. They're hoping for a change. So the first thing that's going to happen is the doctor is going to translate your Basal insulin to this pump. So Jenny, you do that math for me? I get her I get 10 units a day. Injection. What are they going to do on the pump for me?
Jennifer Smith, CDE 4:56
Most often on a pump, because it's expected that your Basal insulin which, and this is kind of outside of it, but within your Basal insulin will now be given by the pump as rapid acting insulin. So that's the first thing to understand is that you're injected Basal insulin, which is a specific long acting kind of insulin will now sit in your refrigerator as a backup in case of pump failure, right. So you don't put Basal insulin into a pump. The only insulin that goes in the pump is your rapid acting insulin of any of the brands, right. Depending on the pump, company, they all have a little bit of different kind of recommendations for type of rapid insulin, but it's a rapid insulin and to translate your Basal dose of what we said 10 units into a pumped Basal delivery, you would essentially take 10 units into a 24 hour day. Right? And that translates into a a dripped amount, right? Because insulin pumps drip drip, drip drip consistently to deliver that total amount of basil that you want.
Scott Benner 6:15
Okay, so let's clean it up for people who get lost very easily. You may be injecting trust Siba love Amira, Lantis, what are the other ones, Basil Glar.
Unknown Speaker 6:27
These are all basil, JL,
Scott Benner 6:29
these are basil insulins, these are now gone. You don't use those anymore. Because as Jenny points out, you're going to take your mealtime or your fast acting correction insulin, put it in the pump, and it's going to split it up, those 10 units are going to get split up over, not just over hours. That's how the settings the pump work, right, you're going to come up with what is it going to be like point four, maybe an hour if you're 10. Today about like that, right? Right, depending
Jennifer Smith, CDE 6:53
on your pump, all of the pumps differ in their precision of a single drip of insulin. Some pumps can drip as little as point one, one, some can drip as little as point oh two, five, or point oh five. So it just depends. But if you broke this down 10 units a day into 24 hours a day would be a rate of about point four, two, if you do rounding, right, some pumps, you may have to round that 2.4, because they can't deliver the point oh two,
Scott Benner 7:24
and you're, you're gonna hear that if you're MDI and think, oh, at the top of every hour, it's gonna give me point 14 Its events on but it's not doing that it's going to break those correctly for Twos Up over the entire hour, over the
Jennifer Smith, CDE 7:36
course of the time. Exactly. Now, the other step to this calculation is that we expect that your Basal insulin you've been injecting I'm trying to think how to say it, so people don't think their insulin is not working. But when you inject Basal insulin as its type it, it will not be absorbed as efficiently I guess is the better way to say it as it would from a pump where it gets infused in those little tiny drips over a very precise amount of time, a very precise dose. So your rapid insulin in your pump gets infused out of sight. And so we usually take your base Basal dose down by about 10%. Some even some physicians even go down by 20%. But the general idea is taking your base dose down by 10%. So 10 units a day taken down by 10% is one unit less, so nine units instead of 10 units. So if you do the math there, nine into 24 gets your rate down instead of point, let's call it point for an hour, down 2.37 an hour, which again, we'd probably round down 2.35.
Scott Benner 8:48
And you're going to want to keep an eye on that because I've seen it go either way. I've seen that be right. And it's amazing. I've seen that beat Now. Not enough insulin and people are getting high blood sugars. And they immediately like you hear them say like the pump doesn't work like well, you gave yourself less insulin and turns out you need right. So pay close attention to that.
Jennifer Smith, CDE 9:10
It also translates into the next step. Once you've been making some notes on this 24 hour dose of let's call it point three, five units an hour. And you can say Well, it seems okay here. But then at this time of the day, I'm always high no matter what I can skip eating and I'm high I can eat and I go even higher. Well, that's when the next step is Basal testing. Right? We need to really look at it and say, where is that point three, five, sufficient and where is it not and where might it be too much.
Scott Benner 9:43
And you might notice, and this is this might sound a little heady if you're thinking of switching but you could put your pump on your belly and have a different reaction to the insulin that is if it's on your hip or your thigh. There's reasons like Arden's thigh doesn't work as well. As her stomach does,
Jennifer Smith, CDE 10:01
you know, neither does mind I don't use my thighs anymore. Yeah, back of your arm might
Scott Benner 10:05
be better than your, the back of your butt or who knows, like, right
Jennifer Smith, CDE 10:10
and with with this being new from coming from MDI, to going to using a pump, I would suggest initially utilizing and testing out within an area of the body, you know, we talk a lot about rotation, not only should you be rotating, if you're doing MDI, your injection should be going multiple different places, not just the same site over and over, the same goes along with pumping, those sites need to be rotated. If you're new to pumping, however, you really want to get an idea if your settings are fairly good. Stick with rotating around your abdomen, right? Get an idea. And then once you have that fairly well set, you can then move to upper body or the back of the arm or maybe your thigh or you know, your lower back and see if you notice any difference some people do and some people don't at all.
Scott Benner 11:02
Yeah, right. No, I mean, there's it's your body composition, hydration, how you know where it's actually going inside of you? Is it subcutaneous? Is it very close to a muscle? We don't want to overwhelm people, but the muscle can kind of, I don't know what the term is like, what a large muscle group can, it kind of lessens the impact of the insulin, but for the life of me, I can't think of why right now. Do you know what I mean?
Jennifer Smith, CDE 11:27
Like lessons? I know, I don't know what you know,
Scott Benner 11:28
I always thought that's why the thigh was in a good spot because it was a large muscle.
Jennifer Smith, CDE 11:34
Well, it might have more to do with how well the insulin at that site is getting absorbed. Like that's a big reason that I don't use my thighs is because whenever I tried using it, either I got a collusion alarms because the cannula was bumping into muscle or potentially that I had nicked, like a small vessel under and it had been clouded kind of near that site where it was trying to infuse. And so that backs up into the pump and the pump tells you hey, the delivery of insulin has stopped. It gives you nice alarms. Right? So I think in some cases that may be part of the issue is the proximity to muscle. Yes. But also I it was either painful or I got occlusions like it just never worked on my thighs.
Scott Benner 12:24
Okay, I'll see. Look, I'm learning from the podcast. Finally. Finally, I learned about this every day, you learn a lot. Yes. Okay. So now we've, I think here's a good place to insert that it is possible that there are some people in the MDI who are achieving reasonable lower blood sugar's some how do I say this? Sometimes your doctors over baseline you because they don't think you're covering your food correctly. And
Jennifer Smith, CDE 12:55
that, or they may not have looked at your records enough to know why they've you know what I mean? Like, it might just be easier to backup with enough Basil with what they're seeing in your data. Yeah. And it may as you're saying, it might be wrong, right,
Scott Benner 13:09
right. So like, imagine if you're a person who has been getting more basil than they really technically need, but you kind of forget meals, sometimes you don't cover all your food. But now all of a sudden, you have this pump, you're like, Oh, it's so easy. Now, I just push the buttons for my food. So now you're covering your meals well, and you're like, why am I low all the time? Right? It might be because you're using more insulin than you have been in the past. So those are things to look for that I see people struggle with the beginning with a pump. And I do want to say I think there's a I think there's a period of transition there. It's not going to be like if you're nervous. It's not unfounded, you know, like you are starting a whole new way of doing something. But it really is just another way of delivering insulin to you. It's not that complicated.
Jennifer Smith, CDE 13:59
And I can say personally, when I switched from MDI, having done MDI a long time before I started using a pump. By the time I started using a pump I was already doing. I was already doing somewhat of a Pre-Bolus. But it wasn't the same once I switched to a pump, there was a definite time difference between my Pre-Bolus with injections, and there still is, I can take an injection and my Pre-Bolus Time is not as long as it is on a pump, right? Again, and have one. But that's what I noticed. And so those are some things to pay attention to between MDI and what you're doing along with what you said about maybe the doses you were taking on MDI. We're covering a certain way for your rapid insulin for meals and corrections. And now that you're on a pump, your meals, the food hasn't changed, your strategy has stayed the same and things are looking weird,
Scott Benner 14:58
right right there in You'll have to step back a lot and try to see what's happening. One reasonable reason for that could be reasonable reason why it wasn't right. But anyway, you use an omni pod and delivers insulin a little slowly. Like it doesn't just like you take a needle and you go. Yeah, and the pump is pumping over time. And and I don't imagine you use very large bonuses, but larger bonuses take longer. Yeah, I've seen, I've sat at a restaurant with Arden. And, you know, you forget you've done it, and you kind of still here like that, like think like click clicking, it's still giving her insolence feels like it's been five minutes, you know, and yeah, so that's, that could be part of it. Anyway, these are things you're going to learn along the way. They're new lessons, but they're not a reason, not just try, because you're going to gain weight, you're gonna gain so much, right? Like if, to me a pump is, at its core, I've always thought of pumping as a way to be able to manipulate basil. Whereas on MDI, I shoot it in, it's in there, nothing left to do. If it's too much, if it's too little, it's what it is, you know, with MD with a with a pump, you know, you can go back and listen to the Pro Tip series, I think about like, wow, if we sit down to a meal, that's all of a sudden, much carb heavier than what I usually eat, I could do a Temp Basal increase, they tried to help me with this. You know, I was thinking a minute ago, when we were talking about breaking the 10 units down into point 4.35, that if you think about putting a sprinkler out on a dry, dry lawn, right, and you need to give your lawn 10 gallons of water, you could come along and dump it on all at once. It'll just be there, that'll be it, right, or it could break it up into little point three, five gallons every hour and go back and forth. And just a light covering, covering, covering, covering, you're never gonna soak it down, you're and it's just I think of basil like sort of like that. Sometimes you're just,
Jennifer Smith, CDE 17:03
and that's a good way to think about it too. Because if you consider that slow Basal drip that you are getting from a pump, when you inject your Basal insulin all in one clump, right? You can, depending on the kind of activity you like to do, you may have found that you have to pay attention to Gosh, I'm doing like a really heavy arm workout, I'm probably not going to inject my Basal insulin into my arm today, I might inject it someplace else, right? Because there's this whopping dose sitting underneath your skin. And any kind of insulin, whether it's rapid, or Basal can get enhanced in action, the more active you are, and especially if you're using that site. So, you know, those are the kinds of things that having those tinier doses that you can manipulate and adjust, especially with the variables that you know, are coming in the day.
Scott Benner 18:04
If somebody's listening and thinking like, well, they have spent the first 15 minutes talking about Basal insulin, it's because it's really important, and nobody tells you it's important in setting. So if you listen to this podcast, like Well, I do MDI, they're always talking about, like, their settings on their pump or anything. This is still settings, you know, if it's MDI, it's your settings, it's, you know, these Basal carb ratio, correction factor, they're all settings. So it's just very important to have them. If they're not accurate to your needs, then everything else is just going to be a mess. And especially Basil, basil is wrong. The whole day is confused. So okay, so we've translated our basil, our insulin to carb ratio, does the doctor keep it the same? Do they usually like what is common?
Jennifer Smith, CDE 18:49
They may keep it the same, especially if your records prove to show that it seems to be for the most part working fairly. Okay. Right? Could there be improvement somewhere, possibly, or whatever, maybe that's also part of the reason that they feel like a pump might actually be better. Maybe you're the kind of person that just eats really slow digesting food. And so you've had problems with taking your insulin and having these big drops in your blood sugar too fast, and then it ends up catching up with you. And then you end up high later, and you've treated low blood sugars, right? And there's not a timing thing that you can really get quite right with MDI. And maybe the doctor says, Well, why don't we try a pump, because, hey, you're eating these types of foods more frequently. We could actually use some of the smart features on our conventional pumps that allow you to take some insulin for food. We're calling these extended boluses. And you can just kind of like basil. It's almost like a secondary use of Basal but for a Bolus where you drip drip, drip drip drip a Bolus in over a certain amount of designated time. You
Scott Benner 19:55
know, there's just there's so much you're gonna get out of having a pump there. Yeah. There's also going to be some things you need to know, sites can, like they're going to tell you whatever pump you have, they're gonna say this pump you can wear for X amount of days or X amount of hours. But sometimes sites go bad. You know, sometimes new sites don't work as well in the beginning. Those are little things that you'll learn along the way. There's, if depending on Arden's blood sugar, she might put on a new pod, and we might just Bolus a little bit to get the site working. This morning, I woke up in the morning, I saw that artists blood sugar was trending up overnight. And listen, for those of you just switching like Arden is looping, but I can see how much insulin is left her pod remotely, which most of you aren't gonna be able to see. But I can see she was down to like 30 units. So this is the end of her sight, right. And I just spent the weekend with her. And doesn't matter. But we were in a lot of restaurants this weekend. So Arden got a lot of insulin this weekend. And in my heart, her blood sugar is drifting up, because this site is kind of done. So because you have experience, yes, I can just tell and you will be able to one day as well. So I sent her a text and I said I wouldn't go to class with this pump one. Because if she does, she's going to spend her whole day with blood sugar's around 150. And she's going to be fighting with them constantly, and bolusing. And they're not going to work and and by the way, if that happens, and then all of a sudden she gets crazy active out of nowhere, she might experience a low blood sugar from all this insulin kind of sitting in this right over use. Well, yeah, get in this pool, right? And so like, that's just the thing you'll learn along the way, you'll learn, you know what people worry about so much like, well, you know, do you travel with pumps? You know, if we go too far from our house, we do if it's a 15 minute turnaround, we don't like you know what, I'm gonna have to have insulin with me now. Like, yeah, I don't know, we don't travel with insulin that frequently, as long as we're near home base, you know. But if we go far, you know, half hour, 45 minutes, and it's not something we want to turn back from, we'll take insulin with us, you know, it's just you. My point is, is that it becomes all second nature at some point. Just like everything else about diabetes, you're gonna have experiences they're going to teach you you'll learn from them and move on. Speaking of moving on, you'll think I'm going to go from MDI, to pumping, to pumping to algorithm pumping, but I want to do CGM first. So okay, you have a meter. And that's how you check your blood sugar. And that's all you have. Hey, you're in the doctor's office. The doctor is like, you know what you want to do?
Jennifer Smith, CDE 22:42
It must be the same deck.
Scott Benner 22:43
I wanted to draw here. Take this a sample you try. You'll love it. They're gonna try to give you they're gonna say to you, hey, you might want to libre, you might want to Dexcom if you're on a Medtronic pump, they might ask you to do whatever the Medtronic CGM is called. And you're gonna say I don't need that or you're going to be newer. You're gonna Yes, please. That remastered diabetes Pro Tip series is sponsored by assenza diabetes makers of the contour next gen blood glucose meter and they have a unique offer just for listeners have the Juicebox Podcast. If you're new to contour, you can get a free contour next gen starter kit by visiting this special link contour next.com forward slash juice box free meter. When you use my link, you're going to get the same accurate meter that my daughter carries contour next one.com forward slash juice box free meter head there right now and get yourself the starter kit. This free kit includes the contour next gen meter 10 test strips 10 lancets, a lancing device control solution and a carry case. But most importantly, it includes an incredibly accurate and easy to use blood glucose meter. This contour meter has a bright light for nighttime viewing and easy to read screen. It fits well on your hand and features Second Chance sampling which can help you to avoid wasting strips. Every one of you has a blood glucose meter, you deserve an accurate one contour next one.com forward slash juice box free meter to get your absolutely free contour next gen starter kit sent right to your door. When it's time to get more strips you can use my link and save time and money buying your contour next products from the convenience of your home. It's completely possible that you will pay less out of pocket in cash for your contour strips than you're paying now through your insurance. Contour next one.com forward slash juice box free meter go get yourself a free starter kit. while supplies last US residents only are touched by type one has the back of people living with type one diabetes. Take for instance, their D box program touched by type one knows firsthand the intricacies of living with type one diabetes. And so their team has created a D box which is a starter kit that provides important resources and supportive materials to individuals with diabetes, they want you to thrive. The D box is completely free and available to newly diagnosed people. All you have to do is go to touched by type one.org. Go to the Programs tab and click on D box. While you're there check out all the other resources and programs available at touched by type one.org. Speaking of support, touched by type one.org is available in English and Spanish. Don't forget to find them on Facebook and Instagram too. You do not want to miss what touched by type one is doing. When you have diabetes and use insulin, low blood sugar can happen when you don't expect it. G voc hypo pen is a ready to use glucagon option that can treat very low blood sugar in adults and kids with diabetes ages two and above. Find out more go to G vote glucagon.com forward slash juicebox G voc shouldn't be used in patients with pheochromocytoma or insulinoma. Visit G voc glucagon.com/risk. Wherever you fall on that you do want it if your insurance covers it, you want it? That's for sure. Right? Tell me why.
Jennifer Smith, CDE 26:38
And I think it applies in all realms of diabetes as well. Right? Not just in type one diabetes, but also type two diabetes and even worthwhile and gestational diabetes. I know there are some rules in terms of when it can be prescribed whatnot. But I think it's beneficial all around what you miss with finger sticks are all of the little dots in between. So where things were trending, right, so if it is something that your doctor does bring up? Absolutely say yes. Right. You may not know how to look at the information or what you're getting from it initially. But it's so worthwhile. You want
Scott Benner 27:21
to know what you don't know. And with finger sticks, especially if you're newer to diabetes, or if you just been doing them your whole life. And this is how you tend to think of it. You do the well i i test before I eat or I test before I go to bed or I test before I drive. And and I know you've asked yourself what's happening when I'm not looking. Right, like and if you haven't asked yourself that. I wonder how do I go from 250 to 50 in an hour, like how does that happen? And you'll learn you'll start seeing the impacts of activity and the lack of hydration and different foods that you eat, the age of your your insulin pump site, all these different things that have a huge impact on the way your blood sugar moves. And now suddenly, it's there. A CGM is going to show you minute by minute. I think it's every five minutes. Right.
Jennifer Smith, CDE 28:21
And I think there are there are some people who have been using it long enough that can say there can be some frustration around the amount of data that you get. And I wouldn't disagree with that. I but I do you think it's how you interact with the data, right? It's how you actually take a look at things and what you do with it and what you learn from it. And you have to you have to expect that in the first month. Let's call it of using a CGM, you're gonna see a lot of stuff. And so rather than being so very emotionally reactive, again, taking a step back and kind of looking at the data to be able to make better decisions about what you felt like was probably happening. And now you can actually see,
Scott Benner 29:10
well imagine you have your sprinkler out on the yard. And you have to keep the dirt moist because you've planted grass seeds, except every time you look out it's kind of dry. That's the CGM. You look at the CGM ago Oh from 3am till 6am. My blood sugar's 140. It's pretty stable, but it's 140. I wish it was lower or moister. I can turn up the sprinkler a little and put on a little more insulin and make it where I want it to be like push that number down a little.
Jennifer Smith, CDE 29:37
And the CGM can show you that if you're really looking at it. That way the CGM can show you where did it start to lose right effect? Where do I start to need to add more insulin? It's not once you get stuck higher or once you get stuck lower than you want. It's before that so any drifts up or drifts down. Now, you can see that very clearly on a CGM I, you have a really good example I think from when Arden first started using her CGM, it was like that overnight thing that you are constantly missing was at Lowe's when you had finger sticks. And I would put
Scott Benner 30:14
or you could see them. I thought it was a genius. I've said it before I would put Arden to bed at 180. And she'd wake up at 90. And I was like, Look how good I am at this. And what would happen. We put a CGM on her. She was 180, she'd go down to the 50s sit there for hours, I'm assuming her liver would be like, hey, here, try not to die. Here's some, you know, some, here's some, here's some glucagon, I'll give you a little bit. And then she drift up to 90 overnight was happening constantly. So the reasons for that are mind numbing in not for this conversation, but we were bad at bolusing for dinner, we were her basil wasn't like there were so many things that weren't right, you know,
Jennifer Smith, CDE 30:52
you didn't know it because you couldn't see what was happening unless you really did a finger stick even an hourly finger stick, it would have caught a drift, it still would apply it. But it would have still been confusing unless you sat down and you connected all those dots. And you could say, well look, look at this. And you probably I mean, not necessarily wanting to see your child sit at 50 for three hours before your body actually reacts and gets you the glucose that is needed to bring it up. But you'd have on a first finger stick probably under 70, you would have ended up treating, so you also wouldn't have had the information to show. Well, how much do we need to take away? And what do we need to do differently?
Scott Benner 31:34
I can't I can't say how valuable it is to be able to see a graph and to enter look at it every three hours or you know what's it look like over six hours, like Jenny's point is great is that you? You don't know why? What happened happened? It's um, if you're married here, it's nine o'clock at night. And you're now in an argument. Right? And you think I don't know what just happened. But mostly this is guys like they're like what? They searched the last five minutes in their brain. And I've not done anything wrong in the last five minutes, right. But if you could step back and see a whole graph of your day, you'd realize that at 630. At dinner, you said something really stupid. And now it's hit me at nine o'clock. So I think that that can be similar. You could have cheeseburger with french fries at dinner at eight o'clock at a restaurant and hit it with a great Bolus. And you're like, Oh, well, my blood sugar's still where I want it to be it's 140 After dinner, that's not bad. And two hours later, it starts to jump up. And that doesn't make any sense to you. Because you haven't listened to the Pro Tip series. You don't know about the fat and the French fries and the slow digestion and how you're going to go up afterwards. But at least if you see it on a graph, and then you go have those French fries and that burger again, you see it happen again, you can go Oh, I could get ahead of this. Right? Yeah, I could not say that stupid thing at dinner. And now we'd be watching television, and she wouldn't be yelling at me.
Jennifer Smith, CDE 32:56
Right. And if you have a pump, you can also address it a different way than waiting for it to finally start rising and getting too high. You can offset it ahead of time knowing what is coming because you've had the experience that, oh, it always hits around two hours. So I'm going to start doing something about an hour and a half before that. So that it actually doesn't happen. Right. So I mean, yeah,
Scott Benner 33:21
million ways to handle that if you're from Arden, an hour after she has french fries, we have to Bolus for the fat. And there's a calculation you can do. And there's that heads off that secondary rise and doesn't cause a low later. That's the other great thing is that everyone, when you don't have enough data, you think, Oh, if I just keep throwing in more insulin here and there, it's gonna be it's not true. Like you can match the need up with the impact of the insulin and never cause a low. Right. And that's something you're going to learn looking at a CGM that, that uh, that a stable line on a CGM is really, your insulin, your insulin is pulling down, and your food and your other impacts are pushing up. And neither of them are winning like so if you can kind of imagine that line going off into affinity nice and stable. There's invisible lines. cables attached to it. One's trying to pull it up. One's trying to pull the line down, and neither can win because you have a great balance between your insulin and your knee. Yeah, so that in the CGM, like, seriously, like I don't care like there's decks comms and advertiser. It's not like I'm saying that like get a CGM. It's of any,
Jennifer Smith, CDE 34:33
right? Absolutely. I mean, I've said before, many times if somebody was going to take my technology, I would fight for my CGM. Before I'd fight for my palm. Yeah, no, I would 100% would keep my CGM.
Scott Benner 34:47
I'll throw this here too. Even though it's about like, leaving quote unquote, finger sticks. You're never going to leave finger sticks by the way, you're going to need them. You're gonna pass when you're not sure about your CGM. You're gonna test when you're making big I listen to my daughter's blood sugar looks high on her CGM, and we're gonna make a big Bolus. I said, Look, you gotta test, we got to know this numbers, right? We can't just start throwing insulin in here. And you're actually 40 points lower than this or whatever.
Jennifer Smith, CDE 35:12
And I think it's also really important to acknowledge what you know about how you feel around certain blood sugars. Because, again, technology. It's wonderful. And it's so much better than it was years ago. But it may still not be accurate at certain points. So always those finger sticks are important to continue to use. Because if your symptoms or how you're feeling doesn't go with what your CGM is reading, I guarantee a finger stick isn't gonna lie to you not unless you still have like, apple juice on your fingers or something.
Scott Benner 35:47
I was gonna say, and I didn't get to it just an accurate meter, just the blood glucose meter. Yes, they're not all the same. They don't all work as well. Don't just take the one that doctor handed you from the drawer, do a tiny bit of research. He's the one that I that advertises here because that's the one we use and it's amazing and, you know, like or do what you can do your own research and find out I will throw out a little story here. Because I did spend the weekend with my college age daughter, which I haven't done in a while as a visitor at school. Second night she was with me. We replaced her CGM. Okay. So at five o'clock at night, I said, Hey, your Dexcom is going to expire one in the morning. You should switch it now. It's before we're gonna eat dinner. We'll get it back online. It will have it we can do some finger sticks through dinner. And then it'll be rolling and working well by the time we go to sleep, because it does take a little while for some people to look right. You know? She does. I don't want to do that right now. So then when do we change her CGM? 11 o'clock, you know, like, oh, so then it's done. So then it's wonky for the first couple hours. And for Arden, if her Dexcom is wonky, it's wonky low when she first puts it on, mine is too. Okay. So like I made it, it'll be like you're 42. And she's 100. Yeah. 10. Like that kind of thing. Yeah. So there's a lot of consternation in what you should do. I'm a fan of letting it be on for a little while and calibrating it to help it get along a little more. But now we're asleep. And it's like Beep, beep, beep. All I could think was like that tone. I know. I said this. Nobody listens to me. But that's fine. And I'm like, and I know she's not that low, like and but it's worrying. So now she's, she's asleep. And I get up and I'm checking her blood sugar and she wakes up. She's like, What are you doing? I'm like, your CGM is going off. She goes, I'm fine. It's like, okay, so I tested her. And she was 130. And I was like, okay, so she's right. And I did a calibration and it came together pretty quickly. And that was it. Having said that, we could have done that at five o'clock. There. So there is a way to time, your technology. Now the new g7 is going to have a shorter warmup period, which will help overlapping you'll be able to soak your sensor, which I'm not going to bother explaining here. But as the technology gets better, so should those things. But that is not to say it's not like hands down. The most valuable thing that's happened to people who have any kind of diabetes, since I've since I've been aware of diabetes, some absolutely. Okay. All right, Jenny. Now we got our CGM. We're using a pump. We're looking online. And we're like, see, this isn't that the doctor is not gonna go you know you ought to do. That's not gonna happen now. Because this stuff's also new. Maybe maybe a really in tuned doctor might say, once you get an algorithm, but for the most part, I don't think I think that's the thing you're going to figure out on your own a little bit. So all this stuff we're talking about about, you know, the Bayes will be incorrect. And you might need a Temp Basal here, you might need to extend a Bolus for fat, you might need all this. There are pumps that make those decisions autonomously. Yeah, you have to be wearing at this time, you have to be wearing a Dexcom. Because it works with that. Right, but
Jennifer Smith, CDE 39:08
or med tronics. CGM? Yes, because they're their system also works with their pump, right? Yeah, so
Scott Benner 39:15
there's a Medtronic version of this. There's a tandem version of this. There's an omni pod version of this. All their algorithms are proprietary, they work slightly differently, but long and the short of it is they're going to give you insulin when you need insulin, and they're going to take insulin away when you don't need it. They're going to endeavor to stop you from getting low and endeavor to stop you from getting too high. You
Jennifer Smith, CDE 39:37
still had how they do that it was with targets Yes, right. Right, specific targets in each of the different pump systems. Medtronic newest one was just approved, which is really nice. But they all have specific targets. So how that algorithm works is based on when and how to give you more or less be Send a target and based on what the system is projecting off of your current CGM trend. So it's a very interesting like the algorithms don't just willy nilly deliver or take.
Scott Benner 40:13
Like, I think maybe now more,
Jennifer Smith, CDE 40:14
right? Yeah, exactly. There's a math to the algorithm
Scott Benner 40:19
Gremlin inside of your pub flipping a coin going, Oh, my God heads. Let's do it. So but it's it's it's stunning. Now there's another version. There's a number of other versions there are Do It Yourself versions. There's Android APs. There's loop. I think, Jenny, you loop. Right. I do. I think you and
Jennifer Smith, CDE 40:37
I've been looping for five and a half years.
Scott Benner 40:41
And Arden has been doing it I think since 2019. Maybe? So okay, yeah. And your Arden's using loop three as a mic, and you just switched to it as well. So like, so they're all just different versions of an algorithm making decisions about insulin based on your CGM tread tread. That's it? Yep. They're astonishing. They work incredibly well. They are not magic. Again, all settings, all knowing how to Bolus for certain foods, understanding the impacts of things, your digestion, your hydration, like all the things that are important about MDI are the same things that are important about pumping are the same things that are important about using an algorithm.
Jennifer Smith, CDE 41:28
And you made I know, people can't see you, but you were very in a line going from MDI, to pumping to algorithm. And I think that's, it's a really important piece. For those who are listening to understand if you're kind of listening to this, because these are not pieces in your life already, right, and you want to get an idea. There is 100%, I'd say 1,000% value in learning on MDI. And then moving to a conventional pump, that does not do anything for you, meaning it does not use an algorithm. There's absolute value in that, you know, we talked about testing, and evaluating settings, and learning about all the variables, food and activity and everything, and how to adjust your pump, or your insulin doses to accommodate for those variables. I think, as you mentioned, when you said, you know, your pumps, like, hey, let's start on algorithms. I can't go as deep as you. So it's a totally different doctor. Right. But in that sense, there are I think, more doctors today who are thinking algorithm, but in my personal and professional opinion, I think some of them are thinking that too fast. Okay? They are they are moving somebody to, hey, you're MDI, let's move to this algorithm driven system, whatever the system is, whether it's Omnipod, five, or tandem or Medtronic there is, there's a missing piece in the middle there, that if for some reason, and we talked about CGM is potentially not being always accurate or technology failing. If your pump fails in its algorithmic dosing, and you have nothing to step back to, you're at a loss. And it's important to understand that, you know, so I can't emphasize.
Scott Benner 43:32
It's incredibly important. Jenny's been talking to me about this privately for years. Honestly, she's like, people can't just be put on the machine, the machine does the whole thing. And they don't understand why it's happening. Because, you know, the general argument is what if the machine stops working? I don't even think that's the need for that I think the need is that this is a thing you have to understand. Like it right, no matter what none of this machine stuff is at the point where you don't need to know how to how it works. It's not AI, it's not even a computer like you know, you used to have to know how to fix your computer because it would break all the time. Nowadays, you buy a Mac, it'll just do the thing you want it to do, you'll never have to touch it, and it'll die. At the end. You'll recall my math doesn't work anymore, you get another one. And you don't need to understand how a computer works. To use a computer. You need to understand how diabetes works. To have diabetes. I don't care what version of care you're using. I don't care what the next one is. Now, if someone magically comes up with something one day, where it just works, no matter what, like a, like a laptop from Apple, okay, then then okay, then God bless. If you want to skip it, then skip it. But I'm still gonna say that isn't happening anytime soon because of not just the things we've mentioned today. You know, your insulin pump site might not work on time, like your CGM might not be right right away like all the other things. It's just not happening anytime soon. So you don't want The worst thing I can imagine is that you put an algorithm on a nine year old who it works for. And then five years later, the kid hits like puberty hard or something, and you have no idea, like the algorithms doesn't know you just became a completely different person, you're gonna have to change your settings to make that work, right. And that takes experience. If you I think if you ever find yourself listening to Jenny and I talking and thinking, How come whenever something comes up, they just fill the next space with something valuable. It's because Jenny has been living with diabetes for over 30 years. And I've been staring at my daughter for 15 years watching her have diabetes, and I have a never ending supply of experiences and answers in my head because I live through them. Yes, that's why and that's why you absolutely yeah. Like you didn't go to like diabetes University where they told you something secret that they don't tell everybody else, right?
Jennifer Smith, CDE 46:03
No, no, not at all. I mean, I have valuable behind the scenes, like information about disease states and those types of things from a medical knowledge base. Absolutely. And understanding them helps me to understand some of the navigation of that with diabetes, but the lived experience and the work that I get to do with so many people, that's the valley that you can't teach that right? In a university, you you can't teach, there's no degree and diet.
Scott Benner 46:36
And for your situation, you've been helping people for so long. And professionally. I tell people all the time, like, it's, it's gonna sound self serving, but it's not like, it's that I was able to get advertisers for the show. So I could turn the show into a job so that I could put this much effort into it. Because I learned that every day I talked to people, like you'll hear me say, like, Oh, I was talking to a guy the other day, he said something about this, that's me. hearing something I'd never heard before and right and retaining it and being able to apply it to a situation go, oh, you know, where that'll help here. And then you get to keep expanding those conversations. I'm gonna get to something here. And you get to keep expanding those conversations till they help other things. We did fibroid episodes. Now we hear from people are like, Oh, my God, my life is different. Because I got my thyroid managed, well, I'm getting a lot of my I didn't realize about my iron and my ferritin, like, a lot of women especially are getting back to me, like they're feeling so much better, because it's something they heard on the podcast, they heard it on the podcast, because I was able to focus on this because this is what I think about. And now and now it's coming to digestion. And that because we had to figure out a problem with my daughter's digestion. And then we shared it on the podcast now I've seen that help other people. That goes for little things about diabetes, too. Yes, that's how this stuff spreads. This is a repository of information, but you're gonna build that in your own mind. Correct? Not if somebody slaps new algorithm on you and tells you don't worry about the thing will take care of it.
Jennifer Smith, CDE 48:07
Right? Because it one that's such a, that's such a big thing that I hear well, shouldn't it be helping me with this shouldn't be doing this shouldn't? The one word I hate is learned, I shouldn't have learned that I don't need this much insulin at two o'clock in the morning. Nope, your system isn't learning. I promise you. It's not learning. It doesn't keep track of two o'clock in the morning, gosh, I gotta give less insulin for this person. It's not that's it's not smart.
Scott Benner 48:33
And Jenny, you know, oddly enough, as we make this episode, I put up an episode today called Rise of the Machines, where a guy comes on to talk about his Android APS system and how it he does believe it's going to learn in the future, which is so exciting, but not now. Like, you know, what's one of his examples? He said, location services. So if you say I'm having pizza, and it realizes you're at Domino's, okay, and you have an experience with insulin, someday, it will remember that experience. Yeah, if you go to a different pizza place and have a different experience. It'll remember that if you go to a third pizza place, it'll remember that if you head back to Domino's, it's gonna go Oh, we're back at Domino's. This. That's not happening right now.
Jennifer Smith, CDE 49:22
No, in fact, there is there are some. There are some apps that actually you can track that way. Like you can take a photo of something and tap the location indicator and the next time you come back to that location, you'll be able to see what your dosing looked like what your CGM trend looked like so you can learn from Bob's pizzas, Friday night last week to this Friday night. Maybe I should change my strategy. It looked like this and I want to improve this right or do it differently, but those they need to be married right into the pump so that not only do you have Okay, now I'm at Bob's pizza. This is what I had. And hey, let's the pump then can acknowledge and I'm going to do something different for Jenny.
Scott Benner 50:06
But for that happening just automatically, that's not here yet. 2023 on the pod five doesn't do that. Tandem T slim doesn't do that the control IQ doesn't do that the Medtronic doesn't do that. They know it may have happened one day. Sure. But the other I think the other thing is, I know you want your days to be easy. And they can be they can be much easier than they are now they can be more your intuition can come into play as you grow. But this is a lifelong thing. And what you want is you want to get to the point where I saw Arden get into this weekend, where we sat down to this meal, there were 16 different things. And she just looked at it and picked up her phone and went and push the button. Yeah. And I was like, How much does she give? She was I don't know, I told her it was like 85 carbs. And I was like, and she and I was like, okay, and then she was okay. And it was okay, look at a table at a restaurant. And she's like, I think about this much. And that's boy, forget this podcast and everything else. It's that's where you want to get to where it just where you wake up at two in the morning, you see a high blood sugar and you go, Oh, I know what this is. And that does come it really does come. So anyway. But you're going to transition along, by the way, I think algorithms are amazing. And
Jennifer Smith, CDE 51:31
yes, they are absolutely i i love my algorithm. Absolutely. But I've also learned to work with it. And I've learned what it can do and what I still need to tell it to do. I think that's the big thing about algorithms is knowing that you still have a fair amount of action to put in to it so that the algorithm can work with you.
Scott Benner 51:53
Yeah, yeah, I wouldn't want anybody to think like, oh, you're using a do it yourself loop. It's magical over the other. There, it all is about the same. Like they all need your help. They all need your intuition. They all need your knowledge. There's nothing if you think you're going to just put a loop on or on the pod five, and it's just going to be perfect. Like, you don't have to do anything. Like that's not going to be the case. No, yeah. So but don't be afraid. Like I'll say something here on the spot myself Saturday, make them clean and make myself set up. Yesterday was my friend Mike would have been my friend Mike's birthday. And I don't want to bring all this down. But Mike had diabetes, type one when we were teenagers. He's not with us any longer. I believe that one of the reasons Mike's not with us any longer is because Jenny alluded earlier that I was stepping along with my hands while I was talking about things like Mike never came along. He just somebody gave him regular an MPH. And he used it long, long after he should have been and you know, didn't have updated meters and didn't you know, he didn't do the little things that you do to come along. I mean, I guess what I'm saying is you don't want to be managing your diabetes like it was 10 years ago.
Jennifer Smith, CDE 53:12
Right? I don't think he's tonight. I think you're also bringing something in here. That's really important to consider. Because you've you've talked about, you know, practitioners bringing up hey, why don't you try a CGM? Hey, why don't you try a pump? If, if you're the one always going to your doctor asking for what's new. I don't know. I you know, and your doctor is very willing and can talk about it then with you. Maybe they didn't bring it up. But they're very, they're knowledgeable about it. Once you do get on it fine. But if this is someone who's never really brought it up and kind of like, shrugs their shoulder and like, sure you could try it, whatever you may need kind of like your friend maybe didn't have a doctor who was keeping up with what could have been better for him. Yeah,
Scott Benner 53:59
yeah. Yeah, you don't you have to take this as a, I don't know if you want to call it a disease or like, some people don't like that word. But this is a way of living, that it begs you to be involved in it. Yes. Like it just it just really does. You have to be aware, you have to take some time to learn what is happening with technology, what's happening with insolence, you know, and you need to move along with it. Because if you look back 50 years, I still interview people who are like in their 70s and have had diabetes forever and they don't even understand why they're alive. Like Like you don't want your life to be a coin flip. You don't I mean, like there are things you can do to to to give yourself better health outcomes. And those health outcomes are not just health outcomes, their quality of life. They're your they're your psychological state of being like there's so much good that comes from just understanding. I know that sounds silly, but How to set your Basal rate and make sure your correction factors, right. And you know how to cover the foods you eat?
Jennifer Smith, CDE 55:05
Absolutely, I think and on a bigger scale, we're also we're all supposed to be a participant in our life, right? health in general, you may have been given good health to begin with, but you're the keeper of that health. Right? It's just like, you're the keeper of the car. If you continue to let the salt buildup on you never wash it off, you're gonna have a rusty car? Well, you're your body's the same way, right? You're the keeper of your health, you got to do things to maintain your health, diabetes, it stepped up a level it is
Scott Benner 55:39
absolutely and so prepare to transition by getting as much good information as you can. But then at some point, you just have to do it. You have to just dive in and do it and then learn a new thing. And then once then you'll be surprised at what else comes from that. And anyway, listen, it's also not to say that you couldn't get an algorithm pump right now and teach yourself backwards. I actually think you can. Sure. I think some people have a harder time with that than others. And I don't want you to be in a position where you're lost and something's happening. And you don't understand why because it won't be any different than a person that gets over Basal on MDI and thinks they're doing okay, but it's not really covering their meals well, right, you know, and then doesn't get hungry one day and it's up low all afternoon doesn't understand what happened, like crack diabetes. There's no reason that if, if you have an if you have enough information and understanding diabetes doesn't have to happen to you. And I think that's maybe the most important part like I would if it feels like it's happening to you, instead of you are doing something and then something's happening. I think you have to have to look and get a deeper understanding, because it shouldn't just be happening to you. That's all. Okay. Awesome. Thank you, Jerry. I want to thank assenza diabetes for sponsoring the remastered diabetes Pro Tip series. Don't forget you can get a free contour next gen starter kit at contour next one.com forward slash juicebox free meter, while supplies last US residents only. If you're enjoying the remastered episodes of the diabetes Pro Tip series from the Juicebox Podcast you have touched by type one to thank touched by type one.org is a proud sponsor of the remastering of the diabetes Pro Tip series. Learn more about them at touched by type one.org. A huge thank you to one of today's sponsors, G voc glucagon, find out more about Chivo Capo pen at G voc glucagon.com. Ford slash juicebox. you spell that GVOKEGLUC AG o n.com. Forward slash juicebox. If you're living with diabetes, or the caregiver of someone who is and you're looking for an online community of supportive people who understand, check out the Juicebox Podcast private Facebook group Juicebox Podcast type one diabetes, there are over 41,000 active members and we add 300 new members every week. There is a conversation happening right now that would interest you, inform you or give you the opportunity to share something that you've learned Juicebox Podcast, type one diabetes on Facebook, and it's not just for type ones, any kind of diabetes, any way you're connected to it. You are invited to join this absolutely free and welcoming community. Jenny Smith holds a bachelor's degree in Human Nutrition and biology from the University of Wisconsin. She is a registered and licensed dietitian, a certified diabetes educator and a certified trainer and most makes and models of insulin pumps and continuous glucose monitoring systems. She's also had type one diabetes for over 35 years and she works at integrated diabetes.com If you're interested in hiring Jenny, you can learn more about her at that link. I hope you enjoyed this episode. Now listen, there's 26 episodes in this series. You might not know what each of them are. I'm going to tell you now. Episode 1000 is called newly diagnosed are starting over episode 1001. All about MDI 1002 all about insulin 1003 is called Pre-Bolus Episode 1004 Temp Basal 1005 Insulin pumping 1006 mastering a CGM 1007 Bumping nudge 1008 The perfect Bolus 1009 variables 1010 setting basil insulin 1011 Exercise 1012 fat and protein 1013 Insulin injury and surgery 1014 glucagon and low Beegees. In Episode 1015, Jenny and I talked about emergency room protocols in 1016 longterm health 1017 Bumping nudge part two, in Episode 1008 teen pregnancy 1019 explaining type one 1020 glycemic index and load 1021 postpartum 1022, weight loss 1023 Honeymoon 1024 female hormones and in Episode 1025, we talk about transitioning from MDI to pumping. Before I go, I'd like to share two reviews with you of the diabetes Pro Tip series, one from an adult and one from a caregiver. I learned so much from the Pro Tip series when our son was diagnosed last summer. It really helped get me through those first few very tough weeks. It wasn't just your explanations of how it all works, which were way better than anything our diabetes educator told us. But something about the way you and Jenny presented everything, even the scary stuff. That reassured me that we could figure out how to deal with this and to teach our son how to deal with it too. Thank you for sharing your knowledge and experience with us. This podcast is a game changer 25 years as a type one diabetic, and only now am I learning some of the basics, Scott brings useful information and presents it in digestible ways. Learning the Pre-Bolus doesn't just mean Bolus before you eat but means timing your insolence so that is active as the carbs become active, took me already from a decent 6.5 A one C down to a 5.6. In the past eight months. I've never met Scott But after listening to hundreds of episodes and joining him in his Facebook group, I consider him a friend. listening to this podcast and applying it has been the best thing I have done for my health since diagnosis. I genuinely hope that the diabetes Pro Tip series is valuable for you and your family. If it is find me in the private Facebook group and say hello. If you're enjoying the Juicebox Podcast, please share it with a friend, a neighbor, your physician or someone else who you know that might also benefit from the podcast. Thank you so much for listening. I'll be back very soon with another episode of The Juicebox Podcast.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#1024 Diabetes Pro Tip: Female Hormones
Scott and Jenny dive into the topic of hormones, specifically female hormones and how they affect those with diabetes. They discuss the challenges and changes that come with menstruation and provide insights on managing blood sugar levels throughout the month.
You can listen online to the entire series at DiabetesProTip.com or in your fav audio app.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - Radio Public, Amazon Alexa or wherever they get audio.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:03
Hello friends, and welcome to the diabetes Pro Tip series from the Juicebox Podcast. These episodes have been remastered for better sound quality by Rob at wrong way recording. When you need it done right, you choose wrong way, wrong way recording.com initially imagined by me as a 10 part series, the diabetes Pro Tip series has grown to 26 episodes. These episodes now exist in your audio player between Episode 1000 and episode 1025. They are also available online at diabetes pro tip.com, and juicebox podcast.com. This series features myself and Jennifer Smith. Jenny is a CD and a type one for over 35 years. This series was my attempt to bring together the management ideas found within the podcast in a way that would make it digestible and revisit double. It has been so incredibly popular that these 26 episodes are responsible for well over a half of a million downloads within the Juicebox Podcast. While you're listening please remember that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise, always consult a physician before making any changes to your healthcare plan or becoming bold with insulin. This episode of The Juicebox Podcast is sponsored by assenza diabetes makers of the contour next gen blood glucose meter and they have an amazing offer for you. Right now at my link only contour next one.com forward slash juicebox free meter you can get an absolutely free contour next gen starter kit that's contour next.com forward slash juice box free meter. while supplies last US residents only. The remastered diabetes Pro Tip series from the Juicebox Podcast is sponsored by touched by type one. See all of the good work they're doing for people living with type one diabetes at touched by type one.org and on their Instagram and Facebook pages. This show is sponsored today by the glucagon that my daughter carries G voc hypo Penn. Find out more at G voc glucagon.com. Forward slash juicebox. Okay, give me a testing. Hello. All right. You're there? I'm there. Okay. Yeah. All right. So I've spent, not my whole life, you know, but the last number of days and weeks looking into all of this, trying to get ready to make a pro tip episode about female hormones. And it's a very scary proposition. There's a lot going on. I'm not scared, scared, but I'm overwhelmed. And then the last kind of piece of it was that I went on to the Facebook page and said to people look, you know, throw out your questions for this episode. I want to be clear, I almost didn't think I needed their questions so that we could talk. I wanted to see if there was repetitive need, like you don't even like what are people like same questions over and over. And my goodness, I mean, it's kind of obvious, right? Like so. The questions ranged from like, just God, is there any rhyme or reason to this to? What about menopause? What about perimenopause, what about the time where my kid isn't getting their period yet, but it's starting to exhibit, you know, symptoms and having hormone fluctuations, talking about puberty and then pregnancy and then and then. Oh, is your head spinning post pregnancy? It's it's listen nature. God, I don't care what you think this is, there's gotta be a better way to do this. Someone, someone, this was an afterthought. Like, like someone at the end was like, oh, you know, here's what we'll do. We'll throw some eggs in here. And then you'll have to throw in some estrogen to get the eggs really roll and then one egg will come out. And if they don't get pregnant, the whole thing will just bleed out of their vagina. Perfect. Like, I don't know who what. Oh, my goodness. PCOS keeps coming up. Is that polycystic ovarian syndrome? PCOS? Yes. Now I know those words. So already, Jenny, I want you to tell me what you just said before we started recording about the inequities of diabetes management from men to men to women,
Jennifer Smith, CDE 4:48
or from an education standpoint to begin with. I mean, it was not something that was ever discussed in my presence, at least and I don't think my mom had outside of this Did conversations with my peds? No at all about hormones? Right. So I learned all of this as I was having this like, typical cycle, you know, that should happen after a certain point in the sort of teen years. And education today. It's focused as on diabetes, in general, right? Not on, if you're a woman with diabetes, versus if you're a man with diabetes, these are the differences that you will definitely see. So you're a woman with diabetes, you've got all the female hormones pumping in your body. Let's discuss diabetes from the angle of being a woman. Right? I mean, especially for my like, I wouldn't even say, when I start working with somebody, if they're from about the age 1011, all the way into, well, even the women they work with, into the perimenopause and menopause age, that's something in an initial visit, I always ask about, because it, even if it isn't yet visible, it will be at some point. And people need an idea that they need to like, see out into, if I see this, and this and this, I'm clearly not a crazy person. This is body function.
Scott Benner 6:21
Well, I guess, especially given that, you know, because we talk about things in general terms, like the cycles, 28 days, that's in general, it's not, it's not for everybody, and it might not be for you from month to month as well. So if you can imagine when you hear people talk about like diabetes, like just when I thought I had it, it changed or you know, those memes, there's meat is it memes? Oh, my God, I'm old, you know, where it's like Monday, two plus two is for Tuesday, two plus two is seven, you know, Wednesday, two plus two is zebra, like that kind of stuff. If that's already how diabetes feels to people in general, and then you put this on top. I mean, you really are kind of creating two different spinning layers of confusion that can impact each other, or show up on their own. And I don't know how you're supposed to make sense that I actually after going through all this, I have an idea I'll share at the end about how to get a handle on this. But I just don't know. Well, I guess to give people some context aren't in 17. So this is the depth of my understanding of this. My understanding of this is I'm married, and I've lived with a lady for a couple of decades. And, and my daughter has diabetes, and she's been getting her period for a while.
Jennifer Smith, CDE 7:43
And I bet you never paid as much attention as when it really was in reference to diabetes management.
Scott Benner 7:49
Only thing I used to pay attention to was, there's this what I call the nice day, there's like this. There's this literally one day a month, where my wife is a 1950s. Like, I'm making quotes perfect mom, wife, lover, like it's that day on that day, I feel taller and more handsome. Like, you know, like she is so incredibly
Jennifer Smith, CDE 8:18
kind of like Leave It to Beaver mom, sort of, at that age have an idea of what a Mom was
Scott Benner 8:23
right? Yeah. 100%. And I, I bask in that day, because the day that comes after it. I can't even look her in the eye. Because if I do something wrong, she's the different like, and then I know that the the event is coming in about five to seven days. Like that's how it works for
Jennifer Smith, CDE 8:44
us paid enough attention to actually like, I can tell you many, many spouses or partners are,
Scott Benner 8:51
I thought I was gonna die. I was defending my own life, you know. And so for years, that's the only way I ever thought about it. And then Arden starts to get her, you know, and then we're kind of rocking along and taking care of Arden's blood sugar. Like it ain't nothing some days, you know, it's just like, I do really have this all figured out. And then one day, she started getting her period. And it was all fine at first. It actually almost got more difficult at some junctures. But it was it was very structured. So I didn't have any trouble with it really. Right. And then all of a sudden, her periods got heavy. And you know, people listening will know that, you know, Arden went through a year or two of like us not understanding what was going on. She got anemic a number of times she had to have iron infusions. This was all ended up being because of her period. Right? Yeah. So Arden would get her period for like 11 days, like she'd have like 11 day long cycle, and then only a couple of day break before she started to bleed again. It was just really Nicholas, which led us to put her on birth control, hoping, like, you know that she wouldn't bleed to death, because she was, I mean, the impact on our life was insane. Sure, you know. And so first go round with the birth control they gave her it wasn't strong enough didn't really do anything. But they still asked you to be on it for 90 days before they consider changing it. So you, you struggled all this time you think you have an answer, and then 90 more days is struggling. And then they moved her up to another, I guess strength and that has, you know, straightened out her. Excuse me. Also, the first indication of that problem was nosebleeds. Oh, really bad out of nowhere nosebleeds. That only happened once a month. And it took us a while to figure it out. It was literally happening on a cycle. I never was able to connect it to her periods. But the minute she went on the birth control and the second round of birth control, and it straightened out her periods, the nosebleeds never happened again.
Jennifer Smith, CDE 11:11
That's really interesting. Well, and I mean, again, a symptom that if you're paying enough attention to your body, there are lots of things that your body is trying to tell you. Right, if we just pay attention to.
Scott Benner 11:24
And that's why I bring it up, honestly, because part of what I figured out, Jenny, part of what I figured out being a man who doesn't get a period, and a person who doesn't have diabetes, as I consider talking about this with you today was was that you kind of have to, you gotta kind of have to Jane Goodall it a little bit, right, like, you got to take notes and step back and see things and keep wondering what's happening until you can build some, some idea of like, I keep seeing this thing over and over again. And where does that fit on the calendar? And how does it work in relationship to, you know, bleeding or pain or insulin resistance, and then you sort of start making sense of it, you have to track your period. Yes, maybe for six months before you'll be able to wrap your head around it a little bit,
Jennifer Smith, CDE 12:14
especially if your cycle is not regular. I would say for women who, especially women who are considering maybe you're starting to track things and pay attention because you are planning a pregnancy, or maybe you're really trying to prevent a pregnancy. So then tracking things becomes just as important, right. But then along with the lines of even planning a pregnancy, the goal in diabetes is to have pretty optimized management prior to conception. So yes, I mean, you really should be tracking things for a fair amount of time, if you don't have them already nailed down because you've paid attention, right. And there are a number of really good period apps out there. I mean, there are some that are free that do just as well as some of the ones that have all the 1000s of bells and whistles for tracking everything else. But I think the ones that are the best actually have a place where you can keep notes. Because the tracking app that I like to use, I actually track month to month, how my insulin changes have looked this month. So I can go back last month, the month before and actually see, has it been consistent enough? Is it going along with what is normal for me. And that helps.
Scott Benner 13:29
Well, even very recently, in the last couple of months, Apple added a period tracker to their health app, which sounds interesting, robust, and it's free, and a lot of people use Apple phones. So I wanted to throw that out there.
Jennifer Smith, CDE 13:43
I didn't even know that was an option. So thanks.
Scott Benner 13:45
Yeah, so because Arden uses one that's third party, I don't even know what it's called now. But as I looked at people's questions, and I thought about Hold on a second. The gods are coming after me for talking about periods when I'm not a leader. That's right. As I thought about how I been figured, like, like step back and looked at what we had to go through to try to figure this out for Arden. And then I looked at people's questions. The real fear when you see fear is around the unknown portion of it. And all I could think over and over again, when I saw their questions like how do I know if it's going to fluctuate? When do I turn up my Basal insulin if I can't be sure when it's going to start? I kept thinking you're gonna have to track it, you're gonna have to pay attention you're gonna have to put like work in and I know that sucks because it feels like diabetes has already worked. But it really made me think about like, kind of what we talked about another pro tips, which is, you know, some upfront effort can save a lot of heartache, right over and over again,
Jennifer Smith, CDE 14:50
are a lot more micromanagement than you really should need to be doing.
Scott Benner 14:54
Yeah, yeah, you get stuck in that situation where you're constantly constantly constantly adjusting your blood sugar in the moment, which I'm a listen, I'm a fan of if your last to stay flexible, but in this situation where what was the number I saw the average woman's gonna have how many periods like 400. And something or it was like, oh, like
Jennifer Smith, CDE 15:17
hold on in a lifetime? Well, I guess if you expect an average age of a period starting at the age of 12, and there are 12 months in a year, right? So you would have, let's say, one cycle a year. And then the average time period of a cycle, completing would be about, let's say, age 12, all the way to maybe 55, let's say maybe even 60. And that's a good amount of time that you would be having cycle.
Scott Benner 15:52
I'm using your math 55 minus 12, is 43 times 12 months, is 516. So you go. So I'm saying, that's a lot of tracking. I'm saying put in put some, like real, like, it's gonna be honest effort, because you're gonna have to track you know, your insulin use every day. And, you know, just giving yourself I think, what helped me was just simple words. Difficult, easy. You know what I mean? Like, referring to my management, you know, meals were, what I expected, easier than I expected, harder than I expected. Yes, you know, my Basal seemed to work well, not Well, today, like just kind of keep it keep it like that, you make a little note for yourself. And I'll tell you to tracking your period is going to help you get better at taking care of your blood sugar, too, because you're gonna see all all around. Yeah, yes, you're gonna see all kinds of things that you didn't, didn't see before. To begin with,
Jennifer Smith, CDE 16:50
you're gonna learn a lot of things too, in that time of tracking for all of those other variables that we have to adjust around, right? Because I for one, know that my sensitivity, once I've gotten to about day three of my period, after that point, and until about ovulation is a really sensitive time. But it's more sensitive from day three to about like day seven ish. And in exercise, I have to be more aggressive and adjusting my insulin for exercise. Or I will go low. Despite my other tools and tweaks working outside of that, I will go low, if I don't adjust more than I normally would, is
Scott Benner 17:39
that a progesterone period in there.
Jennifer Smith, CDE 17:42
So you're essentially when you're looking at progesterone, that is typically like, peaking at certain points, right. And then there's also the luteinizing hormone, there's follicle stimulating hormone and there's estrogen, and you got a lot of hormones that are coming into play. So progesterone kind of starts to really kind of like, fall off. Essentially, once your period is started, it has really climbed in the time of you coming into potentially having a period. And part of the reason for that is in the anticipation that you in sort of that Avi LaTorre time period, have actually conceived, right? progesterone levels will stay high and continue to climb in pregnancy. One, you don't have conception happen, and you start to have your period, that level falls because there's no reason to have that elevated. I mean, again, other hormones at play here as well progesterone being one of them, but it doesn't need to remain where it was because you're not pregnant. Okay. So then it flexes right.
Scott Benner 18:58
And do do we let's try to think about this. Do we count the the beginning of the cycle is considered when the period starts right?
Jennifer Smith, CDE 19:09
Day one of your period is day one of your sites.
Scott Benner 19:14
In that moment, estrogen at that point is lower. Is that right? And then it starts to
Jennifer Smith, CDE 19:23
and then estrogen starts decline. Coming in to ovulation. And then in that next day is around ovulation and potential like conception. Again, progesterone is sort of like climbing into that time period, right? So, you know, again, all these fun hormones doing different things. I mean, if you even looked up a simple like just Google have a graph of like, what your hormones should look like. You can tell why. One Basal for 30 days in a row if you're a woman who has As a monthly cycle
Scott Benner 20:01
couldn't doesn't work yeah, it does. The remastered diabetes Pro Tip series is sponsored by assenza diabetes makers of the contour next gen blood glucose meter and they have a unique offer just for listeners of the Juicebox Podcast. If you're new to contour, you can get a free contour next gen starter kit by visiting this special link contour next one.com forward slash juice box free meter. When you use my link, you're going to get the same accurate meter that my daughter carries contour next one.com forward slash juicebox free meter head there right now and get yourself the starter kit. This free kit includes the contour next gen meter 10 test strips 10 lancets, a lancing device control solution and to carry case but most importantly, it includes an incredibly accurate and easy to use blood glucose meter. This contour meter has a bright light for nighttime viewing and easy to read screen. It fits well on your hand and features Second Chance sampling which can help you to avoid wasting strips. Every one of you has a blood glucose meter, you deserve an accurate one contour next one.com forward slash juice box free meter to get your absolutely free contour next gen starter kit sent right to your door. When it's time to get more strips, you can use my link and save time and money buying your contour next products from the convenience of your home. It's completely possible that you will pay less out of pocket in cash for your contour strips than you're paying now, through your insurance. Contour next one.com forward slash juice box for E meter go get yourself a free starter kit. Touched by type one has the back of people living with type one diabetes. Take for instance, their D box program touched by type one knows firsthand the intricacies of living with type one diabetes, and so their team has created a D box which is a starter kit that provides important resources and supportive materials to individuals with diabetes. They want you to thrive. The D box is completely free and available to newly diagnosed people. All you have to do is go to touched by type one.org. Go to the program's tab and click on the box. While you're there check out all the other resources and programs available at touched by type one.org. Speaking of support, touched by type one.org is available in English and Spanish. Don't forget to find them on Facebook and Instagram too. You do not want to miss what touched by type one is doing. When you have diabetes and use insulin, low blood sugar can happen when you don't expect it. G voc hypo pen is a ready to use glucagon option that can treat very low blood sugar in adults and kids with diabetes ages two and above. Find out more go to G voc glucagon.com forward slash juicebox G voc shouldn't be used in patients with pheochromocytoma or insulinoma visit G voc glucagon.com/risk. You know what else I learned by digging into all this? Is that not that I wouldn't expect this because it's a physiological thing. But it's incredibly complicated what's happening. It's not just like, you know your your eighth grade health understanding of it, which you know, in my mind was an egg gets released you use it or you don't use it if you don't use it, you know the uterine lining and the egg come out in a period which I know is high level what it is. But the idea of like the ramp up right like the gosh, like you start talking about like follicles and like there's this process that's happening in there where your body's trying to locate the strongest egg to be released. It's not just like the next one on the assembly line. It's like it literally anyway, it's mind boggling. Even the TED talks on it are confusing. Even when even when nice girl sit in front of cameras in front of YouTube and trying to talk to you right in your eyes. You're like, I don't understand there's so much happening. But I think for the case of but for type one for using insulin is it is it as easy as saying that there's a time when you're bleeding. There's a time when you're ovulating. And there's a time when your body is trying to make your body a hospitable place for sperm to live. So that the process of fertilization can happen well, is that basically like there's I mean, that's
Jennifer Smith, CDE 24:45
basically the simplified and I think sort of along the same line of what you're getting at is if you if you're having a cycle whether you're on birth control with a cycle or you're not on birth control with a cycle you can expect the times of your period to show similarities for you in insulin need, right? One person may experience during this phase of, you know, hormone release, or this phase of their cycle, that they always have higher blood sugars now that they've been tracking things, they can say, Yes, I'm always getting higher here, one of the first places that that commonly starts is the fasting blood sugar, or the overnight blood sugar. For whatever reason, in the hormone dance of the human body, that's the first place that commonly women see things are running higher. And if you start to pay attention to your calendar, it will most likely coincide with, that's going to be somewhere about like, three to maybe seven days prior to your period, starting. Some women experience really short lived higher insulin needs. And whether they may have missed a slight nudge up maybe a week sooner. Most of them notice cash, the first, you know, day and maybe the two days before my period, I'm just high, I can't take enough insulin, I dump it all in and I still sit high. Well, next month, you know, if that's the case, and you start seeing higher blood sugars, and you do and you are maybe somebody who doesn't have a regular enough cycle, I would probably expect that this is what's probably on its way, as long as your site isn't bad, you know, all the other variables that it could possibly be?
Scott Benner 26:34
Yeah, so it's going to be incredibly important for you not to throw your hands up to the diabetes ferry and go, Oh, it's just diabetes, it's happening to me again, like, after it happens a couple of times, you gotta say, like Jenny saying, like, this is what happens. Whether or not I can tell you that it absolutely happens on day, I don't know 13 of my cycle or not, it becomes unimportant, like you, you sort of see, you know, it's not any different than, like, as you're talking about all this and about when people see higher blood sugars, like Arden has this too. But because my mindset is like more insulin pushback, don't let it happen. I can't see it. Sometimes I can tell you that we're bolusing more or that I'm running a higher Basal like profile. But I'm so accustomed to just being in the fight and fighting the fight. I sometimes don't think about why it's happening. I just
Jennifer Smith, CDE 27:27
right, you just adjust to get it back to target. Yeah. And I think that's, that's okay, as long as you're okay, adjusting that way. And if that works for you, then great. I think that more women especially again, those who are planning a potential pregnancy, are really wanting to track well enough because they're also in ensuring that their blood sugar's are really optimally managed for possible conception, and that thereafter, you know, so if you really do want more consistency, rather than saying, Well, I know how to do more insulin, I do it all the time. I just, you know, adjusted here and take more, they're just back here or whatever. But if you have even those that have a regular enough cycle, it could take some of the like headache out of the salon. Hi again, I know I need more, I'll take more. But gosh, is this happening regularly enough that I could actually figure out how much more do I need on an average monthly change time? Well, yeah, well, that is less guesswork in the moment that
Scott Benner 28:30
and the reason I brought it up is because the process of getting ready to make this episode with you made me realize I'm going to set up three different profiles for art and because she's gonna go to college. Yeah, I know what I need to do. Her blood sugar is gonna go up and she's gonna be like, this never used to happen before. You know, and she's, you know, not going to realize the thing she's missing is me. Texting, texting, you're going yo Bolus, what are you doing? Cuz because for people who don't like really understand, I know, it sounds like micromanaging to some like newer people, but for people listening to podcasts, I don't imagine it does. Like, I don't like to see a blood sugar over 140. And I act like like, you know how some people might act when your blood sugar is 300 is about how I start feeling at 140. I'm like, yo, what are we doing here? Because in my mind, I'm targeting back to AD in my mind 140 60 points too high. Like get it get it, but the the amount of insulin that it takes to get it has climbed since Arden's been on a birth control pill. So while yes, the birth control pill has regulated artists period, and she's not bleeding to death anymore. Her diabetes has gotten more difficult. Yeah, because and now if you go look at graphs about how it's like, Listen, what I know about birth control is probably not enough. But you're getting you're getting a pretty regulated amount of these hormones. Every day, and that birth control is literally tricking your body into not releasing an egg. I didn't realize that, that the bleed
Jennifer Smith, CDE 30:09
is keeping you on a one cycle of hormone akin to not needing
Scott Benner 30:14
ovulation. Yeah. Right. And so you're not nothing's happening. And obviously like the whole process isn't happening actually, I think what confuses people? Is that the bleeding that happens when you're off the hormones and you're on the the placebo placebos is not your period. It's got it's actually got a name. It's, uh, hold on a second. I have so many browser windows open. It's called withdrawal bleeding. Yeah, it's not your it's not the same thing.
Jennifer Smith, CDE 30:44
Never heard. I've never heard it called that before. Okay. Well,
Scott Benner 30:47
I was schooled, I recorded an episode about this with a different podcast. I'm going to be on a vagina podcast pretty soon. And that's funny. Oh, it was hilarious. And as I was being asked, I was like, why is this happening to me? But but but people who really take birth control? I don't mean, seriously is the wrong word. But but see it as stuff that maybe, you know, there are people who think you shouldn't do it. There are people who think you shouldn't tell people how to live their lives, there's a lot of consternation around birth control in some circles. And it's important for those people for you to know you're not actually getting your period when you're on birth control. So and I have to be honest, I don't want Arden to be on birth control, not because it's birth control, but because I don't want her to take anything she doesn't have to take right when she was going down. You know what I mean? Like, we were looking at her like, I guess this is it, like, you know, the money, the money we saved for college, we could buy a house with now or something? Well, and
Jennifer Smith, CDE 31:48
that's I mean, those there are, I think, really, there are really good reasons to utilize birth control all around, there are. But in a case like this, it's almost a necessity in order to get containment of something. Now, the other thing is, you know, is this something that's just, it's just the way that her body is gonna continue to work even into like adulthood, where she continued to have to have this level of birth control, you know, management, so that she doesn't have this problem. That question, you know, I had
Scott Benner 32:22
constantly like, when do we just like, stop at once and see what happens? You know what I mean? Like, but I don't understand any cause and effect reasons why using birth control for a while, would you know, quote, unquote, regulate things and then you wouldn't need it anymore. Were was this just a cycle of her life, and it was going to pass on its own. And we're never going to know, as long as she's on the birth control pill. Right? I keep saying, I keep thinking maybe, you know, a few months before college, maybe we like, would try to bail on at one time and see what happens. Because when you've done
Jennifer Smith, CDE 32:58
enough work already to know, I mean, she's used several different types of it. So you also have an idea of what works, what really did nothing good. And what does actually work because there are so many kinds of birth control that are available. And so many mixes of hormones that you could use, or some are single, single hormone, some are a mix of hormones, at different levels. They're taken different ways. I mean, there are
Scott Benner 33:32
at one point, our our pharmacy benefits changed her over to a generic things were going great. And then they change the generic and it went right back to where it was again. Oh, and then we had to swap her back to another one.
Jennifer Smith, CDE 33:45
So funny, right? I mean, if it was the same thing, only a generic what's different about it? Right?
Scott Benner 33:53
I have no idea. This is the this. Jenny in one way or another vaginas are the bane of my existence. They're, they're torturing me from different angles and different perspectives all the time. And, and on the Ardennes period has been, I mean, a roller coaster, it has not been fun for her for the people trying to help her. Well, and I
Jennifer Smith, CDE 34:17
think you see it from a perspective of you want the best for her. You want her to be healthy and enjoy life and everything's you see it really as a it's problematic, not from a physiologic standpoint is problematic and what it brings into the picture of her management, you know, you may have a very different look on it. If she didn't have diabetes.
Scott Benner 34:42
Yeah. Yeah, I guess I there's so much about I wouldn't even understand or pay attention to her. Right, Senator. So I, I'm basically having this conversation to tell people that I'm going to start doing what I think you should do, like I'm going to I'm going to set up my own tracking app. And I'm gonna track Arden's like insulin in bushes, Jenny's making a face because I don't,
Jennifer Smith, CDE 35:05
I'm pretty AMI like, you don't do things like
Scott Benner 35:10
she's gonna leave for college and either bleed to death or having a onesie and the aids like one of the other. Like, it's just one of the others gonna happen.
Jennifer Smith, CDE 35:18
So and typically I mean that is it's also another piece in the mix too because you brought a lot of things in that could be happening in periods that are mismanaged, right? Someone who has excessive bleeding can bring in a lot of other health risk problems that can also make the diabetes management piece even harder to figure out and manage around. So it's really important. I mean, on average, don't quote me, but I think I read at one point, like the average woman with a normal healthy cycle length, and not excessive bleeding, really only loses about a quarter cup of blood through the whole period, which is it's a tiny amount, right? I mean, if you know what a quarter cup measuring cup looks like. So I mean, if you're saying gosh, excessive, clearly excessive is like lots and lots that shouldn't be happening.
Scott Benner 36:14
Here's the one measuring stick for you. Arden's ferritin gets down to like the teens, she gets an infusion. They tested again, it pushes it into like the 130s. It gets pretty high when you get the infusion. Yeah, within three months of not being on the period. She was back in the teens again, teens again, yeah. So and just I mean, for people who don't know, anemia, low blood, low iron, whatever, you know, however you get to it. I mean, just can't hardly pick your head up. Oh, freezing feels horrible. You feel like you're dying, the whole time, shortness of breath. You can have heart palpitations. Like, it's not good. You know, you get like pain and you're like muscles and joints and like, it's, it's terrible. So Arden's gonna stay on this as long as she needs to. But yeah, but it's funny, while she was home, aren't chill at home, like when she was going to school from home, she needed less insulin. As soon as she went back to in person I knew her needs, were gonna go up again. And I did the thing, where I was bolusing too much and didn't adjust settings for a little while to like, it happens to everybody, it's sure doesn't not happen to me, because it's my podcast, like, you know, like, you're so used to managing one way. And then this big piece of your life changes. And you don't even realize it for some reason. And that just made me sad, or when I realized that thinking about this, because basically, on your period, your life is changing. Like every couple of weeks, you know, like there's this impact and an end, it might not happen to everybody, there are some women who will listen to this the go, oh, that doesn't happen to me, or, you know, just like, Oh, my God, well, in fact,
Jennifer Smith, CDE 37:59
I've got, you know, some women that I've worked with, you know, even outside of like preconception planning, just in terms of diabetes management. And obviously, the cycle is a piece that we talk through and talk about, and some women who actually have the higher blood sugar levels during their period. Not before. It's more really an onset, while they're actually having their period, which is not the typical of what I've seen, but again, I've heard it enough that it's also not odd or rare,
Scott Benner 38:30
ya know, in the questions that I sent to you that that I found online, it was almost like people were like, hey, during these days here, my blood sugar is incredibly easy. And then somebody would come along and say, well, in those same exact days, my blood sugar is incredibly difficult. And yeah, I'm sure if we could, you know, Doctor House, every person in the world you might find, but I don't think that's gonna I used to love that show. I mean, right. sarcoidosis usually. Right? And I don't even know what that means. But, but so did you see anything in these questions that you definitely wanted to go over?
Jennifer Smith, CDE 39:08
I was just gonna go back to because
Scott Benner 39:14
because at some point, too, there were a number of questions about menopause, too. And some women are asking about what about when they take hormone replacement? Is it going to happen then, and I don't know, but it seems like the same as taking birth control to me, right your your address, you're adding hormones to your daily intake. If you're living with diabetes, or the caregiver of someone who is and you're looking for an online community of supportive people who understand, check out the Juicebox Podcast, private Facebook group Juicebox Podcast, type one diabetes. There are over 41,000 active members and we add 300 new members every week. There is a conversation how happening right now, that would interest you, inform you, or give you the opportunity to share something that you've learned Juicebox Podcast, type one diabetes on Facebook. And it's not just for type ones, any kind of diabetes, any way you're connected to it, you are invited to join this absolutely free and welcoming community.
Jennifer Smith, CDE 40:23
And hormone replacement therapy is usually for the most part centered around like the menopause kind of time perimenopause, menopause kind of time, it's supposed to help to ease much of the hormonal transition that's creating some of the symptoms, things like the hot flashes, and the energy swings and the insomnia and the, I guess, level of irritation, one woman may experience versus another. Right? So that's supposed to technically, even things out more. And it's a good question to actually ask, if you haven't, and you're considering or already taking the hormone replacement therapy, you know, asking your physician if they know anything, really about that piece in terms of what they should expect. My expectation would be that with the replacement therapy, if it's going well, and the dose is well managed, technically, you should have actually more stability than in how you're feeling, which should also bring more stability to your glucose management, right?
Scott Benner 41:35
Well, I guess while we're in this area, what about somebody who's had a hysterectomy? Did they lose all of those, that the cycle is just gone? Right? So that is, but it's all the hormones are all the hormones gone to?
Jennifer Smith, CDE 41:49
So although I mean, there's a good question, because quite honestly, you could have a partial or you could have a, like a total hysterectomy, right? I mean, so there are hormonal imbalances that can definitely happen with partial hysterectomy. It does, for the most part, from what I know cause less dramatic change in hormone levels than a full hysterectomy does. So in terms of that, you know, your hormones definitely shift because obviously, there's nothing there to cause that trend of hormones change, right, there's the period, right disappears. So, you know, overall, while there may be some initial management that needs to be done, I wouldn't expect that there would be as much I've worked with many women who've had hysterectomy. But I wouldn't expect that there to be as much fluctuation, as they probably usually had. I mean, when the menopause obviously is kind of similar in that when that happens, obviously, your ovaries stopped producing enough hormones to continue the menstrual cycle. Right? So if you had a hysterectomy, which includes removing the ovaries, you would then be essentially moved into sort of like a premature menopause kind of time. Right? So
Scott Benner 43:19
all right. Well, you know, if there's one person that asked such as a detailed question that I think Yeah, way they broke it down might be valuable for us. So her first question was, why does the body become more insulin resistant during different phases of the menstrual cycle? Just the laid out for people now that I think we haven't, but is the answer, just simply there's more hormones at different parts?
Jennifer Smith, CDE 43:43
Right. And so that's, you know, initially we're talking like what is the surge of the different hormones through the course of pregnancy or through the course of of a menstrual cycle? Right? So in terms of that rise up in insulin need, you know, there are a couple of points of time for different hormones, one of them progesterone, as its kind of rising, in terms of, are you going to find out you're pregnant? Or are you now you don't know if that you're pregnant, or you're not going to be pregnant, so you end up having a cycle. So then that climb in progesterone is again that typical time period before your cycle starts, that you would have insulin resistance creep into the picture. It may creep slowly, like seven days before you start to notice you've got that rise in blood sugar, okay, maybe you change up your overnight settings or, you know, whatever it might be. As you get closer to your expected first day of cycle, you're going to see a lot more resistance. I mean, many women find 20 to even 40% more insulin needed in that time period of climb in hormone, and then that most women experience the most significant and resistance the day before their cycle starts
Scott Benner 44:55
the day before the cycle starts which is the day yes leading
Jennifer Smith, CDE 44:59
day before there. Put yes there before their period starts, there's their bleeding happens, the event here, but in the event, there you go. So you know, that could be, you know, a visual point of saying, Well, I'm not crazy, I didn't need to change my pump site and change to new insulin or at nothing was really wrong, I see that this is the pattern and this is what's always happening. So how high did my blood sugars go? How much more insulin did it look like I continually used in the past two or even three months, so that you can expect it now. And you can make a, I guess, a wiser shift in your insulin rather than just sort of like completely guessing. Right? Oh, I'm gonna take three units today because clearly two and a half yesterday didn't work well. Okay. But if you have some back knowledge, you can say okay, this is definitely how much more I needed. And I can adjust better here. Now
Scott Benner 45:53
do you know there are months that Arden's period doesn't begin on the first day of the placebo, it happens sooner. Which doesn't make any sense at all. She's definitely kooky in her belly, like like, something's, something's going like when that happens. So two days ago, I saw as much resistance from her as I as I had in the month. And I said to her, like something, you're gonna get your period. Soon she goes, I have like four pills left. And I was like, okay, so then yesterday, dude all day, like we had to cut her insulin back. Crazy yesterday. So when she got home from school, I was like, did you get your period? Because No, I still have a couple of days left. But her body acted like her period started yesterday starting. And I'm like, I wonder if the bleeding is now adjusting back to where it's supposed to be. I also wonder, sometimes like Kelly's, you know, still still matched traits, my wife still fertile.
Jennifer Smith, CDE 46:52
That's a good thing. The longer you actually have your cycle, the healthier for you. It reduces a lot of the risk of female related cancers. Because the longer you have your cycle, and the length of the cycle matters, too. Not that this is diabetes specific, but it's a piece in the mix of if you've bad cycle, regular cycle, and the longer you have it in the life the better for you.
Scott Benner 47:16
Yeah, well, that's good news. But what I was wondering was is you know how you kind of sync up to people? Yeah, like I I've often wondered if Arden and Kelly even being near each other is messing with Arden.
Jennifer Smith, CDE 47:29
Very likely because in college, I had three other roommates. And at that point, we we all within a week had our periods at the same time. Yeah, like it was not a house
Scott Benner 47:48
or buying a bigger trash can. Okay, so this person's next question was, do insulin needs change? Only when premenstrual or does it happen around ovulation as well? I think yes. We've pretty much gone over that. Right.
Jennifer Smith, CDE 48:03
Yeah. And ovulation. For some, just in clarification, some women notice more significant insulin resistance around ovulation than they do in the pre cycle or like period start time. And it's often much shorter lived have a is a swing up, more noticeable rise. Post meals often tend to be impacted more if you're going to notice a change around ovulation. But it's only going to be like 24 to 72 ish hours around that ovulation that you're going to notice such significant resistance. So again, we've got this like roller coaster of hormones going on. Making people feel crazy.
Scott Benner 48:48
So I watched a video about how to know when you're ovulating getting ready for this. And there's a lot that you can watch. Oh, geez, I learned a lot about discharge and cervix ripening and feeling sexual and that it sometimes happens and sometimes, to some people doesn't happen to others. Some people get many of the symptoms, some people get fewer Nan. Yeah, you know, I love it when something spelled out to you like this. Here's what could happen unless it doesn't. Or maybe it won't, but K could and you're like this is not helpful, like, say something concrete or stop making videos. But it was really, I don't know, it was interesting. Anyway,
Jennifer Smith, CDE 49:32
there's a really good book I got actually years ago before we even plan to to start trying. It's called taking charge of your fertility. And it goes through it's really, I think, I think that it should be given to women in general. Because even if you never plan to have children, it gives you a really good idea of how the female body works. Yeah, and it Can, from just that standpoint make you feel less like? Like, I've always kind of hated when people are like, Ah, she's getting her period. Like, that's the reason for all of these mood swings and whatever. Well, it's I mean, that's, quite honestly, it could be true. I mean, it's somebody's meaning it in kind of like, not a very nice way. Yeah, but it is true that hormones change in flux a lot. But for you to know that as the person living with it, so you don't feel silly, about that's your body. It's supposed to be doing that.
Scott Benner 50:34
I'm 20% More a feminist than I was before I started paying attention to this. And I was already on the lady side. And so I mean, listen, I've never once been given medical direction that began with start with a clean finger. But I've heard those words a lot. Now, since I've been paying attention to this. And I just thought like poor girls. Like you don't even like Jesus and seeing it happen to my daughter, like firsthand. It really does. I mean, if you're, if you're not moved by it, I mean, I don't tease my daughter or my wife about like, Oh, your periods come and you're acting. But I tell you, when I was younger, I probably said it. But now that I've lived around it, I'm like, it's not. I mean, they should just say you should, you should be thanking them, not telling them. Yes, sir. You know,
Jennifer Smith, CDE 51:19
I know, to some degree, and I'm very happy that they have two boys. Because I'm like, You're gonna go to your dad. This is dad's department, go to your father,
Scott Benner 51:29
whatever he says it's not going to start with begin with a clean finger. I can tell you,
Jennifer Smith, CDE 51:33
nobody asked Bobby about that. And you
Scott Benner 51:35
You're lucky to because you're not going to ever be in this situation that Arden and Kelly are in where your periods are like, No, it just jerking you back and forth on timing. Right? You know what I mean? Right,
Jennifer Smith, CDE 51:45
right. Because I have, like I said, I have experienced that like in college. But I don't think at that point, I was even while I did a really good job of management as well as I could. That technology at that point was not, I mean, there was no CGM. I was still doing, you know, a lot of darn finger sticks a day to see where things were going. But I don't think I was as attuned to even wanting to pay attention to why something I was just like, I didn't even at that point. I was like, it looks like I just need a little bit more insight.
Scott Benner 52:22
I mean, maybe we're a decade into having the technology where you can break this stuff down a person's next question, I really want to thank them for this. And I don't have her name here, I apologize. Is you know, she brings up what are ways to track it, um, you can track it on a paper calendar, you can track it in an app, it's my intention to just like I said earlier to it a quick, easy way, maybe even colors would work, honestly, you know, green, yellow, red for insulin. I would track insulin needs I would track when the period starting, I would try to figure out as much about ovulation as I could. So you can kind of find that window in there about where it is. And I'll tell you to like it sucks, but you could track your mood. You could track your you know, your sexual desire. Like you can make all those little like clicks there. It's yeah, you don't I found thinking sucked for women the whole time, is that things that from an outsider's perspective seem like choice can be driven so harshly by hormones, which can make you feel like you're not doing things purposefully like it's your body doing it
Jennifer Smith, CDE 53:34
telling you to do you telling you to do Yeah,
Scott Benner 53:37
like, like, I would hate the idea of, I'm on a date. And I'm open to having sex tonight. Not because I want to have sex or because I like this person. But because my hormones are in a state where it's telling me
Jennifer Smith, CDE 53:50
they're kind of telling me to feel this way.
Scott Benner 53:53
Yeah, do this now. Because sperm will live in you for five days, and then we can get you fertilized and give you a good chance that, you know, of bringing this egg along. That's, I mean, it's kind of which brings
Jennifer Smith, CDE 54:07
in a lot of interesting fact, especially for the teenage. Right, yeah, where I mean, the majority of teenagers at this point are not considering conception. They're not they're beyond that, you know, for many reasons, but those are some of the things that your body is supposed to be telling you to do. Right? And you know, what's the reason? Well, eons ago. People were getting married when they were 1415 years ago old and having kids at that point, in fact, you know, if you weren't married by the time you were like 25 was like it was over.
Scott Benner 54:49
Window, right, because you were five years away from dying and probably it's um Well, I mean, I listen. It's beautiful, like you know, in a nature kind of natural ballistic weigh like, it's amazing. I just found myself feeling badly that you could be having feelings or thoughts that aren't the ones that you decided to have. But then I kind of brought it out larger. And I thought, when my iron was lower, I wasn't who I was. Right? I mean, we're all just, you know, some dialed up level of different chemicals and hormones and impacts and everything. And I, you know, I think that I hate to say that I think this episode could have been like, Hey, you should track your period, and then make better decisions about your insulin. Like, I really think that could have been the end of it.
Jennifer Smith, CDE 55:36
And then well, I think there's other I checked, there were a couple other questions in here that I think that do go. I mean, they they kind of go into, yes, that's the base, track your insulin, see what you need, and then make the decision on how to make your insulin delivery system. Do what you want it to do before you right, but there were a couple of questions. One of them was on MDI. Che change my diesel in a certain point of my cycle to deal with increased or decreased position resistance. And I should I also focus on adjusting my Bolus is I can say that, absolutely, you'll need to adjust at least your Basal insulin even on MDI. I mean, when I was MDI, and had caught on to the fact of needing more, based on what my blood sugar was doing, I knew that I needed a certain dose, that was three units, I still remember it was three units higher than my baseline dose for the time period of resistance that I needed. So you know, in terms of that, I could always adjust and unless something shifted and changed, you know, I would have maybe used a little bit more, or a little bit less. But overall, it was, it's funny that I still remember three units, where it was always what I use when I had my period. So yes, you could use more. And if your doctor isn't directing you to do that. Our doctors don't direct us to do many things that we end up doing. This is not advice or recommendation to do that, but discuss it with them. But it definitely bring in maybe some of the logs that you've kept and say, Hey, I'm noticing this, would you agree? I'm thinking I need this much more insulin, right? I mean, always check with somebody, obviously, if you feel that you need to boluses could they need to adjust? Absolutely, they could.
Scott Benner 57:32
Well, you know, I just did the math real quick, three units is only like point 125 an hour if you're on a on a Basal program for a pump. So right, it's but but, but it might have been significant for you. Do you remember what your basil was back then?
Jennifer Smith, CDE 57:48
Yeah, I do my basil. And overall was sitting at 12. And I needed 15.
Scott Benner 57:56
Okay, yes. Okay, so that makes a big jump. Even though it doesn't look like a big jump per hour. It is a big jump percentage wise, it was a
Jennifer Smith, CDE 58:03
big jump percentage wise, and it was a bit I mean, it looks like a big jump like Gosh, going from 12, all the way up to 15. Oh my gosh, like, that's a lot more insulin, right, especially when you talk about, like adjusting things. Okay, we're going to add one unit more of your Basal insulin. And we'll see how this manages things over the course of that whole 24 hour time period, right. The other one that I thought was good to focus on would be using algorithm driven pumping systems. As a female, the algorithm was not, it wasn't built for this to deal with hormones. It was not it wasn't built for hormones, it wasn't built for pregnancy, you can successfully use it. If you know how to manipulate settings, right? I I personally find that it's better for me to just adjust my baseline profile in my system. And then the months that I am more resistant on top of that, then a temporary adjustment up using a temporary Basal or an override or you know, whatever your adjustment is for the algorithm that you're using. I adjust up using that. Yeah.
Scott Benner 59:21
Is this whole conversation really similar to what you would have if you were talking about like, a teenage boy who's going through a lot of growth and hormone changes and stuff like that, like just it's just not on a cycle that you can see as well.
Jennifer Smith, CDE 59:38
Right? It's not on a cycle. That's as I mean, it doesn't seem to be from the team guys that I've worked with. It doesn't seem to be as cyclic. Yeah, predictable, right? It Right, right.
Scott Benner 59:50
This really is predictable, though, within reason,
Jennifer Smith, CDE 59:53
within reason. Yes. And I can even see if you're the person with the irregular sight Goal, let's say 25 days, one month, 29 days, another month back to 30 days and then back down to 25 days. Despite that, the things that you're seeing happen to your blood sugar in that time period will continue to happen for you. Yeah. Right. So even if your cycle length isn't about the same, if you start to see those in a time period that could be soon enough to be close enough to like an early cycle. Or maybe you're gone back beyond that, and you haven't seen changes yet. And up now I see changes.
Scott Benner 1:00:36
Okay, right. Yeah. Well, I was just thinking that you're talking about like variables and inside of variables inside of variables. You can, you know, you know, food, food cravings are not uncommon, right around hormone changes. So you could you could have forever thought, why is it sometimes I'm really good at nachos. And other times, I'm not really good at nachos. And maybe it's because once in a while you have nachos when you want them. And sometimes you want nachos? Because your hormones want them. And you're already in a situation, that's more difficult. And then you add in food, because what made me this was the question here is like, should I eat differently or exercise differently through different phases of my cycle? She's a great question. And it made me think, you know, I'm not into telling people how to eat. But there are definitely foods that are easier on you that take less insulin that you might want to try eating, while you are having an increased need for another reason, because now otherwise, you have to increase needs correct difficult food and your hormones at the same time. Right.
Jennifer Smith, CDE 1:01:39
And the hormones are driving a desire for things that otherwise you may have very, you may have very easy management around, right. You may love nachos, but your typical serving of nachos is appropriate and, and fine. And if it's a hormone driven time, you know, you might eat much more of your batch.
Scott Benner 1:02:00
You know, while we were adjusting Arden's birth control pills and getting it right, she couldn't stomach meat. She was not a vegetarian kind of person. And for a while she couldn't stomach meat. Like just get it away from me, she couldn't smell it, she definitely couldn't even think about eating it. And then as her as the pill, we found the right pill. And it got kind of like set in stone. Now that's come back a little bit.
Jennifer Smith, CDE 1:02:25
It must be something to do with the hormone levels in the birth control she's using because it's actually not uncommon for just thinking about hormones in general. Many women have some aversion to meet during pregnancy. Yeah, many women can't stomach red meat specifically. Okay. So I wonder if it's something hormonally similar. That was weird happening for her before it got regulated.
Scott Benner 1:02:52
I'm running around the house pointing to that my wife's like, that's crazy artists like you don't like Arden just thinks I pay too much attention to her. So she's like, stop paying, like caring. I tried to level up to the OB the OB is like, I don't know, I'm like, god dammit, I'm right about this. I was like, no one's watching these people more than me. You know what I mean? Like, um, they trust me, they'd all be dead without me, Jenny. Like, in one way or another? My wife, like, you know, like with the thyroid stuff, like, I'm the one who's kind of like, stepped back. Like you guys hear me talk about on the podcast, like being micro and macro. Like, on my family on macro. Like I step back, I look for big picture stuff. And I don't worry, but when I start seeing stuff over and over again, I don't know. It's just who I am. Like, I just, I don't know, I worry about people. So
Jennifer Smith, CDE 1:03:36
that's not a bad thing necessarily bad
Scott Benner 1:03:39
for me. It's great for them. You never noticed me worrying about myself. But
Jennifer Smith, CDE 1:03:46
was this I think this kind of me answers some of the question. I see and hear about age. Do you how old was Arden when she had her first cycle? Do you remember? Of course you remember?
Scott Benner 1:03:57
No? I don't know if I do. It was a little later than her friends. Okay, maybe,
Jennifer Smith, CDE 1:04:05
as was, as was I have a couple of questions here. And, you know, just relative to like, When should I expect this in my daughter? Honestly, could be as early as age 10. Wow. Honest, and it could be I mean, I was I was definitely late. I was definitely late in getting my cycle comparative to all of my friends. But I also think, in terms of that, my, my management wasn't then what it could have been if I were diagnosed in today's age, right. So I think that the management style that I had, at that point was not managing well enough to allow my body to actually be consistent enough to start my cycle at the time that it technically should have started. Yeah,
Scott Benner 1:04:57
this is Jenny's third attempt to let You all know to go back and listen to all of the pro tip episodes, you can do a really great job of getting your settings right understanding how to make changes for yourself how to Bolus for meals, how to keep high blood sugars from happening, like she is very artfully telling you, it's the ability and understanding is the is the firm foundation of living with diabetes. She's just, she's so nice about it when she says, Say what Jenny saying, y'all aren't doing a good enough job. You gotta get in there and try a little harder. You know, it's funny, I think Arden was 14 Having just turned 15. And I don't remember the date. I remember the situation we we, along with a number of her friends, were on our way to go swimming. And this was Arden's first time swimming with a period. And a bunch of little girls disappeared upstairs in my house, and came back 20 minutes later, disheveled, sweaty, rocked, and the end the one girl just we couldn't get it in. And apparently, this is apparently at one point like a mechanic
Jennifer Smith, CDE 1:06:08
and how funny that they actually like. I mean, they felt comfortable enough with you that they actually announced it to like a guy. I would have been like mortified, telling my dad something.
Scott Benner 1:06:19
No, he just described to me as Arden was a car on a lift, and the girls took turns trying to change oil and couldn't figure out how to do it. Oh, that's interesting. So that's about what happens around here usually. And well. Actually, I gotta say that's not usual. But but it didn't work out. And so I'm thinking it was the end of her 14 right around her 15th birthday. If I'm paying from guessing right? If I'm wrong about that, then it's no, it's not 1516. She's been at this for a while. I think it's 14 to 15. But yeah, like this could like you could have kids getting their periods, all kinds of crazy, just like what I used to hear like the hormones and cow's milk or making girls develop sooner or something like I don't know if any of that's true. But you know, there are girls walking around sometimes where you're like, are they 20 or 10? Or like what you can't tell?
Jennifer Smith, CDE 1:07:09
Yeah, I know. Yeah. The I mean, I think that that's like a rabbit hole of we could dive in there. But it would be a long, long discussion.
Scott Benner 1:07:18
We should make euphemisms about holes while we're talking about periods. So. So I mean, do you think I'd see it? Do you think there's anything else? Like? I mean, I feel like this is a good conversation. I mean, perimenopause, people are asking about different kinds of birth controls, like there are non hormonal birth control, like, ways, right. So, I mean, there's, I'll tell you, more than two people asked about Plan B. Whether it has an app, whether or not that would have an impact on blood sugar's and I wasn't able to find that out. You know, I
Jennifer Smith, CDE 1:07:55
that is a really good one. I can actually ask my my old mayor, may MFM, I can actually ask them if they have any reference to that having worked with enough women with type one? I don't know. I mean, the goal of that, obviously, is to not conceive. So it has some level of hormone shift to prevent pregnancy,
Scott Benner 1:08:22
you would think it's an overwhelming of hormones to kind of stop
Jennifer Smith, CDE 1:08:26
whether it has an impact on blood sugar? I don't know. It's a really good question. I
Scott Benner 1:08:32
don't know enough about how that works. How about IUDs? Do they impact blood sugars? That I'm sure you've seen in practice? Right?
Jennifer Smith, CDE 1:08:40
Right, those more they seem smoother than other birth control methods. From what I have seen. So do they have impact? They probably have an impact in terms of initially having one and then the outcome of what now your sort of monthly cycle, if there is still one remaining. What does that look like? Do you see any shifts? I've I've seen women who don't actually have any visible cycle whatsoever, right? Who have noticed a minor shift that appears to be cyclic, but most of them tell me that they don't even adjust around it. They just end up taking like a little more corrective at the next mealtime the correction seems to work well enough, kind of gets them, you know, back to where they want to be. And they never make any shifts in their insulin at all.
Scott Benner 1:09:37
I have to say that Ardens OB was pushing, pushing, she wasn't pushing. She was saying if we don't find some stability with blood with birth control pills, she wanted Arden to consider an IUD now Arden's like a little young, like we walked out to shoot, like the first thing she said to me was like, I'm not doing that. And I was like, gotcha, but it was, you know, she's like, you know, in the future, we might have to keep this in mind. Yeah, I don't I, you know, that is another thing I don't know much about. But you look like you have something you want to say, what did you find? No, I
Jennifer Smith, CDE 1:10:06
was actually just looking up a little bit about whether I could find anything on the plan B and blood sugar specific to type one, but I don't really see anything at all that documents that
Scott Benner 1:10:21
Okay, how about so is PCOS somehow related to diabetes? And or no? Like, why do you use it just because I only apparently at this point in my life, I only talk to people who have diabetes that I I start thinking things are more common or
Jennifer Smith, CDE 1:10:37
right PCOS is more common in those with other metabolic shifts that include insulin resistance and PCOS can bring more resistance into the picture, right? Other metabolic things being have more difficulty with weight management, they have higher cholesterol levels may already have higher blood pressure, despite potentially doing all of the healthy lifestyle things to manage those. But PCOS is more common with the type two. But interesting. In the past, I would say five years, I have had more women more normal, like healthy body weight and healthy lifestyle, who have actually been diagnosed with PCOS. And part of the part of the reasoning in terms of like sending them to their back to their doctor to say, hey, I don't understand I am doing everything in the picture of management. And I need so much insulin to keep things where they are. Something else has to be in the picture. So a mine is always Why don't we look for PCOS? Because if that is in the picture, one of the long term even in women without diabetes with PCOS medication that's very common and uses Metformin. Okay, it helps to dial down the resistance. And from the PCOS level, it helps with some of that cystic nature in the ovaries, and it helps with evening some of that out in terms of hormones and everything. So Metformin is definitely a heavily used additional medication that could be, you know, beneficial.
Scott Benner 1:12:35
Yeah, somebody mentioned Metformin. In in one of those, I forget where it was. I didn't bring that question over for some reason, because they were like, because they were talking about like, can I could I just use Metformin during certain times of resistance around like, you can't stop and start it right?
Jennifer Smith, CDE 1:12:56
That's no, that's not the way that Metformin is meant, you know, if you're gonna use it, we started a low dose, evaluate tolerance. I mean, it's one of the older oral medications it typically for most people is well tolerated after you get over some initial like first week or so of like, some stomach upset. And as long as you're tolerating it, it increases to like more of a therapeutic level. And then you continue use of it, you don't start stop it use
Scott Benner 1:13:23
the Advil during one section of your I only, I brought it up here, because if somebody was thinking maybe somebody else was thinking, I did not think that was a good idea. So, okay. I don't know like, there's this moment where I go, Are we good Johnny that I do we do it or?
Jennifer Smith, CDE 1:13:42
Yeah, I think, you know, I was looking at more of the questions just to make sure that P A mean in terms of talking specific like cycle, I think yes. I mean, I think discussion around things like menopause and that kind of stuff are it's such a transitory time in terms of
Scott Benner 1:14:10
that ever, right? Like menopause can go on for years. It can
Jennifer Smith, CDE 1:14:15
go on from very long time. Absolutely. I mean, and that's really perimenopause. Right. Once you're fully in menopause, you have no longer have to cycle for a year's time. Right. Then are you are menopausal. perimenopause starts with many women notice a shift in their cycle. Let's say you have had a regular 30 day cycle consistently, you kind of getting into the age of and what age in general about 50 ish, but women with diabetes have from research sort of proven to start earlier than the typical like age of 50? Let's say. So, any shifts in your cycle, without any lifestyle changes or anything like that, you know, now you're having 25 day, the next month, It's 30 day, this month, you have three days and a really light cycle next month. It's really, really heavy and painful and it's just not your typical. It could be very likely that perimenopause is kind of in the picture. And there aren't. I mean, many women would say, Well, can I, you know, get hormone testing levels done to see in this point of perimenopause, it's not typically recommended. It really isn't until menopause, that they would recommend doing testing of hormones to actually sort of prove the case that they have come to a level without a cycle, you're no longer ovulating. And some women actually haven't done the testing to make sure that they're actually not ovulating. From just like a sexual standpoint, they're just ensuring that they can't get pregnant any longer.
Scott Benner 1:15:53
Yeah. Okay. That's how you imagined having a baby when you're 50. I'd be so tough.
Jennifer Smith, CDE 1:15:58
I personally, I can't I,
Scott Benner 1:16:01
I would be so tired. That's all I can think of.
Jennifer Smith, CDE 1:16:04
Yes, I mean, from an age No, I can't.
Scott Benner 1:16:08
So no, my God. Last night, Kelly was like, can you imagine if we had had three kids? And one of them was just a couple years younger than Arden. Wouldn't that be nice? And I was like, No, I don't think so. It's it's 930. And I want to go to bed. How would that be a good thing? That child would end up being feral? I'd be like, just try not to die. I don't know if I'd have the energy to take care of it. I really don't. I don't. I mean, good for you. If you do. I don't think I could. That it were good. I think that's it. You should be good. All right. So thanks. On the whole that's everything.
Jennifer Smith, CDE 1:16:42
Probably not everything, but you know,
Scott Benner 1:16:44
is it. Alright, cool. All right. Awesome, Jenny. I really appreciate this. Thank you so much. Thank
Jennifer Smith, CDE 1:16:51
you. Yeah, you're very welcome.
Scott Benner 1:16:53
I want to thank assenza diabetes for sponsoring the remastered diabetes Pro Tip series. Don't forget you can get a free contour next gen starter kit at contour next one.com forward slash juice box for E meter, while supplies last US residents only. If you're enjoying the remastered episodes of the diabetes Pro Tip series from the Juicebox Podcast you have touched by type one to thank touched by type one.org is a proud sponsor of the remastering of the diabetes Pro Tip series. Learn more about them at touched by type one.org. A huge thank you to one of today's sponsors G voc glucagon, find out more about Chivo Capo pen at G Vogue glucagon.com Ford slash juicebox. you spell that GVOKEGLUC AG o n.com Ford slash juice box. Jenny Smith holds a bachelor's degree in Human Nutrition and biology from the University of Wisconsin. She's a registered and licensed dietitian, a certified diabetes educator and a certified trainer on most makes and models of insulin pumps and continuous glucose monitoring systems. She's also had type one diabetes for over 35 years, and she works at integrated diabetes.com If you're interested in hiring Jenny, you can learn more about her at that link. I hope you enjoyed this episode. Now listen, there's 26 episodes in this series. You might not know what each of them are. I'm going to tell you now. Episode 1000 is called newly diagnosed are starting over episode 1001. All about MDI 1002 all about insulin 1003 is called Pre-Bolus Episode 1004 Temp Basal 1005 Insulin pumping 1006 mastering a CGM 1007 Bumping nudge 1008 The perfect Bolus 1009 variables 1010 setting Basal insulin 1011 Exercise 1012 fat and protein 1013 Insulin injury and surgery 1014 glucagon and low Beegees in Episode 1015 Jenny and I talked about emergency room protocols in 1016 long term health 1017 Bumping nudge part two in Episode 1008 teen pregnancy 1019 explaining type one 1020 glycemic index and load 1021 postpartum 1022 weight loss 1023 Honeymoon 1024 female hormones and in Episode 1025 We talked about transitioning from MDI to pumping. Before I go I'd like to share two reviews with you of the diabetes Pro Tip series, one from an adult and one from a caregiver. I learned so much from the pro tips series when our son was diagnosed last summer, it really helped get me through those first few very tough weeks. It wasn't just your explanations of how it all works, which were way better than anything our diabetes educator told us. But something about the way you and Jenny presented everything, even the scary stuff. That reassured me that we could figure out how to deal with us and to teach our son how to deal with it too. Thank you for sharing your knowledge and experience with us. This podcast is a game changer 25 years as a type one diabetic, and only now am I learning some of the basics, Scott brings useful information and presents it in digestible ways. Learning the Pre-Bolus doesn't just mean Bolus before you eat but means timing your insulin so that is active as the carbs become active, took me already from a decent 6.5 A one C down to a 5.6. In the past eight months. I've never met Scott But after listening to hundreds of episodes and joining him in his Facebook group, I consider him a friend. listening to this podcast and applying it has been the best thing I have done for my health since diagnosis. I genuinely hope that the diabetes Pro Tip series is valuable for you and your family. If it is find me in the private Facebook group and say hello. If you're enjoying the Juicebox Podcast, please share it with a friend, a neighbor, your physician or someone else who you know that might also benefit from the podcast. Thank you so much for listening. I'll be back very soon with another episode of The Juicebox Podcast.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!