#1351 Caregiver Burnout: Experiencing Chronic Sorrow
A three part series about caregiver burnout with Erika Forsyth.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Hello friends and welcome back to another episode of The juicebox Podcast.
Today. Erica Forsyth is back, and we're going to do a short series on caregiver burnout, this is part one. Please don't forget that nothing you hear on the juicebox podcast should be considered advice medical or otherwise, always consult a physician before making any changes to your healthcare plan or becoming bold with insulin to save 40% off of your entire order@cozyearth.com All you have to do is use the offer code juicebox at checkout. That's juicebox at checkout to save 40% at cozy earth.com if you are the caregiver of someone with type one diabetes or have type one yourself, please go to T 1d exchange.org/juicebox and complete the survey. This should take you about 10 minutes, and will really help type one diabetes research. You can help right from your house at T 1d exchange.org/juicebox, Erica Forsyth is a type one herself and a therapist for families with type one diabetes to learn more about her. Go to Erica forsyth.com. Eric, can see you in person or virtually in California and virtually in Oregon, Utah, Vermont and Florida.
This episode of The juicebox podcast is sponsored by ag one drink. Ag one.com/juicebox when you use my link and place your first order, you're going to get a welcome kit, a year supply of vitamin D and five free travel packs. Can you name the only CGM that has only one sensor placement and one warm up period every year? Think about it. It doesn't matter if you can, I can. Eversense 365 is sponsoring this episode of The juicebox podcast, Eversense, cgm.com/juicebox, a year's a long time. The episode you're about to listen to is sponsored by OmniPod and the OmniPod five. Learn more at omnipod.com/juicebox use my links to support the show. Erica. How are you?
Erika Forsyth, MFT, LMFT 2:21
I'm great. Thank you. How are you? You're
Scott Benner 2:25
great, but your power just went out. We just got you back in time to record.
Erika Forsyth, MFT, LMFT 2:28
Yes, good thing.
Scott Benner 2:30
Things are happening now. It's Friday. Day's almost over for me. For you just getting started, but nevertheless, I get a note from you pretty recently, after we saw each other for the first time, Eric and I got to meet in person at the touch by type one event in Orlando, and you had an experience there that gave you an idea for the podcast. Can you tell people about
Erika Forsyth, MFT, LMFT 2:53
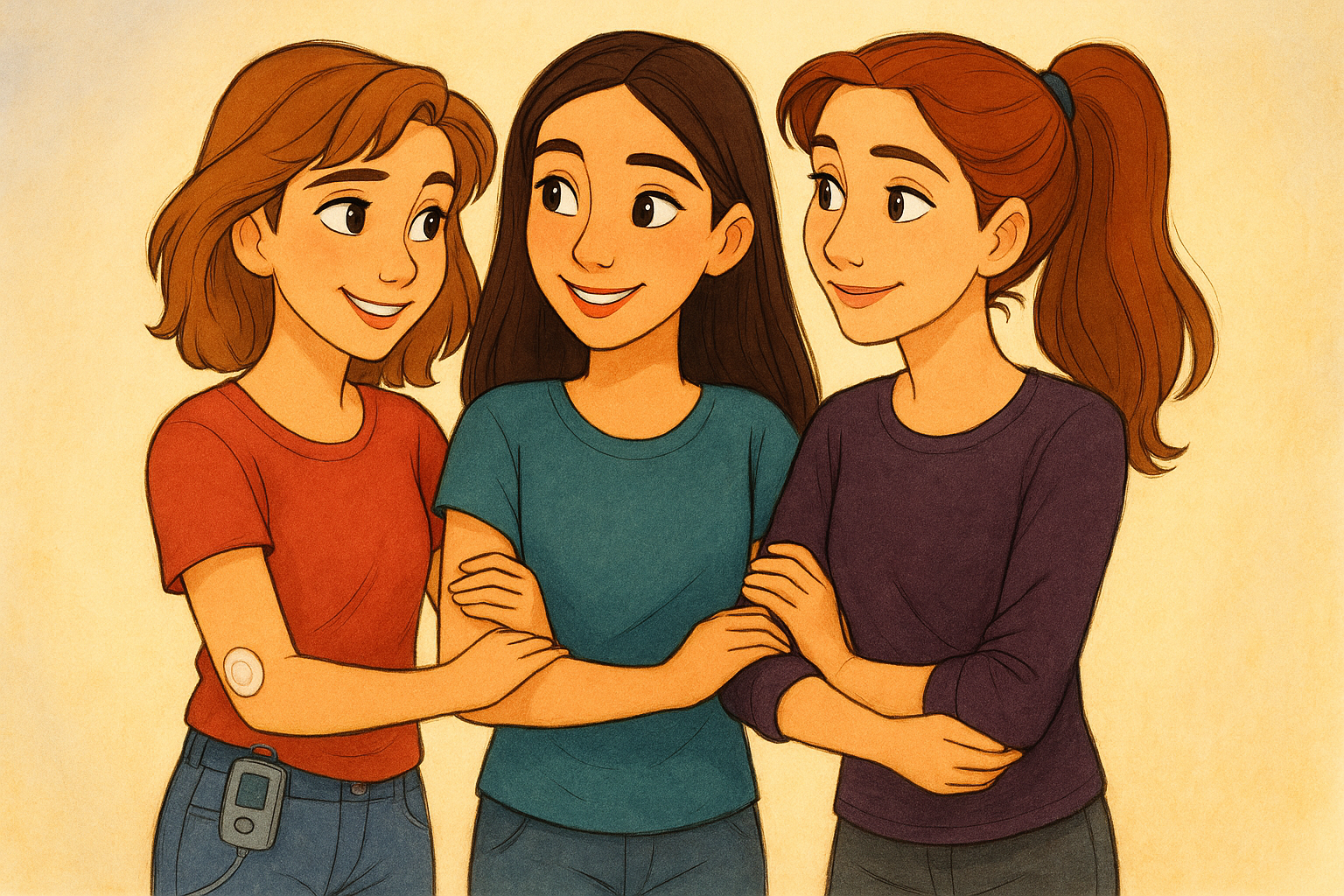
it? Yes. Well, first it was, it was such a joy to be at the conference and get to meet you in person, and Jenny in person, and all the wonderful people who run touch by type one. And just being there, I was there to speak in two different seminars, one for teens and one for caregivers, which was an absolute thrill to do. But also I was reminded how important it is to show up and do you know, participate in events like that, personally, because I was reminded of how great it is just to be in the room of hundreds of people, hearing the beep, seeing the things on our arms and being supported just in that way, physically. So I loved that.
Scott Benner 3:35
Do you feel like you got something out of it?
Erika Forsyth, MFT, LMFT 3:39
Yes, I think just, you know, even though I work in this field and I'm and support people living with type one and caregivers and with diabetes in general, I often don't do probably enough for my own benefit within in the type in the diabetes world. And so just the reminder that you're not alone is so powerful, yeah, and that, wow, looking in a room of people who know and understand what you do and how you live on a day to day basis is is so significant that it's almost kind of an intangible, unspeakable, and you know, it's hard to define, but You feel it? Yeah,
Scott Benner 4:20
I kind of found myself wishing I do this one thing. It's not really a talk, it's an hour with kids, and they range in ages, like, there's probably five, six year olds in there, up to, like, 14 or 15. But they don't let the parents in. There's somebody there from the organization and everything, but they want the kids to feel free to speak, and I just used it as an opportunity to let them find kind of commonality between each other. And then it opened them up. And I just started easily going around the room, like, What's it feel like when your blood sugar's high, and then, you know, what's it feel like when you're low? And what do you not like about this? Like, just real simple stuff. But you could see them a young kid, seriously, like a seven year old, looking at. 12 year old and go, wait, you have that thing happens to you too. That happens to me, you know. And then before you knew it, they were asking questions and making pronouncements about things they'd learned about their life and their health and everything. And I was like, wow, these kids, they know way more about this than I think people would give them credit for. It was really, it was eye opening for me, and it was helpful for them. Because, you know, on a basic level, one of the kids was like, Wait, why does my blood sugar get high when I'm at school? And then they all started talking about it. And then they realized about stress and anxiety, pressure, even just going in for a test, could make your blood sugar go up. It was wonderful. This little girl came up to me afterwards. I'm dying to interview her. I don't know who she is. I hope I can figure out who she is. But she came up to me with a notebook, and she asked me to sign it. And I was like, What? What are you? What are you doing here? Like, I don't think my my signature is not worth anything. She goes, No, I took all the notes of the stuff we talked about. I was hoping you would sign it. And she had pages of notes from the conversation. It's so cool. So that
Erika Forsyth, MFT, LMFT 5:58
is so great. It it creates a space for people to feel safe, to share what they're feeling. And I was so also impressed by the teens who were able to open up and just by one person saying something, and then they can say, Gosh, me too. Right? Like I feel that too. I've experienced that too, and that is the validating, normalizing experience that we all crave as humans, but in the diabetes world, that is so powerful. Just
Scott Benner 6:27
to let them say out loud, what feeling low felt like. And they all were like, oh, that's how I like just you could see their faces light up, like, wow, everyone feels this. It's not just me. It was a big deal, you know. So anyway, we were there. We had a great time. We met each other in person for the first time. It's awesome, yes, but you came away from the experience with an idea for the podcast. So what was that? Yes, so
Erika Forsyth, MFT, LMFT 6:50
I in the second seminar, I was, had the privilege to speak to caregivers, and I was, I was also blown away by the vulnerability that that the caregivers were able to share and experience in the in the group. And I thought in the session, it felt kind of a little bit like group therapy at times. And so I felt like, you know what? This might be powerful to bring that the talk that I gave at touch by type one here, and we can create it into a series awesome and essentially that the title and the focus was, you know, the caregiver burden. And I know we've talked about it before in various episodes together, but my hope is that by having kind of a really focused series on the caregiver burden, we would be able to create that experience for you here in the podcast, to validate your experience, to normalize it, and then to hopefully empower you with tools to not to maybe understand what's going on through your caregiver burden experience, and then actually give you some practical tools beyond deep breathing, which are, you know, It's always good and taking a walk, but beyond, beyond, kind of the the stereotypical coping strategies. So yes, well, how
Scott Benner 8:08
do you want to begin? I mean, this is your baby. So what do you think? Okay, well, I
Erika Forsyth, MFT, LMFT 8:13
think, just as we often do, kind of going to the definition starting with like, what is we talk about, the mental load of being a caregiver, we talk about the burden and that it's there's a there's a hardship and a loneliness that comes with it. And when, when we're talking about the caregiver burden, that kind of the true definition is the financial, physical, social, spiritual and emotional or psychological stressors that accompany caring for someone with chronic illness. So those are a lot of different factors that are really significant in life, that are impacted that I know you, you all experience as caregivers. And as a quick note, I also just want to say yes, I am I am a parent. I am a caregiver. My child, one of my my fourth graders, actually sick at home today. But I am not a caregiver to a child with type one. And so I was just even thinking about like, gosh, if she were, if she had type one, and I was trying to do this, I'd be worried about her ketones and all the other things, you know. So I certainly understand what it's like to live with type one for you know, now 34 years, but I don't. I will never pretend that I know what it's like to be in Scott's shoes or to be in any of your shoes as caregivers, but I do have the experience professionally in walking alongside you as a caregiver to a child with type one, and wanted to validate that, I
Scott Benner 9:40
take your point. It's nice of you to say, but it does bear pointing out that just taking care of a child is not the same as taking care of a child who has type one diabetes. It's just, it's different, and it even, like you said, a sick day. I can remember them in my head like ardent sick everything stops anything you had planned that day kind of over now. Well, you know, like, you're going to be super focused on this. You're going to be running around, hopefully everything goes the way you want it to. If it doesn't, am I going to call the doctor? Am I going to, you know, the first time, the first time you realize that your kid has ketones, but their blood sugar is 85 but they need insulin. Fries your mind. You're like, what am I supposed to do? 85 doesn't need insulin, but ketones need insulin. Yeah, it's not, it's not for the fatal heart, that's for sure. Sorry, yeah, today's episode of The juicebox podcast is sponsored by OmniPod. And before I tell you about OmniPod, the device, I'd like to tell you about OmniPod, the company. I approached OmniPod in 2015 and asked them to buy an ad on a podcast that I hadn't even begun to make yet because the podcast didn't have any listeners. All I could promise them was that I was going to try to help people living with type one diabetes, and that was enough for OmniPod. They bought their first ad, and I used that money to support myself while I was growing the juicebox podcast, you might even say that OmniPod is the firm foundation of the juicebox podcast, and it's actually the firm foundation of how my daughter manages her type one diabetes every day. Omnipod.com/juicebox whether you want the OmniPod five or the OmniPod dash. Using my link, let's OmniPod know what a good decision they made in 2015 and continue to make to this day. OmniPod is easy to use, easy to fill, easy to wear. And I know that because my daughter has been wearing one every day since she was four years old, and she will be 20 this year, there is not enough time in an ad for me to tell you everything that I know about OmniPod, but please take a look omnipod.com/juicebox I think OmniPod could be a good friend to you, just like it has been to my daughter and my family. This episode of The juicebox podcast is sponsored by Eversense 365 and just as the name says, it lasts for a full year, imagine for a second a CGM with just one sensor placement and one warm up period every year. Imagine a sensor that has exceptional accuracy over that year and is actually the most accurate CGM in the low range that you can get. What if I told you that this sensor had no risk of falling off or being knocked off? That may seem too good to be true, but I'm not even done telling you about it yet. The Eversense 365 has essentially no compression lows. It features incredibly gentle adhesive for its transmitter. You can take the transmitter off when you don't want to wear your CGM and put it right back on without having to waste a sensor or go through another warm up period. The app works with iOS and Android, even Apple Watch. You can manage your diabetes instead of your CGM with the Eversense 365 learn more and get started today at Eversense cgm.com/juicebox, one, year one CGM,
Erika Forsyth, MFT, LMFT 13:04
basically what we're going to do in in my preparation for the talk in the conference, I did some research, and I was curious to like what what research is out there, what tools from research are already out there to support caregivers for children with type one and coincidentally, there was research that was conducted and published just in March of 2024, and the title is called caregiver burden among parents of Children with type one diabetes, a qualitative scoping review. So these researchers, I'll just say them once here, so we won't repeat them. Azimi Johnson, Campbell and Monte Santi said, You know what we're going to do? We're going to look at all of the research that has ever been conducted on caregiver burden from 1995 to 2021, and they actually gathered, I think it was 1900 papers from there they, you know, had reduced it down through various filters of duplicates, but they and they wanted to ensure that every article identified all of those stressors that we that we discussed for caregiver burden. So they landed with 18 studies. And so from these 18 studies, they discovered six themes that are common and consistent through all of their research. Okay, so these themes are we're gonna what we're gonna do, and we'll start with the first one today, and then we'll break them down with each episode. So the six themes from all of these, from all the studies, are this. Number one, experiencing chronic sorrow. Number two, responsibility for glucose, highs and lows. Number three, managing T, 1d and night time. And sleep disturbances. Number four, making career sacrifices and choices to optimize T Wendy care. Number five, navigating social experiences post diagnosis and number six, isolation and stigma, and as a result of that, they're also everyone's endorsing, how much support they're finding from social support online. So I'm sure you all can relate, and all these things resonate. So from these six themes, we're going to discuss them as barriers to self care. Like, why is it we're going to look at the question, why is it so hard to create time, to take time for yourself as a caregiver? And so through that lens, we're going to discuss these themes as barriers to self care. And then after each barrier, we're going to discuss some tools, okay? That will help you find ways to, you know, to understand and then to make some changes, however big or small, to taking care of yourself. How does that
Scott Benner 16:11
sound? That sounds like a perfect plan. Excellent. Okay, yeah. Okay.
Erika Forsyth, MFT, LMFT 16:15
So what I'm going to do, so the for burden one experiencing chronic sorrow, I'm going to read a quote that is, this is all taken from this the research. Okay, so experiencing chronic sorrow as time goes by. There is not the same drama about the whole thing, but I still feel the despair and the loneliness when I let it come to me.
Scott Benner 16:39
I know that feeling right? You hold it, you kind of hold it all at bay on the other side of a wall somewhere, right? Because if you keep experiencing it over and over again, it just it crushes you. Yes,
Erika Forsyth, MFT, LMFT 16:51
yeah. So we know, and all across all the studies, and I know all the people you've interviewed and the people they work with, there's that initial sense of shock that we've talked about, that you've experienced, the anxiety, maybe guilt. What you know, could I have done anything to prevent this despair, the sense of overwhelm, feeling sad, angry, a lot of self doubt, as you're trying to learn so you're feeling all of that intense sadness, anger, grief, but then you also are forced to have to learn and educate, and so that is that initial shock and loss is very intense. Yeah, it's the the loss
Scott Benner 17:32
piece too. You think you're not sure what your life was supposed to be, but you're positive it's not going to be that. Now, you know what I mean, like the loss of possibility, maybe, or freedom? I don't know, but it feels like I've never, not heard anyone talk about it that way. You know,
Erika Forsyth, MFT, LMFT 17:49
I think I shared this in the in the talk, but I'm also remembering that you once said no parent ever gives birth or adopts or however you have your child with the expectation that they're eventually going to be diagnosed with a chronic illness like you never. That's never in your you
Scott Benner 18:07
never, yeah, there's no planning for that. No matter how thoughtful of a person you are, you never sit around going, oh my god, we're pregnant. You know what'll probably happen? You know, in year 17, they'll have a car accident, and like you don't. That's not how it works, you know. So you have all this hope and diabetes, somehow it doesn't just ding the hope, it dashes it completely. It just feels like it just removes all of it, and then you have to build back and realize that's not actually the case. But boy, it feels like that at first, yes,
Erika Forsyth, MFT, LMFT 18:40
and go ahead. No,
Scott Benner 18:42
I just upset. I'm already upset.
Erika Forsyth, MFT, LMFT 18:45
I don't want to be upset. And I think that's actually a good point. You know, as you are listening to this episode in this series, be mindful of maybe where you are in the day. And if it does, if this does trigger or evoke emotions. I do encourage you to let them come out, if you are able to, if you can give yourself that time and space in this kind of chronic sorrow. So we have this initial shock grief and loss. With that is the disenfranchised grief that I'm pretty sure we've talked about before, but I think it's important to go back to that disenfranchised grief kind of the definition is, it's also known as hidden grief or sorrow, and it can refer to any grief that goes unacknowledged or unvalidated by social norms or by your family or your friends, this kind of grief is often minimized or not understood by others, which makes it particularly hard to process and work through. And this type of grief is really is so common with those you know with us in the in the diabetes community. Because there is so much misunderstanding, you're suffering, you're grieving, and you want people to know, but you don't quite know how to communicate. That part, there's like this duality, right? But you and even when you try to communicate it, they don't quite ever get it. And then that leads you to maybe even feeling worse and more alone. And
Scott Benner 20:23
if you're caught in that, in that vortex, when you see a late night comedian, for example, like use diabetes as a, you know, in a joke line, or something like that, yes, that's where you get that feeling of like being minimized, dismissed, or just that unrecognized social problem. So that's where that comes from. Like, I need people to understand what this is, so that What the Why do I need them to understand so I can get past this part from me.
Erika Forsyth, MFT, LMFT 20:51
We want people to understand because that will decrease that feeling of isolation, okay? And but then we realized it's really hard to fully understand this severity and intensity of what it's like to care give and
Scott Benner 21:09
so you're isolated, and you feel helpless to explain it to somebody. Yes, so if they just didn't make that joke, you'd feel less isolated, and the pressure to explain it might be alleviated as well.
Erika Forsyth, MFT, LMFT 21:23
Yes, yeah. I mean, which is why, consequently, the community is so important for us, right? Because we do have that immediate understanding and decrease isolation and but in anything that you're going through. You want people, you want support, and you want people to know, but when you find that it's challenging or that they just can't quite get it, you then come to this point of, okay, how am I going to move through this? Right? Like, am I going to keep trying? And I think that's that's part of your experiencing this chronic sorrow and chronic grief is that journey of, how do I share? How do I be vulnerable so that people know and I'm talking even like family members, how do people know that I'm struggling without feeling like I have to share with them all the nuances of T, 1d, or diabetes. How do I let them know where I'm at emotionally and be vulnerable enough so that they can support me that I mean, that that's and that's a journey, that's a personal journey. So just noticing that yes, so
Scott Benner 22:36
you can get emotional validation from them. Is that what you're looking at. Like, yes,
Erika Forsyth, MFT, LMFT 22:41
emotional validation, like, I'm here for you. Like, wow. And, and we'll, we'll get to these more, even more specific tools in the in the social episode. But this is part of it. Is kind of trying to figure out, what can I say that elicits the response I need, and when I'm not getting it? What do I do next? How do I educate without having to, like, re traumatize myself, or having to re educate everybody and get the support I need?
Scott Benner 23:07
Yeah, I mean, once people really see you and there's affirmation about like, who you are and what you're going through, once they understand it, my expectation would be that they could be empathetic about it, and that probably begins a new process for you, right? Like, once, once those other people like, oh, they get it. They understand. They're not fighting with me anymore. It's not like, Oh, you're always been so difficult. I actually heard somebody say that recently, just in a social media post, this girl who's in a wheelchair, I didn't even know what for, and she was saying that her family says, Oh, you're always so dramatic. I'm like, okay, like, you know what I mean? Like, and she's, you know, she's like, I'm just trying to share my situation with people, and they just see me as, like, looking for attention. She's like, I don't want this attention. I this is not something I wanted, but it's interesting that you can get that pushback. I'm just I'm so stuck on the idea that I need those other people to understand and to be empathetic, but I can't keep putting myself out over and over again to explain it to them. Is that where the rub comes?
Erika Forsyth, MFT, LMFT 24:16
Because, okay, we're and I'm talking this could be at any stage in in your child's diagnosis, when you are struggling and you're exhausted and you want people to know, because maybe it's not even a want. Maybe you just need people like you just you need the emotional support. You just need like, Hey, I don't understand what's going on, but I see that you're really struggling, and I'm here for you. And it might even be hard to communicate that much to somebody. And it's not necessarily like you want people to know that it's hard. But when someone, and this is what this is exactly what is disenfranchised grief is that because. Is they don't know how hard it is. You might not ever get that, yeah, extreme, that validation that you really are needing and wanting, and that is hard. That's hard, yeah,
Scott Benner 25:13
needing biologically too. I mean, we're humans, are we're social creatures, right? So as long as the as long as your social structure is about what people expect it to be, then they're accepting of you. But then once the thing becomes too different or scary or unknown, or even some people get I've seen people have unreasonable fear that someone's illness will make its way to them. I can't tell you who this is, but I know a person who has a story of getting into a pool with cancer and other people getting out of the pool like that. And so now you don't get that like that, just biological need fulfilled for connection, for society, and, you know, a social group.
Erika Forsyth, MFT, LMFT 25:55
Yeah, yes. I mean and that. And this is why, if this, if this is particularly challenging for you to work through, to process this, the grief and the isolation, that's why group therapy, that's right. Group conferences, you know, are so significant and powerful. Yeah, it's just, it's just hard, and it's not impossible to work through, right? But I think it's important to have a name to it. If that's what you're noticing and experiencing, is feeling the grief, but then also feeling isolated and alone in it, that that is the disenfranchised grief.
Scott Benner 26:33
Do you think some people get stuck there forever?
Unknown Speaker 26:37
Gosh, that's a possibly. Yeah, and
Scott Benner 26:40
then it affects everything. You don't realize that. That's when you start seeing yourself becoming, I don't know, I'm not sure what the word is, but cantankerous, and just always thinking everybody's coming for you. And that whole piece that I do see sometimes, right, where some people are just so backed into a corner that, you know, and by themselves, that everything that comes towards them feels like a thing they just have to run from or attack back at, even if it's not attacking them. Yeah, you've seen that with people with type one who are older, right?
Erika Forsyth, MFT, LMFT 27:12
Yes, there's, there's a reason why, right, that perhaps you're stuck in that space. And whether that's past trauma, and we'll, we're not going to go into all of that. We'll plug our resilience series here. Yeah, if you, if this is you're noticing, gosh, I feel like I'm really stuck in this spot. There's a reason why. But if you're noticing that you're filled with the constant sense of resentment and bitterness and just you're ang full of anger, again, that's really normal at times. So not just not to dismiss that or minimize that, but if you're feeling stuck, and you've been in that place for years and years and years and years and years, I would encourage you to get to do some analysis around that. And what is that? What is keeping you in that stuck place? It's hard, it's hard step to acknowledge and to take
Scott Benner 28:01
when we're doing these, I'm always worried that I'm taking you from where you want to be. So I know this is good, okay, all right.
Erika Forsyth, MFT, LMFT 28:07
Well, this is, you know, these are points that I would I made in my talk, but because I don't have you know, you as a sounding board, this will make it more, you know, probably rich, richer, hopefully. Well, I'm glad the last point before we get into the tools for the chronic grief is that we know, we all know that grief is not linear, even though we know there are the stages, the five stages of grief. And while we can get to the place of acceptance that will look different at different stages of your journey with diabetes as a caregiver, and perhaps you you get, you kind of get through, I like saying, get through. And kind of, instead of getting over the initial diagnosis, you kind of get through those initial stages of shock and loss. And then you might feel like, okay, we've got, we've got a rhythm going. And then go back to the six your child's sick for the first time, your child goes to the birthday party for the first time, or goes through puberty or off to call, you know, all these small and big changes where you feel like you're the comfort and the security and the safety that you felt in managing and managing the diabetes and also managing emotions felt very secure. And then you go through this first time, and then that can just that sometimes it can set you right back to where you were. And this is for all the reasons that we talked about in the in the resilience series as well.
Scott Benner 29:32
Oh, for sure, I see it online all the time. There's hallmarks in people's lives, and those who are struggling are, for sure, going to be set off by them the first time they have to go through TSA with diabetes.
Unknown Speaker 29:44
Oh yes, I
Scott Benner 29:45
have to get an x ray. I don't know what to do. Do I take this off? Is the company going to really charge me for another one? Like it just falls off a cliff, like the worry and the anger and everything and the fear birthday parties? I used to play softball with my buddies, and now I don't think I can. Anymore I ride a motorcycle. Can I still do that? Like it just every little thing that pops up for people, it just over and over again. It feels like it starts over. And when you're sharing online in an open space, it's also interesting to see what people decide to come in and be supportive and say, Oh, I've been through that. Here's my support. There are people who are like, Oh, that's a thing I've been worried about, and now they're hoping maybe they can learn about it before it actually happened to them. Then there is this interesting thing that happens sometimes, if a person's been in the community too long and they've seen too many people say, I don't know how to bolus for a cupcake at a birthday party, they can almost get frustrated. They'll lose sight of the fact that this person asking this question, this is the first time this has happened to them. They are not everybody else. It's interesting, you know what I mean? Because suddenly you get, you get measured with I already saw people ask this question three weeks ago, and I'm like, that's not how a Facebook group works. They didn't see that, you know, like, like, this is the this is the time when they're going through it. And it always brings me some measure of comfort, because I think the things that are happening I see happen over and over again to people and over and over like, what if we could get to them with this information before the fear hit them? Then maybe it would be easier to deal with and quicker and maybe not as painful. So that's kind of where I come from when I'm making content.
Erika Forsyth, MFT, LMFT 31:23
But yeah, yes, we are all on our different stage and age in our relationship with diabetes, yeah, for sure. And we want to offer support and encouragement, and we always have to hold where you're you know, where am I in this journey? Where is this person coming from? And that could be hard to do if we're not pausing. No,
Scott Benner 31:46
no. This line here that you have in your note, grief is not linear. Intensity of grief can pop up at any time, and there's a lot of and there's first times for a lot of different things. It just just kept making me feel, made me just think about over and over again. Like, I don't know that people would understand how valuable the private group is for me, feeding the podcast, right? Because I it's almost like, sometimes it's almost like, you guys are all in a room together, and I'm like, behind a I'm behind like, a one way mirror. And like, you know, get to say, like, oh, look, that happens all the time, like we have lists of things you wouldn't imagine. One I just saw today was common questions that people have online, common fears that we keep lists of all that stuff to try to inform the podcast. So I didn't mean to make anybody feel like they're like a test subject on the other side of a piece of one way glass, but, but when they're willing to live their life out like that, besides all the great communal things that happen and the support that happens in the social setting, you're actually helping me to make a better podcast as well. So pretty great.
Erika Forsyth, MFT, LMFT 32:52
That is great. Yeah, good. So
Scott Benner 32:54
now we got to get to the schools, and we have all this sorrow, what are we going to do with it? Yes,
Erika Forsyth, MFT, LMFT 32:58
okay, so what? So, yes, what can we do? What can we do with this, this chronic sorrow, because you're caregiving for a chronic illness. So grieving without a timeline is the major tool here, and then we're going to go through some specific items. One of the things that I hear the most is having an expectation around when the grief should be over, and that then lends itself to shame, right? Like, okay, it's been a week, or it's been a month, it's been six months, it's been a year. We should be getting it by now. Why we should be and again, I'm holding both of these. We should be getting it now the diabetes management side, and I should be feeling better. I shouldn't be grieving as much. I shouldn't be crying as much. I shouldn't be lamenting as much. So not only are you feeling the primary emotion, which is the grief and loss, you're then piling on shame that you should be in a different spot, and that is keeping yourself kind of stuck in that cycle. I know this can feel complicated, right? Because you're saying, Well, it's a chronic illness. There's chronic sorrow, but don't put a pressure on your don't put a timeline or expectation around when you should be done. And so it is important to hold that loosely and give yourself that freedom to be on your own journey. And again, it might be more challenging for you and your own story because of your past history and past trauma. And so just by allowing yourself to say, okay, yes, it's been a year. It's been two years, and yes, maybe I feel better, but it still feels hard. Now we'll get into kind of the nuances of, you know, what's right, what's appropriate, but I think you you know, like, how are you functioning? Like, noticing some of the things that we're going to talk to right about right now, but I want to pause. Did you want to say anything?
Scott Benner 34:55
In just 60 seconds, you can get your daily dose of vitamins. Minerals, pre and probiotics, adaptogens and more when you drink ag one. I drink ag one every morning, and you could as well. A recent research study showed that AG one was actually doubling the amount of healthy bacteria in your gut. These healthy bacteria work together to break down food and are known to alleviate bloating, promote digestive regularity and aid in digestive comfort. Long term, ag one is made with bioavailable ingredients that actually work with your body. So start with ag one and notice the difference for yourself. It's a great first step to investing in your health, and that's why they've been a proud partner of mine for so long. Try ag one and get a free bottle of vitamin d3, k2, and five free. AG, one travel packs with your first purchase at drink. AG, one.com/juice box. That's a $48 value for free if you go to drink. AG, one.com/juice, box. Check it out. Just think it's, I don't know. I don't have the right word for it, but the idea that you could have some sort of a breakdown or a failure because you don't understand something functionally that you need to do for diabetes, and then you somehow get through it, and when it's over, the last thought you have is, I can't believe you messed that up. You don't even mean like beating yourself up at the end is just like, it's God, it's on. It's just an unfair thing happening to you twice, yes, long into this thing that you know, maybe your doctor hasn't even helped you with, or you don't understand functionally at all out the other side of it, and then your last thought is, you know, it's like self flagellation, really, and then really, then it just puts you back into a different issue, where you stay until the next thing comes up that you don't understand. And then the whole thing gets to happen over and over again. Oh, it just made me it bummed me out. You're bumming
Erika Forsyth, MFT, LMFT 36:48
me. I'm sorry that this is, yes, it is this is intense, this is heavy. This is what it's but it's real.
Scott Benner 36:55
But I do appreciate what you said about the timeline thing that happened to me, and now I'm acting like, you know, but it probably happens to everybody, like, Arden's one year anniversary. I don't know what I thought, but I thought I was going to wake up and magically understand diabetes that day. I don't know why we do that with arbitrary like, dates and times. And then I thought, well, one year wasn't enough. It'll be two years. And then the second year came, and I was like, I am not much better at this than I was last year. So, yeah, that's it's very important. But how do you, how do you give yourself like that loose hold on that idea that there's no timeline but guard against falling into an abyss you can't climb back out of either right?
Erika Forsyth, MFT, LMFT 37:35
Okay, great, great question. Scott, so I'm going to encourage you to notice a few things here in your in your thought process, and increase some awareness. So as we've already mentioned, you know, no parent envisions or expects the loss that's going to come, whatever that may be. But obviously, in this instance, we're talking about diabetes, and I encourage you, a lot of times, what I hear is the grief or the life that your child had before diagnosis, and then the grief and anticipation of a of a life that's going to be riddled with challenge and medical trauma for their child. And so the from the parents perspective, you know, you're you're grieving what was, and then you're anticipating a really hard life for your child, because that's all you maybe know and are feeling in the moment. And sometimes, then we, as parents, we put our own emotion or grief onto our child, not, you know, mistakenly not knowing or or we kind of feel like maybe we're doing it empathically. We feel like I'm, I'm going to connect with my child and worry for them and grieve for them, that it's going to be hard for them to play sport, it's going to be hard for them to go to college, it's going to be hard for them to find a partner. You know, all these things that, as parents, we worry about, I totally understand that, but then we have the diabetes there, and we project kind of worst case scenarios, and that's coming from the grief. And so I encourage caregivers, as you're grieving, to be mindful of how much is your own grief, and separate your grief from your child's journey and your child's relationship with diabetes and their own grief
Scott Benner 39:25
because they didn't have the same expectations for their life that you had, right? Exactly, so they're not judging their situation based on your expectations. Yes, they might not be nearly as upset as you are.
Erika Forsyth, MFT, LMFT 39:39
Yes. Ah, okay, that might not. How do you stop
Scott Benner 39:45
yourself doing that?
Erika Forsyth, MFT, LMFT 39:47
That might not make you feel better in the moment, right? But I think through a process of awareness, whether that's through journaling, through and, you know, obviously. Through therapy to separate your grief and your relationship with diabetes from your child's and obviously this is going to be so different based on the age and stage of your child at diagnosis, you will be surprised how much your child remembers before diagnosis. I will speak for I was 12. I don't remember what it was like to not have diabetes prior to 12, right? Some kids might remember who were diagnosed at five. They might remember, you know, everyone is different, so how do you separate it again? It's it's being mindful every time you're thinking, Oh, my child, are they gonna base? Are they gonna all the things I just said? Are they gonna play sports? Are they gonna find a partner? Are they gonna do all these things that I envision them to have this six? Have this successful, thriving life, that that is your grief and your worry and your they aren't feeling that when you start to feel and be mindful that gosh, is my child going to feel this? Their child is not going to feel that they mean, they may have, they may have challenges,
Scott Benner 41:00
yeah, but they're not gonna be overwhelmed the way you are, because expectation is really the it's the enemy here, right? Like, because you don't recognize that you had all the expectations you had the day before diabetes, and that most of the things you thought were going to happen, or the way you thought they were going to happen, they're not actually going to happen that way, but that gets to unfold slowly over years and decades, and so you adjust as you go, Oh, I thought my kid was going to play soccer because I played soccer, but it turns out they really love baseball because sports where you can't use your hands aren't sports. I'm sorry. I was just kidding. And like, so that adjustment happens when they're seven, and you go, Okay, well, I wanted to play soccer about you play softball anyway. It's okay, no big deal, right? Like, but when it all comes in one shot and your brain starts rolling through all of the expectations you had, you don't stop to tell yourself, oh, this wasn't actually going to go the way I thought it was going to anyway. So this isn't that big of a deal. You just say this is what life was going to be, and now it's not going to be that. And so we give like it said, it's all it's all ruined, you know what I mean? And then that's how you feel. But that's not the case. Like people are going to come help you, if you're in this community, they're going to say to you, don't worry. I did this with diabetes when I grew up, or I did that, or I drove here, like, you have any idea? I just shared Arden's graph one time while she drove to college, and it was an all day drive. She drove like, 12 hours one day, and so many people were like, like, adults who came back and said to me, this is so encouraging to me, I won't go on long drives. I'm like, oh. And I thought, God, you don't go. You're an adult. They won't go on a long drive because they have diabetes. And then just seeing some kid leave for college, and they're like, Oh, she did it. And then they just reset their expectation, and then then they do it. It's awesome. Actually, I'm sorry. I feel like I got you off track. Yes,
Erika Forsyth, MFT, LMFT 42:58
no, no, it's good. It's good. And we'll, that's a good point. We'll, we'll expound on that. Okay, going back to your question of, you know, giving yourself permission to grieve without a timeline, what do you do? How do you kind of keep yourself in check, right? Like, how do you know, and so noticing, I encourage you to notice the amount of time, like, literal time that you are grieving privately and publicly and again, this can be at any stage from diagnosis. And I told the story the conference I shared here again to shortly after, my brother was also diagnosed with type one, two years after I was and I remember we went out to a restaurant, and the hostess was walking us to a table, and she directed us to a table, and my mom said, We can't sit there. My children, both my children, have type one. And so she we kept walking us to another table, and I remember looking at my brother, and I remember being horrified, and just like, why did she tell this person what there's nothing to do about the table, like, what is, you know, I was just like, solely embarrassed and probably pretty angry too at the time, and upon reflection, I now think and believe that my mom was grieving. She obviously had nothing to do. She
Scott Benner 44:19
just wanted to tell somebody, I'm struggling. My kids are struggling. We have problems like, be empathetic with me, yeah,
Erika Forsyth, MFT, LMFT 44:28
like she, I mean, maybe she didn't like the table where it was just like, um,
Scott Benner 44:33
I got a card who says type one on it. We don't have to sit in a booth like a common person, by the way. I prefer a booth, but
Erika Forsyth, MFT, LMFT 44:39
I'm sure, I'm sure she, she probably didn't like the table, but it came out as both my children have type one and feel
Scott Benner 44:47
bad for me and give me the table I want. I gotcha. I got so
Erika Forsyth, MFT, LMFT 44:51
she, I mean, and this happens right? Like, we tell when we are grieving and we're kind of like just oozing out. And flooding over and again. This is normal when we are in a really intense situation. For a lot of people, a lot of people will hold everything in and not say anything, and a lot of us will will share everything to anyone who can listen, and she was grieving I needed to tell people. And didn't, you know was landing in different places, yeah, and so just noticing, are who are you? Who are you talking to? Are you talking about it all the time? Are you reading? Are you going, you know, again, the Facebook group, other social media, are you going there to find support or to share your story and receive some validation and normalization of your experience that is so healthy and probably really powerful for you in the moment. And then are you finding yourself hours later reading through traumatic story after traumatic story. So perhaps your initial motivation is to go to a community who understands you, to be validated, supported. You receive that. But then we're humans. We get, we get sucked in, and then, then we're, then we're experiencing kind of more vicarious trauma and reliving everyone else's trauma. And so just notice, how long are you doing that? What is the impact you don't
Scott Benner 46:28
want it to turn into disaster porn for yourself, where you're just like, Oh, I've worked through my problem. Now let me go relive it again and again and again and again. There's a difference between community and searching out those stories that why do people want to feel badly, though? Is it because at least they know how it works? I
Erika Forsyth, MFT, LMFT 46:47
think it's initially you feel validated because you're saying, oh, this person went through that too. This Karen is struggling with the same issue I am. Yeah, and that feels good, because then you feel that isolation is decreasing and decreasing and simultaneously, depending on how much time you're then exposed to can you become consumed and overwhelmed by all everyone else's trauma? Yeah, right. So there it is this. It's a sweet balance of finding it just going to support groups in person. I
Scott Benner 47:22
think in the 70s, my dad would have said you have to pull your head out of your own ass at some point. Is that, is that what you're saying? No, of course, that
Erika Forsyth, MFT, LMFT 47:34
is not what I'm saying. I think it's, it's, you know, noticing then this is, it is hard to and even as I say this, like notice your thoughts increasing that awareness of what you're doing is hard to do when you're exhausted and trying to just get through the day and trying to manage it all, yeah, not just your child's diabetes, to manage it all, so that even in and of itself may feel challenging, and the awareness piece of noticing how much you're talking about it, reading about it, crying about it, consuming yourself with it. There is a time and place for that. And notice if you feel like you're you're stuck in it, yeah. Also, you can
Scott Benner 48:15
just look at your kids while you're talking to other people, because if you've been telling the same story over and over again, they will be looking at you cross eyed. So, you know, has everyone not been in that situation where they're like, why is mom telling that person so much like, I have that story from when I was a kid. I was like, What is she's really oversharing here, yes, and I Yeah, I hear you. Yes. Okay, yeah. I just want to say like that to me, sounds like the most difficult part of all this, because I don't imagine that most people are standing up and saying, I'm gonna go do something now that is really unhealthy for me. Like, you know, you don't know you're doing it when you're doing it, to be aware of it to, I guess, helps you see it eventually. And then maybe then you can, you know, curb it somehow. But I'm sorry, go ahead.
Erika Forsyth, MFT, LMFT 49:01
Yes, it is. It is hard, and in the moment, you're dysfunctioning from moment to moment, day to day. Yeah. So these are, these are tools that, when you have the bandwidth to implement and start to noticing, what are the thoughts, what are my actions, and how are they impacting how I feel one thing that I know we've talked about before is the dear diabetes letter that I think is powerful. Whether you're living with diabetes or you're caregiving, doesn't matter what type, but oftentimes this goes back to you want people to know how hard it is to live with it, to care, give, and they don't really understand, and you hold a lot of feelings towards the actual diabetes, but it can't, can't talk back to us, you know, right? And so this is a tool that I know many people have found to be successful, to do not just once, but monthly. Or annually, and you're writing, you are literally writing a letter, dear diabetes, comma and let it all come out. Sometimes it'll be neutral, sometimes it'll be full of hate and rage and anger. Sometimes it'll be sadness. And I think if you do practice this kind of in a ritual way. If it feels helpful, it's interesting to always look back, because I think we often forget that we have healed or we have grown. And so when you can look back and be like, Wow, two years ago, I was in a real I really hated diabetes. Yeah, I tell you now all
Scott Benner 50:37
the time, a year from now, you will not recognize yourself today.
Erika Forsyth, MFT, LMFT 50:41
You do say that, yeah, it's just true. I'm sorry. And if we know it's it's so true, but we forget. We forget because it's hard to remember where you were and where you are today for sure. And so I think that can be a really effective oftentimes, what comes out in these letters, too, is an anger and kind of disillusionment with people's when they if they have a faith or belief in God or kind of the universe, whoever your relationship is to a higher power, if you have that, that often comes out in these letters, and people are surprised by that, and that kind of goes along with the expectation of what your life is going to look like.
Scott Benner 51:23
I mean, that's you don't even think about that, that that extra layer of it's not just like, oh, I wanted my kid to be able to do this thing, or I didn't want to be up in the middle of the night dealing with something. But if you have those beliefs, then somehow this, this entity, decided to screw you right, like that's, that's what it feels like, yeah, and that's got to be hard to deal with too. Okay, all right,
Erika Forsyth, MFT, LMFT 51:49
okay. The practical tool, the dear diabetes letter, the kind of psychological, emotional tool of noticing your thoughts and your actions, I have also found through, you know, professional work and also listening to all the stories on the podcast, that your past really does impact how you cope and with with the diabetes. And I have found that if you you know if you have past trauma or even specific experiences with diabetes that impacts your not only your grieving, but also your like, hope and belief that things are going to get better or or that it's just going to always be hard. Conversely, if, for example, when I work with caregivers who have type one and then their children have type one, it's a different experience because they have the belief and hope that they've lived with it. There's still grief. It's still hard, right? But it's different. And even for caregivers who have partners or other family members who have type one or another form of diabetes when their child is diagnosed and it's positive and it's positive, their grief is still there and present, but there's a hope that's easier to grab onto, as opposed to when you have a negative either experience with diabetes or a negative either medical trauma or trauma in general. And so I know, I know again, we've, we've spoken into that piece a lot, but I think it's important to park it here too.
Scott Benner 53:31
I'd be remiss not to say that when we did that four part series about resilience, how much I learned about past trauma and how it affects who you are in the future. Really, I thought that was awesome. But what you put together for that one, and so I'll throw it in here. It's episode 1229, 1235, 1245, and 1250, I mean, if you want to look into why you might do what you do, or react the way you react, it's, it's just super helpful for that, I think,
Erika Forsyth, MFT, LMFT 53:59
thank you. Yeah, I think it was, there's a lot of content there that might help you kind of understand and at this point that we're talking about right here, yeah, yes. And then if you are having difficulty, even having the bandwidth, time energy to notice your grief, obviously, having, you know, sessions with therapists or mentors, and if you feel safe enough, asking close family or friends to reflect back to you how you're doing. To say, it's a vulnerable question. To say, How am I doing with my grief? Like, how do you feel like I'm doing? And again, this is it's I want to make sure that you ask that in a in a relationship that feels safe insecure, a
Scott Benner 54:50
kind truth teller who understands the big picture, not just somebody who's going to look at you go, you're being dramatic, like that kind of
Erika Forsyth, MFT, LMFT 54:57
thing. Yeah, yes, right. So I'm talking. You know, mentors, pastoral counselors, therapists, maybe a really close family member that has walked with you for a long time, somebody who understands, somebody who understands and also knows you. Because at some point you might be healing in your grief. Again, we know that it's chronic, but you might be healing, and you might not even be aware of that. And they could say, no, actually, look, you, you were doing X, Y and Z, and you weren't able to do that last month or last year, yeah. Or they might say, gosh, you know what? I think it seems like you're you're still in a really hard and challenging place, and that might be because I don't know what's going on, but how can I help you? So again, it's a vulnerable question to ask non professionals, but it can be really powerful, right?
Scott Benner 55:48
Yeah, definitely vet out the person you're going to ask that from, if it's not a professional person, who can, you know, be thoughtful, a third party, that kind of thing, like, Yes, don't be surprised too. If either, if your spouse is either great, like at this, or not great at it, because they're also going through the same thing you're going through, but they experience it differently than you do, because when they were eight, something different happened to them than what happened to you when you were eight. And so it's, I know people, there probably are people who hear that think, oh, that's like therapy mumbo jumbo. But man, that I'm telling you that resilience series, I was like, Oh, my God, that. What's that list that the 10? How come I can't think of the name of the list of the things that, if you have a certain a number of them, have happened to you in the past. Oh,
Erika Forsyth, MFT, LMFT 56:36
the aces, yes, the adverse childhood experiences. Yeah. That
Scott Benner 56:41
thing opened my eyes. And I have more than although I couldn't remember the name of it right now, I have more than one time, more than a dozen times in my life, pulled this thing up in front of other people and gone through and went, Hey, have you ever experienced emotional, physical or sexual abuse? How about neglect? Emotional or physical and like, gone through it like that. And you can see people ticking in their heads, and then, you know, they come up with, like, Oh, I've got, like, four things on this list, and you and they go, oh, oh, yeah, oh, okay. And then they all of a sudden, see their situation, really fascinating. So anyway, yes, think we're to the end,
Erika Forsyth, MFT, LMFT 57:16
but I don't want to we're to the end. We are to the end. Yes,
Scott Benner 57:19
I can't. Thank you enough. Seriously, this is wonderful. I was so excited when you reached out about this. So thank you.
Erika Forsyth, MFT, LMFT 57:24
You're welcome. I hope it's hope it's helpful. Tell people where they can find you. Erica, forsythe.com,
Scott Benner 57:32
you have a website. Everybody's got a website, Erica, but yours is awesome. They should go check it out. That is my website. Yes, you can help people virtually in what states,
Erika Forsyth, MFT, LMFT 57:41
California, Oregon, Utah, Vermont and Florida. And
Scott Benner 57:46
you can see people in person if they're Cal California
Erika Forsyth, MFT, LMFT 57:49
or California. Yeah, I have an office in Southern California in Pasadena.
Scott Benner 57:53
Thank you so much.
Erika Forsyth, MFT, LMFT 57:54
I appreciate you.
Scott Benner 58:03
I'd like to thank the Eversense 365 for sponsoring this episode of The juicebox podcast, and remind you that if you want the only sensor that gets inserted once a year and not every 14 days, you want the Eversense CGM. Eversense cgm.com/juicebox, one year. One CGM, a huge thank you to one of today's sponsors. AG, one drink. AG, one.com/juicebox you can start your day the same way I do with a delicious drink of Ag, one, OmniPod five sponsored this episode of The juicebox podcast. Learn more and get started today at omnipod.com/juicebox, links in the show notes. Links at juicebox podcast.com. If you're looking for community around type one diabetes, check out the juicebox podcast. Private, Facebook group, juicebox podcast, type one diabetes, but everybody is welcome type one, type two, gestational loved ones. It doesn't matter to me, if you're impacted by diabetes and you're looking for support, comfort or community, check out juicebox podcast, type one diabetes on Facebook, if you or a loved one was just diagnosed with type one diabetes, and you're looking for some fresh perspective. The bold beginning series from the juicebox podcast is a terrific place to start. That series is with myself and Jenny Smith. Jenny is a CD CES, a registered dietitian and a type one for over 35 years, and in the bowl beginning series, Jenny and I are going to answer the questions that most people have after a type one diabetes diagnosis. The series begins at episode 698, in your podcast player, or you can go to juicebox podcast.com and click on bold beginnings in the menu. Are you starting to see patterns, but you can't quite make sense of them. You're like, Oh, if I bolus here, this happens, but I don't know what to do. Should I put in a little less? A little more if? You're starting to have those thoughts, you're starting to think this isn't going the way the doctor said it would. I think I see something here, but I can't be sure. Once you're having those thoughts, you're ready for the diabetes Pro Tip series from the juicebox podcast. It begins at Episode 1000 you can also find it at juicebox podcast.com up in the menu, and you can find a list in the private Facebook group. Just check right under the featured tab at the top, it'll show you lists of a ton of stuff, including the Pro Tip series, which runs from episode 1000 to 1025 I can't thank you enough for listening. Please make sure you're subscribed or following in your audio app. I'll be back tomorrow with another episode of The juicebox podcast. Hey, what's up, everybody? If you've noticed that the podcast sounds better, and you're thinking like, how does that happen? What you're hearing is Rob at wrong way recording, doing his magic to these files. So if you want him to do his magic to you, wrongway recording.com, you got a podcast. You want somebody to edit it. You want rob you.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#1350 Don't Get Stuck in the Mud
Jess is the father of a nine year old type 1 who wants to get more in touch with his emotions.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Here we are back together again, friends for another episode of The juicebox podcast.
Jessie is the father of a nine year old daughter who has type one diabetes. She was diagnosed just a year ago, and she's already taking a big chunk of the care on herself and has an A, 1c, in the sixes, nothing you hear on the juicebox podcast should be considered advice medical or otherwise, always consult a physician before making any changes to your health care plan. When you place your first order for AG, one, with my link, you'll get five free travel packs and a free year supply of vitamin D drink. AG, one.com/juice, box. Don't forget, if you're a US resident who has type one, or is the caregiver of someone with type one, visit T 1d, exchange.org/juice box right now and complete that survey. It will take you 10 minutes to complete the survey, and that effort alone will help to move type one diabetes research forward. It will cost you nothing to help. I know that Facebook has a bad reputation, but please give the private Facebook group for the juicebox podcast, a healthy once over juicebox podcast type one diabetes.
This episode of The juicebox podcast is sponsored by cozy Earth. Use the offer code juicebox at checkout@cozyearth.com and you will save 40% off of your entire order. The episode you're listening to is sponsored by us. Med, usmed.com/juice, box, or call 888-721-1514, you can get your diabetes testing supplies the same way we do from us. Med. This show is sponsored today by the glucagon that my daughter carries, gvoke hypopen. Find out more at gvoke glucagon.com. Forward slash juicebox. Hello, everyone.
Jesse 2:14
My name is Jesse. I am a dad of a nine year old daughter, Brianna, who was diagnosed with type one diabetes in February of 23
Speaker 1 2:30
February of 23 she's nine now, or was nine then she was eight, then, okay, correct. It's been a challenging year. Yeah. Do you have any other kids?
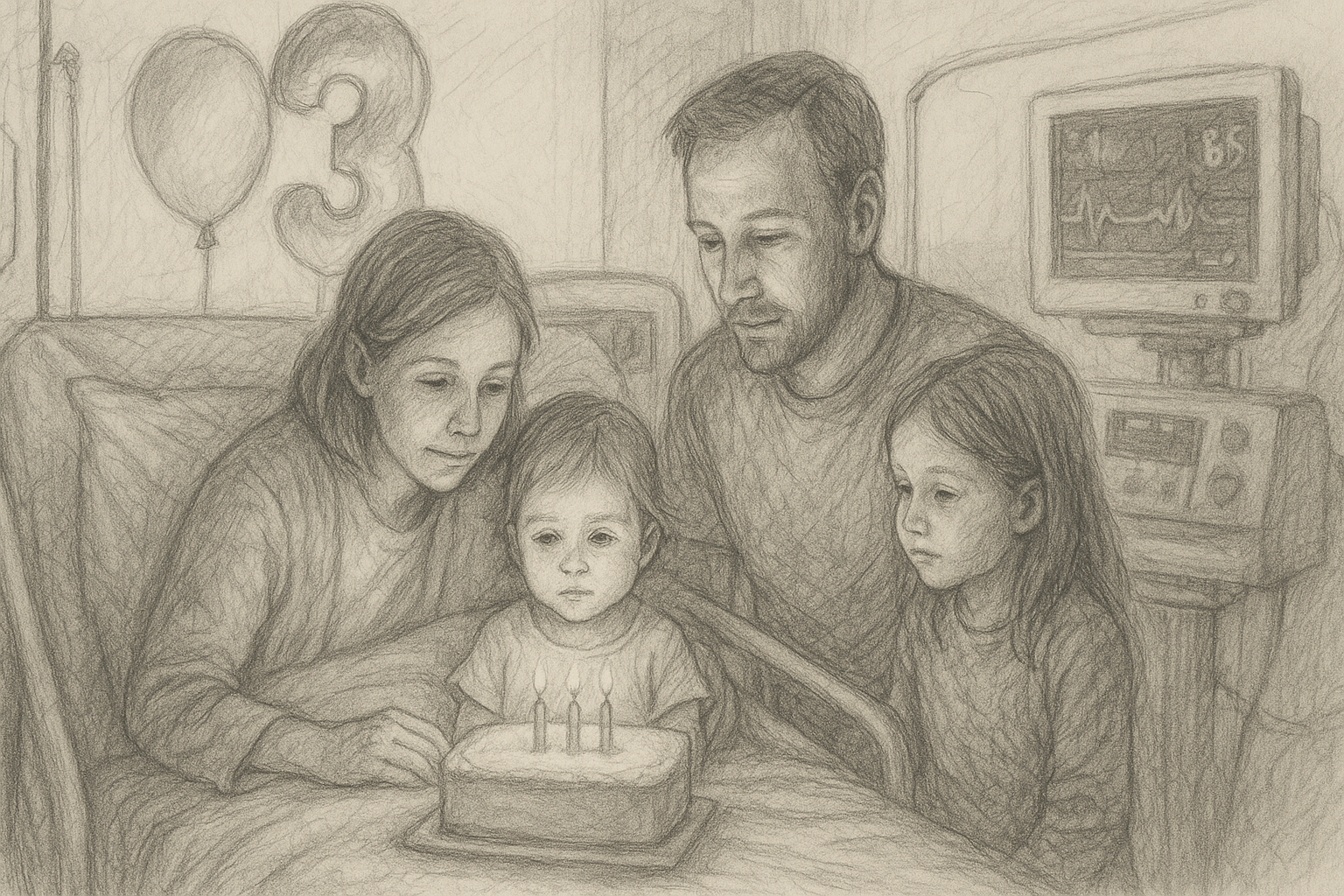
Jesse 2:43
So my son is five, and his so my daughter was in the hospital February 21 and his birthday is February 24 so we were just in fact, she told the doctors, I want to be discharged so I could go home for my brother's birthday.
Scott Benner 3:03
Did you have the birthday in the hospital? Or did she make it home?
Jesse 3:06
We made it home, which was awesome. Very
Scott Benner 3:09
cool. Was this a surprise? Do you have type one in your family?
Jesse 3:14
It was a complete surprise. No diabetes in the family.
Scott Benner 3:18
Okay, how about now that you've been with it for over a year, other autoimmune stuff that you've noticed with yourselves or her? Yes, so
Jesse 3:26
in 2014 and that's the year that she was born, I had issues that were undiagnosed for five years, and in 2019 I was diagnosed with autoimmune disorders. I've had two of them. One of them is children's, and the other is Hashimotos, which is also news to me. It's, it's new to the family, okay, that I'm aware of.
Scott Benner 3:53
So you think your Hashimotos symptoms go back for years. It's
Jesse 3:58
kind of tough, because I think my primary is definitely showgirns, and I check just about every single box for that. And I denied it for like, a year or two, saying there's no way, how could I have this? It doesn't make sense. It's gotta be something else, you know, continuously trying to look and find an answer, but I check almost every single box for that the Hashimotos. To date, I still don't require any treatment or anything. My levels are still relatively normal, but I have the presentation, you know, the scan of my thyroid and everything gives me the presentation of Hashimotos.
Speaker 1 4:39
Can I ask you, do you have any symptoms of it? No, no. And what? What are your PSH levels when they measure them?
Jesse 4:48
I don't know offhand, but they're, they're all within normal range, and they, in fact, I recently saw a second endocrinologist for a second opinion, and. And still have to do the blood work on that, but I have been tested multiple times from TSH levels, and they're relatively normal.
Scott Benner 5:08
Yeah. So there's a pretty wide range in the testing. So if you are over like 2.1 TSH and you have symptoms, they might still tell you you're in range. But if that ever happens and and you have symptoms, tell them you'd like to treat the symptoms. Yeah, because at
Jesse 5:25
that point, like I said, the doctor wasn't willing to treat anything. That's why I'm looking for that second opinion, because I have most of my everyday symptoms are answered by the Children's but there are a couple things that are still unanswered. And it's you know question as is it rheumatoid arthritis? Is it Hashimotos? Is it other things, what do you have? Joint pain, muscle muscle tightness. Is a big one that really isn't answered by shogrens.
Scott Benner 5:58
Stiff back, stiff neck. Yeah, yeah. All the time. Crack your neck. Doesn't matter. Cracks again. Five seconds later,
Jesse 6:05
I have a spot in my shoulder blade that is just a constant knot, and it's, you know, and it's not answered by anything orthopedic. So it's kind of like Arden has all that interesting, yeah, she she diagnosed with Hashimotos as well, or just yeah, she
Scott Benner 6:24
has she takes um two thyroid medications. She takes uh tyrosine for t4 replacement. She takes cytomil for t3 replacement. If you take insulin or sofony ureas, you are at risk for your blood sugar going too low. You need a safety net when it matters most, be ready with jivo hypo pen. My daughter carries gevok hypopen everywhere she goes because it's a ready to use rescue pen for treating very low blood sugar in people with diabetes ages two and above that. I trust low blood sugar emergencies can happen unexpectedly, and they demand quick action. Luckily, jivo kypopen can be administered in two simple steps, even by yourself in certain situations. Show those around you where you store jivo kypo pen and how to use it. They need to know how to use jivo kypopen before an emergency situation happens. Learn more about why gvok hypopin is in Arden's diabetes toolkit at gvoke, glucagon.com/juicebox, gvoke shouldn't be used if you have a tumor in the gland on the top of your kidneys called a pheochromocytoma, or if you have a tumor in your pancreas called an insulinoma, visit gvoke. Glucagon.com/risk, for safety information. But she's like, we could start an ASMR podcast of just art and cracking herself. I mean, every
Jesse 7:54
so in my journey to getting diagnosed, I had a lot of physical therapy, and physical therapy seemed to be the only thing that helped me and but it's only temporary. Every therapist I've been to, every doctor I've been to, is just massage therapist. Their first comment is, Wow, you're really tight. And I'm like, Yeah, that's just my muscles. Hey,
Scott Benner 8:15
Jesse, can you hyperextend your elbows, your arms? Are you super stretchy? Can you pitch a baseball, really well, anything like that. No, no,
Jesse 8:24
I would say my joints are pretty flexible, like, especially my neck. I mean, it's tight and it cracks. But at the same time, the chiropractors that I've seen have also said there's a lot of motion,
Scott Benner 8:35
yeah, so you could maybe have you looked into um airs, Danlos Syndrome. I've heard of that, and I have checked into that at some point. Also, you're much louder right now. So whatever you just did, let's keep doing that. Okay, cool, okay, yeah, so that's an autoimmune issue that would be highlighted mainly with, like, super flexible flexibility, because your ligaments are extra stretchy. You might get, like, over like, hypermobility, I guess would be an easy way to say it, and there is no real treatment for it other than physical therapy. So that might be while, why, while you're doing the physical therapy, it's better, but then it doesn't stay better, gotcha, it's E, H, L, E, R, S, D, A, n, l, o, s, if you want to look into it, awesome. Yeah, that could definitely be it. And the thyroid thing, again, if you have a TSH over 2.1 like, say your thyroid is like three and a half that or four, and your doctor's gonna go, that's in range. You would say, I would prefer to be under two. Can we medicate it under two? It's one little pill. You take it like once a day. I
Jesse 9:42
just pulled up a 2020 result, and it's 2.090
Scott Benner 9:47
okay, yeah, almost 2.1 no one would medicate that. I wouldn't see anybody medicating that, but it's a watch for sure.
Jesse 9:53
Yeah, it's and that's 2020 so, yeah, okay,
Scott Benner 9:56
no, well, how about when you think. Back on your your family, your connected family, your mother, your father, aunts, uncles. Up until
Jesse 10:04
recently, the only thing would be my grandmother had rheumatoid arthritis, and that was the only known diagnosis. You know, autoimmune in the family, in the family. Until recently, my aunt on my mother's side and my grandmother's on my mother's side. My aunt was just recently diagnosed with celiacs.
Scott Benner 10:25
Okay, that's you guys, Irish, Italian, Italian. Okay, interesting. Do you have I'm gonna, I hope you don't mind unpick. I know you're probably, but I think I'm getting to your topic. So give me a second anxiety for you.
Jesse 10:42
No, no, nothing over the top. No,
Scott Benner 10:45
okay, you know, it's funny. I'm just gonna, I'm gonna throw this out there, because I want to get into your topic, right? You know, you sent a little note. Everybody sends a note about, like, what they want to talk about, and because, I hope you take this the right way. You have an androgynous name, so I didn't know if I was going to be talking to a man or a woman today, and now I'm going to say something that people are probably going to find offensive. I found your note I get I was guessing you were going to be a woman because you spoke so much about trauma in your note.
Jesse 11:22
It's interesting. I mean, so when I started my pitch, my pitch was, Hey, Scott, I'm just a dad. I'm just a 45 year old dad, and it's just like, I'm just a regular dad kind of thing. But I will tell you that this diagnosis hit me hard. My wife was the champion the let's put all that crap aside and full steam ahead, let's figure this out and get going. And I was holy. Now, what
Scott Benner 11:53
you know, like stuck was that your personality prior to it,
Jesse 11:57
no, no, no. Like, I'm, I'm, I'm,
Speaker 2 12:01
I think I'm often the problem solver,
Jesse 12:06
the let's deal with reality. We need to get to the next step. My wife is also like that. Both type a people that just, let's go, let's, you know, get things done, right? You know, there's, there's, you know, going back to college, you know, a breakup hit me hard. Generally, I'm not the emotional guy. I'm the, let's do, you know, I'm very task oriented. And for some reason this not, for some reason, this just hit me. Yeah,
Scott Benner 12:37
you think it could be, because it is your daughter 100%
Jesse 12:40
you know it's like when it's your own kids, and it's the same thing, like anything medical you could give me gunshot wounds, stabbings, somebody bleeding all over the place, and I'm calm, cool, collected, no problem. My daughter gets a paper cut, and my wife is often like, get out of the way. Let me do this. And it's like, it's, it's my daughter.
Scott Benner 13:04
I don't need this guy crying on the band aids. We gotta go. I'm telling
Jesse 13:08
you, like, she literally pushes me out of the way and says, Get out of here. You're no help. So, and it's, it's strange for me because like that, that's like, my, um, that's my wheelhouse. That's, you know, I have no problem with that, but it's my daughter and I just, I crumble. Do you freeze or do you fall apart? Um, just fall apart. I don't. I don't freeze like I definitely act, but I'm a mess. You know, it's just not the typical my wife's right. Get out of the way. You're not
Scott Benner 13:41
crazy. Tell me about about Brianna's diagnosis. Then how did you guys figure it out? No, it's,
Jesse 13:47
it's kind of like mirrors, you know, everybody else's story leading up to it. She was super tired. We had just gone to Disney in December, in December, all the way back then, she wasn't herself, like, I remember saying it to my wife like, She's awfully quiet, she's not quite herself. And then come February, you know, up at two, it she the the bed wedding is, was the final clue that, you know, we're like, something's not right. We, you know, we did the research, we looked and we're like, diabetes. Maybe she has diabetes. And, you know, like a typical parent would do, I went in to denial, and I was like, nah, nah. That seems crazy. But again, she checked
Speaker 2 14:36
the boxes. So we scheduled an appointment
Jesse 14:41
with the pediatrician just prior to the bed wedding, and then she wet the bed and like the following, like, I don't know it was like four days away or whatever, that we had the appointment previously scheduled. So we're like, Okay, let's get her to the doctors and see what happens. I'm. Never forget it, because I don't know what happened, but I promised Brianna. I was like, Yeah, well, I'll get you a smoothie. So let's go get a smoothie. We'll go to the doctor or whatever. We just happened to be running late, so I was like, All right, the smoothie is going to have to wait until after the appointment because we're running really late.
Go in,
I knew what was going to happen. I knew they were going to check her sugar. And I don't know if I expected it to be high or not, because I really didn't really believe it. I was like, There's no way. Yeah, but sure enough, they checked it. She was I forget what the number was, but by the time we got to the hospitals, it's close to think it was 600 you
Scott Benner 15:41
know, you and I live so close to each other. I think you might have gone to my kids pediatrician as possible. Yeah.
Jesse 15:47
I mean, it's like, it's crazy, because it's funny, because the office that we normally go to, we went to a different office because there was the available appointment, right? They were like, you have to. I think they did the finger stick there, but we are the urine test, but we had to go to the other office to do a finger stick or something. I forget. It's kind of all a blur. They made us go to the other office in another town before we went to the hospital? Were
Scott Benner 16:21
you? Well, maybe it wasn't my pediatrician. It sounds like a sounds like we got to get you to a better place. But so wait. So what are the um, with the four of you together,
Jesse 16:29
where did you just go? It was just me and her.
Scott Benner 16:32
Why did they send Captain crumble? How come your wife didn't go? Did you? Oh, you didn't know this about yourself yet. No,
Jesse 16:38
that's true too. Like, I mean, I wasn't crushed at that point. So, like, you know, but still dealing with her with any true emergencies. It's
Scott Benner 16:50
not, not the best. But how often does that really happen?
Jesse 16:53
Yeah, it doesn't, yeah. So it wasn't like anything, you know, it's super known. But then after that, it was like, I just went into, like, a tailspin pretty quickly that day, no, no, I think the during the hospital stay, like it was just, you know, once we got the confirmation, once, you know, they did the finger stick and sending us to the hospital like it. I mean, I, I knew at that point. And once we got to the ER and they did the intake and whatever, the number was six, 700 I don't quite remember, but it was definitely high at that point. I wouldn't say I was crumbling, but it was like, Oh my God, you know, like it was just, what
Scott Benner 17:38
were the thoughts that were getting you. Do you remember specific things that were were alarming to you? I mean, I listen, I understand the whole thing's alarming, but were there things that stood out, I think,
Jesse 17:50
for me, and I think why it hits me, hit me hard is and I think a lot of parents will say this, but like Brianna, is a very bright eight year old. She's in gifted and talented. She's super smart. She has so much going for her, super mature, you know, bright girl, really nice, great friends. You know, just everything about it is like, this is perfect daughter kind of thing. Just knowing the diagnosis it, it was just,
Scott Benner 18:25
did you think her life was over? Yeah,
Jesse 18:28
yeah, that that's, you know. And again, it goes to that my wife pulled me back in. Like, hello, this isn't cancer. Like, you know, this isn't death sentence, you know, so to speak. So, yeah, like, you know, in my mind, this totally changed her life. You know that I didn't view it as a speed bump. I viewed it as crushing, like a crash,
Scott Benner 18:53
like, like, we Oh, my God. She only made it seven, eight years, and now and now, all the promise of her life is gone. How
Jesse 19:02
is she going to do those things that we envisioned? You know, you know her bright future and right just taken away or gone. A little, you know reality, a little knowledge and understanding what diabetes is, and knowing that it is not a stage four cancer or something like that. I mean, once reality sets in, it's not that doom and gloom, but I I still had a really hard time with why her, you know, like that. Why did they why God, pick her, you know, why does she have to go through this, that type of stuff.
Scott Benner 19:41
Was your life going really well up until then? I mean, it was good, good. Okay, not like you like, but things were going the way you expected they I guess that's more. Mike, yeah, that so that's how I felt, right, like things weren't easy, but they were going I had a goal. We had goals together. Things were moving towards those goals as expected, exactly, yeah. Then the diabetes is, like, it felt like the thing that, really, I was gonna, if it, like, if me up, because I was like, it's maybe the first time as an adult that I thought, Oh, I have no control over any of this. Yeah, yeah.
Jesse 20:18
It's, it's, you know, all that taken from you. You know, you have zero control. And as far as I want to say, like the outlook, I mean prognosis or whatever, like at that point, you don't, you're not really in tune to all the nuances of diabetes. But at the same time, you know, it's not stage four cancer, but it's still heavy, yeah. And I think once throughout the hospital stay, you know, and seeing, okay, yep, she's going to be okay. This isn't, you know, it's manageable. There's tons of stuff out there, seeing, you know, the various people who came in during the hospital, it was outstanding, even like I I hear, you know, horror stories from people admitted and whatnot. And we had an unbelievable hospital stay. We had, we got connected with her current doctor. You know, when she was like, you know, I practice outpatient. She could be my patient if you're interested. And I'm like, Absolutely, you seem great, you know. And she she is her doctor. Is amazing. That stay in the hospital definitely helped. But it's still overwhelming, you know, and that fresh feeling of, now, what? And
Scott Benner 21:40
it doesn't take long for you to realize that as good as the hospital was and how and as comfortable as they might have made you feel that they didn't really tell you, like, a small percentage of the things you're actually going to need to know no fault of their own. Like, how would they
Jesse 21:52
but you were really I feel like we were really lucky. We had an unbelievable educator. You've
Scott Benner 21:58
probably heard me talk about us Med, and how simple it is to reorder with us med using their email system. But did you know that if you don't see the email and you're set up for this, you have to set it up. They don't just randomly call you, but I'm set up to be called if I don't respond to the email, because I don't trust myself 100% so one time I didn't respond to the email, and the phone rings the house. It's like, ring. You know how it works. And I picked it up. I was like, hello, and it was just the recording was like, us, med doesn't actually sound like that, but you know what I'm saying. It said, Hey, you're I don't remember exactly what it says, but it's basically like, Hey, your order's ready. You want us to send it? Push this button if you want us to send it, or if you'd like to wait, I think it lets you put it off, like, a couple of weeks or push this button for that, that's pretty much it. I push the button to send it, and a few days later, box right at my door. That's it us. Med.com/juice, box, or call, 888-721-1514, get your free benefits checked now and get started with us. Med, Dexcom, OmniPod, tandem, freestyle, they've got all your favorites, even that new islet pump. Check them out now at usmed.com/juice box, or by calling 888-721-1514, there are links in the show notes of your podcast player and links at juicebox podcast.com to us Med, and to all the sponsors. The podcast is sponsored today by the place where I get my oh gosh, my sheets, my towels, some of my clothing, a lot of the things that I stay warm or comfortable with. Cozy earth.com I'm wearing a pair of cozy Earth joggers right now. I've recently gotten another pair in a different color. I sleep on cozy Earth sheets. They are so comfortable and soft and temperate, temperate meaning I'm never hot or cold, which is really saying something, because my wife loves to turn that giant fan on, but they keep me nice and warm without making me like, sweaty or moist. You know what I mean? You don't want to be moist while you're sleeping. And then, of course, the waffle towels I use every day to dry off my bits and parts after I've showered. Cozyearth.com use the offer code juice box at checkout to save 40% off of your entire order. I'm not saying 40% off of one item. I'm saying 40% off of everything you put in the cart. Cozyearth.com use the offer code juice box at checkout.
Jesse 24:24
They got her CGM on her, like, day one or day two. Like, I mean, super quick, just the connection of here's what's going to happen, as far as you know. Here's your MDI. Here's how it works. Here's all the calculations. We're not going to discharge you until you know what you're doing. A nutritionist came in, like we were peppered with you
Scott Benner 24:45
felt ready? Yeah, 100%
Jesse 24:49
like when we we left, we I forget how long we're there, three days, four days. I mean, it was on a longer end compared to a lot of people. Let's say day three. Three, like, I don't wanna say we were experts, but we were pretty comfortable.
Scott Benner 25:03
Did that end up panning out like in real, real world play? Did you actually know what you were doing?
Jesse 25:09
I Yeah, okay. I think we, like I and I attribute it to the A our the endocrinologist, amazing, and then the diabetes educator that we had. She also had type one, okay, it was absolutely huge. I mean, she hit every point that you would want to know, and she really, truly educated us before we were discharged.
Scott Benner 25:34
What's your background? That you felt like you picked it up so quickly. So I,
Jesse 25:39
I was an EMT. I was an EMT for about 10 years or so, high school through college, and now I'm a police officer. Now the medical aspect of things is always interest. I always had an interest in the medical field, okay, I think it was a combination of maybe a little bit of my background. I did not as an EMT. I definitely did not know diabetes until the diabetes, until Brianna was diagnosed. And the educator, as far as, like, being an EMT police officer, you get very, very, very little training. You
Scott Benner 26:15
know, it's funny, I don't want to shift this on to me, but I just felt for the first time that I might get a PBA card out of this podcast, and I got really excited. You could I have one you don't want to take responsibility for how I drive. Trust me,
Jesse 26:34
all of my I get, not different than many people in New Jersey, New Jersey. So I don't know, I don't
Scott Benner 26:38
even know how to describe what I use driving for, but it's some sort of a release, that's for sure. Isn't that interesting because at work, you're constantly, that's what you were alluding to earlier, like, in like, blood bang situations, you're okay,
Jesse 26:53
yeah, it's like, and, and my wife could see it as soon as you know, it's one of my kids, she's just like, get out. And typically she doesn't deal with the blood and all that stuff. But when it comes to her kids, she's on it. So we kind of reverse roles with that. Yeah, that's
Scott Benner 27:10
the mom thing, for sure. Yeah, that that whatever gonna say blockade they throw up in their brain in situations like that, is really impressive. You know, it's, it's like a superpower, really is crazy. I'm like, OmniPod. Like, normally she's so goofy, and now she's like, seems to know what's happening.
Jesse 27:27
So we have this, we have the same life. It's superhero powers. No
Scott Benner 27:32
kidding. Really cool. Okay, so you've taken the the diagnosis as a trauma. Did you go to therapy? Yeah. So not initially,
Jesse 27:42
initially, I think we were still very much in the management stage, just trying to figure it out and balance things out and more task oriented. So even though I was crushed, it took me a little bit of time, I don't know, let's say, actually, I guess it wasn't that long, maybe a month and a half, month to month and a half, before I found somebody. And the therapist that I found is a type one diabetic. I don't know that. I knew that up front, but he, he was a former paramedic, and I knew him like I've I've been to training, you know, he's a little bit older than me. I've been to training with him. I know he trained me to some degree, through various EMT classes, and I knew who he was, and I that's how I found him. And I think it just happened that he happened to be a type one diabetic, so I kind of got a double benefit, because he's familiar with the job and how I kind of react to things and deal with stuff. But then he also had the knowledge of diabetes, which was huge, because he can put things in perspective and just simply say, you know, her blood sugar's 200 she's not gonna die. You know, Jesse, how
Scott Benner 29:02
old are you? 45 oh, you're not that much younger than me. I'm sitting here as you're talking, and I thought this podcast keeps like surprising me as it grows like I didn't if you would have asked me, like, where on my bingo card do I have, like, in touch, open, honest male cop. On my possibility of recording with somebody, I would have put that pretty low on my list.
Jesse 29:28
You had me as young female mom.
Scott Benner 29:33
Yeah, no kidding, good for you. So,
Jesse 29:35
I mean, I do have an interesting background, like I started EMT wise, and I went to school. I was the first one in my family to go away to school, go through college, got my master's degree, and I got my master's degree in community counseling. I have the degree in counseling, and I at that point, I was like, I satisfied my family. I got. My degree, but this isn't what I want to do. And I did a lot of internships and stuff in the inpatient psychiatric inpatient because I liked the variety of it, and I quickly put myself through the academy doing the police thing. And that's where I want to be. My background is that typical of a police officer?
Scott Benner 30:20
Yeah. I mean, I know a lot of cops, if you listen, you might know that right, like I was, I was just at a retirement, my buddy just retired as a sergeant the other day, and I was, I was faced with all these guys I knew when I was younger, who had all gotten older. Such a crazy thing. Felt like I walked through a time where I was, you know, 1819, 20 and they were 2324 2526 like back then. And then I get there, and they're all like, you know, in their late 50s and early 60s, I was like, What? What happened to you guys? But they were all still very kind of classically the way you would expect them to be. And I think for people from the outside, you might have one picture I find the people I know who are police officers, to be really lovely people, but they're also more no bullshit people. They usually lean a little more conservative than liberal, maybe, like they fit into a bit of a into a mold, right? But, but nobody you'd want more than them in any kind of a personal situation, like anything like my lawnmower broke, to my kid just fell out of a tree, to I killed somebody. What do we do? These are the people I would call you know what I mean, not one of them is anything like you. Well, super interesting. Do you feel proud of that? No, I
Jesse 31:35
do like I I've been lucky to like. I'm lucky to have the background. That I do. Retirement wise, I'm definitely thinking along the ways of counseling for kids with diabetes. Like, that's kind of like, yeah. I mean, both my wife's pushed me to do that because they're not out there. They really don't exist. It's pretty tough. Yeah, there's
Scott Benner 32:01
not a ton of them. I'm just, I'm just surprised you didn't say I'm going to work security to car dealership, because that's pretty much so
Jesse 32:07
I have the mindset that as soon as I retire, I'm doing nothing police related, so and, and I think with my background, like, I'm lucky I have that option, which is, which is kind of nice,
Speaker 1 32:19
but you ever had to pull your weapon out? Oh yeah, yeah. The thing had things changed over the last 10 years around here. Oh, my goodness.
Jesse 32:30
The world we live in is crazy. Easiest way to put it, it's absolutely nuts. The thing that grounds me is the perspective and, like, just, you gotta put things in perspective. And like, when going back to the diagnosis, I couldn't do it like, like, you just spiral, because it's, it's my kid, you gotta look at the bigger picture. You gotta look at, you know, what is the reality of stuff, and put things in perspective.
Scott Benner 33:00
So you're doing that? Is that helping you? Yeah, 100%
Jesse 33:02
like I think, as time has gone on, you become more educated, you learn more, you're able to manage things, and you obviously become more confident and able to deal with stuff. It certainly helps. Yeah, I think for for me, where I'm at now, when I reached out to you to say, hey, I'm interested. You know, this diagnosis really crushed me, but at the same time, things were getting better, and you are the physical and the daily management of things is easier as time goes on and you know, you're less I guess, bothered by the late night lows or whatever it may be, because you're just able to deal with it. But Brianna has had a hard time mentally since I put the request in to be on the podcast. So the whole mental health aspect of it is shifting from you to her. Like, when I say, like I was crushed, like I felt it, but I don't she. She may have picked up on it, but I like, you know, like in your mind, you may think like a full blown depression, I wasn't there. It was just the maybe more of like an anxiety of now what and having to
Scott Benner 34:33
move on and deal with it. But
Jesse 34:34
I think, like I was able to do that relatively quickly. But for her, she internalizes things very much so, like where
she feels like it not that it's her fault, but it's that she's no good. And it's not,
I know it's not all diabetes, the daily stress. Answers of the disease has made things harder for much harder for her.
Speaker 1 35:06
Do you have examples of of some things that have gotten gotten the better of her? So
Jesse 35:11
I guess the latest thing for her is, you know, obviously, I think most kids that are diagnosed, obviously have to deal with their peers and a lot of the questions and things of that nature. And at first, Brianna was like, no shame. You know, here's my pod, here's my Dexcom. This is what it does, zero shame she was out there. She was not afraid to show them. And that kind of slowly morphed into, well, I don't want to put it there today. I'd rather, you know, put it on my arm. Wear long sleeves to so and so keeps asking me about it, and I don't want to talk to him about it to I think the biggest challenge we had recently was her nurse, her regular nurse was out with an injury, so we had a couple of substitutes, so the consistency was difficult, because she was, you know, she would text and say, I just got called down to the nurse's office for 130 you know, down or they called me down to the nurse's office at 90 and they wouldn't let me go to to class for 30 minutes. I treated with 15 carbs, but then they gave me an another 15 carbs. So, like a lot of different things, and like, over like a month's period of time, I was trying to figure out how much of it was her just reacting to things, or just having a hard time to how much of it was the nurses just not following the plan. It took a little bit of time to try to figure it out. And I'm like, You know what? My daughter is really smart. She pretty much has this why am I relying on the nurses at this point? Because she's having a hard time with the nurses, either over treating her or calling her down prior to a low to different different things, like one nurse just like to let her ride high, another nurse would not be okay with the Dexcom continuously going down, even though she already treated and should be going back up so she would overdose.
Scott Benner 37:33
Yeah, so once the new car smell like, wears off, and she's not like, you know, like, I've got diabetes, and it's cool, and let me show you my stuff. Like, once that happened, that went away, and, by the way, was that heard, were you guys pumping her up like that? Do you think, because I see that, I see that sometimes, like the parents are, they get, like, cheerleaders. And I'm like, oh, you know, you're trying to make something exciting. That's not really exciting, you know, like, No, I mean, insulin pumps are terrific and everything, but they're not like, on the level of, have you seen my new iPhone? Yeah,
Jesse 38:04
in the beginning, I think we were pretty we were very strong with me, encouraging her to help others understand, like, educate kind of thing, as far as showing stuff off. And I don't think so, like, I don't think we pushed that with her, but we were definitely like I was saying, we were, you know, with two type a parents, and we were very much with the teach people about this. If they want to know, teach them, tell them, educate. I think she did, but I think that we're off to the point where she became annoyed with the, yeah, too
Scott Benner 38:37
much, right? And then the kid that wants to know too much. It stops being fun, and it starts being like, leave me alone. And then the nurses start making mistakes, and then everything is a hassle, like it, it's holding her back instead of helping her.
Jesse 38:50
Oh, like, you know, she's diagnosed at eight, so I kind of envisioned, you know, burnout happening like 1314, 15, someplace in there. But here we are at age nine, and it's like, kind of like a burnout, and it's, it's just been at it for a year. Yeah,
Scott Benner 39:10
I saw somebody online today. They were kind of lamenting all the things that have been going backwards for their kids since the diagnosis. And it feels terrible when you're reading it. But like, there's this part of me that knows, like, this is all normal, which it sucks, because, you know, your kid wishing that they were somebody else because they don't want to have diabetes or something like that, is not, it's not an easy thing to hear, obviously. But then you start, you know, I start hearing the I can't take this anymore. Like, I can't do this anymore, from the from the parents, like, I don't know how much longer I'm supposed to live, without sleep, without this, without that. And I'm like, Yeah, you gonna do it? Like, so, I mean, I'm not saying your attitude, you know, makes it better, but you got to get past the part where you're like, I can't, because it does.
Jesse 39:57
I mean, yeah, I think the attitude is. Is, like I said, kind of going back to grounding and putting things in perspective. Like the attitude is key. Yeah, I find, like me and my wife, we kind of like trade off, you know, she has bad days, and it's like, this sucks. And it's like, all right, I got it. I'll deal with it tonight. Where, you know, I have bad days, or just came home or something, and she has it. So, yeah, the attitude is key. But I think, like, personality goes into it for her a lot. She is, like, there's a control factor. And when she doesn't have control it, it's very hard for her. You know, in talking to her teacher, the social worker and the nurse, the nurse wasn't on the same page, but at least the teacher and the social worker is like, she needs to be independent. She can do this on her own. Let her do this on her own, and gave her carte blanche. Everything is yours. And nine years old, she's she's rocking it.
Scott Benner 41:06
How are outcomes like, what's her? A 1c like, in
Jesse 41:10
February 23 she was diagnosed. She was a 12.8 in May of 23 she went down to a 6.8
Scott Benner 41:19
and then we were, like, couple visits
Jesse 41:21
in between. We're 646364, and then our latest visit, which was last week, couple days ago, actually, was a 6.5 so she went up by point
Speaker 1 41:33
one. Oh, she's doing terrific. She's doing that by herself, mostly herself, 100% Oh, geez,
Jesse 41:39
she has brought up, like, you know, the nurses have said things to her, like, you shouldn't have just juice. You should stabilize, you should add protein and protein to help stabilize your sugars and whatnot. And it's like, I see your point. You know, like to the Brianna's like, no, that's not how you do it. I gotta have fast acting carbs, and then they're giving me additional carbs and proteins on top of the juice, and it's causing me to go high, and my pumps doing corrections, and then I'm hitting the low an hour, two hours later. Because what
Scott Benner 42:15
kind of pump is she using? The
Jesse 42:17
OmniPod five. The OmniPod, we have it set almost as aggressive as you can. We're constantly in a state of flux where we're adjusting stuff. But I would say her Target's 110 her ratios are pretty aggressive. Correction factors aggressive, like we're pretty aggressive with things. But at the same time, you know, the endocrinologist says don't correct Under this circumstance, and she has followed her guidance, which is awesome.
Scott Benner 42:49
Yeah, wow. So do you think that having it, the management on her is part of her burden right now, or do you think she's okay with that part of it, and it's more about the outside forces?
Jesse 42:59
So she's only been managing for completely by herself about a month, and it's been like night and day, much better for her. The flip side is she's still nine, so she's a kid, and she'll forget to dose, she'll not do a correction. You know, some of those things that you would expect of a nine year old. So I
Scott Benner 43:26
bet she also doesn't like being told what to do by the nurses, especially when they're not right, too.
Jesse 43:30
Yeah, like that. That was probably the biggest factor for her mental health. I mean, she and I didn't really see it as a father for a while, as to how defeating or annoying it was to her. It it truly bothered her. Yeah, now that she's doing it and she has more confidence, she feels better about herself. Every aspect about it thus far has been when we last week, when we met with the endocrinologist, the social worker, the first thing the social worker said to her was, you know that you don't have to do this all by yourself, right? And she's like, No, I know. And she's like, you know, there are people to help you, right? And she's like, Yeah, you know, like, sometimes I forget, and Mom and Dad help me. Sometimes mom and dad ask me, you know what my number is. You know, different things like that that, you know, it's
Scott Benner 44:31
most important that she just realizes that there's someone there, not maybe so much that she has to actually take them, take them up on it all the time. I think maybe just knowing it's there is valuable
Jesse 44:41
100% because she would take it on herself if she could 100% you know what? I mean? Yeah,
Scott Benner 44:48
it's something super well. You know, I just put out an episode today. It's the first of a four part series with Erica about resilience. We really dug into what like. Being resilient means, and how people end up in that situation. And it's not as clear cut as I think we make it out to be. It's pretty it's really very interesting. A lot about like, what's happened to you in the past, how you face things, you have a much better chance. There's this list. It's called, like, the ACES list. I'm gonna do a lot of this off top of my head. But for people who have lived through certain issues, they have different challenges, physical, sexual, verbal abuse, physical emotional neglect, living in a household with mental illness, growing up a parent who's addicted to drugs or alcohol, if someone in your home has been imprisoned, witnessing abuse, losing a parent to divorce, separation or death, like these things all impact how you manage like stresses and how resilient you actually are as an adult. It's super crazy and interesting, and it's very often not up to you, yeah, so we spent a lot of time picking through it. It's interesting because you describe you and your wife is very type A, yes, you know, like, and so your daughter, I guess, likely, is too like, even that's what I hear, which doesn't want the nurses to tell her the wrong thing. Yep, you know, a lot of people, they'll just listen to authority and do what they're told, and if it's wrong, they'll go, well, they were wrong, not me, and then it's all gone. But she doesn't want someone else in control of it. She doesn't even really want you guys in control of it. It doesn't
Jesse 46:30
sound like, no, yeah, and it's and she, you know, as a kid, it's tough, because she she has to balance the listening to authority, and she, 100% wants to do that, and does that because she has those values and everything else. But at the same time, she also wants to control to or at least, like you said, if they're doing something wrong, she just, more often than not, will take it and listen to the authority, and that would make her feel worse, because she feels like
Scott Benner 47:05
she knew the right thing to do, right? And she's not in control. Well, this is, this is very new, developing, to say the least, for you guys,
Jesse 47:13
resilience is a, I think there's like, certain key words, like, you know, putting things in perspective, resilience, patience would I don't like I think resilience is probably the best word, but to be that way, like you said, I don't I think your life experiences helped you to do it like I find it
Scott Benner 47:33
after having the conversation with Erica, it's largely not up to you how resilient you are.
Jesse 47:38
Like my mentality is adapt and overcome. You just gotta do it, unless it comes to my kids, right?
Scott Benner 47:46
But do you, can you look back on your childhood and figure out where that comes from?
Jesse 47:50
Yeah, like, it's definitely your upbringing. I think, like, my father was tough. He was definitely disciplinarian kind of thing, authoritarian, but he, he also very much so challenged us. Everything was, you know, trying to figure this out and do well. And he pushed us to do well, motivated. So I think that it kind of put you on that track. Yeah, you're kind of put in a position where you have to do it, right? I think, you know, like, I hear it a lot at work and stuff like, Gen Z, Gen X, you know, different. The word is, like, it's just a different breed. I don't completely subscribe to it. It's, it's true, like, it generational differences is, you know, there's clearly differences, but I think part of it is the world and how they're growing up today is different than when we grew up, you know, like, just think of like the playgrounds when we were kids in 1980s the playgrounds at school were considered death traps in the 1980s and I wouldn't go out and play without getting like a splinter or banging your head on a metal bar or something like that. Whereas today, everything is padded and low to the ground and, you know, just super, super safe that it's, you know, it's almost like, over compensation. It doesn't allow kids to to learn.
Scott Benner 49:28
Yeah, I wonder how, how that's going to change, because your daughter's a completely new generation now. I mean, at eight years old, you know, and your son even at five, like, right? Like, where does this like? Because they, they're going to fast forward through so much stuff, like things that we would have spent years adapting to, they learn about, get thrown into, figure out and move past, sometimes in weeks, it's kind of fascinating. Like, I think it's gonna overall make people more capable, you know, but like. In those in between generations, for the people who weren't accustomed to it, it was a big shift, yeah, like, a, like, a really, really big shift. I feel lucky that I paid attention to technology early on in my life and I kept up with it, because I think that keeps me, like, nimble. And like, you know, I see something new, and I'm like, Ah, that won't work. But then you see another thing. You go, that's a good tool. I should learn how to use that. Then you use it, you learn. Then you have to be careful. You don't start learning so many things that actually, you can't actually apply them. And then when I kind of explode that out into real life, like, I wonder how many things kids are taking in that are valuable, and how many things they're taking in because it's in their face, and you feel like, oh, I need to learn this new thing. But it really, it won't hold any long term value for you, right? It's super interesting. Like, I mean, like, I can't wait to do this podcast for 10 more years and talk to like, your daughter 10 years from now, like, and see where she's at, because she's probably going to be fine. And you'll realize that a lot of this was just necessary to have happen, and that the real key to the whole thing is to not get stuck in one place, like not hit quicksand and think, Oh, God, this problem right here is gonna define us, and then you worry about it so much you can't get past it. You know what? I
Jesse 51:19
mean, yep, and I think for her and people growing up, you know, today, it's the management tools are changed, evolving and changing so much that it's like all these tools or resources are available, at least for the physical part of it. I think the mental health side, it's tough, like, there's not a ton out there for the mental health aspect, yeah, but I take
Scott Benner 51:45
your point with kids. Think about this though 30 years ago, an eight year old type one just had diabetes for a year, could not have said I have a mid six, A, 1c that I manage on my own. And my biggest problem is that my nurse doesn't understand fat and protein and how it pushes up my blood sugar later, and how to mean those people were back there going, Oh, the doctor told me I'm gonna die in my 30s. So I
Jesse 52:12
mean, like the management's evolving so quickly that
Speaker 2 52:16
her and even new generation, it's like they're gonna have different experiences,
Jesse 52:21
and it
Scott Benner 52:22
should allow them to focus more on the mental health side of diabetes, which might be one of the might end up being one of the more, like, unsung heroes of the technology, like, you know, like we think about it, and all the other aspects of life, right? Like your car drives itself. You don't have to do this. You're you know, this does that like, you know, takes this load from you. What do you do with that time, once the the load's been taken away? And I would say that type ones, historically, are so busy keeping themselves alive in the moment, they don't have time to think about big picture stuff. And maybe now they will like, maybe now you can throw in an OmniPod, five, an eyelet pump, hand them something or other, like, you know what I mean, and let the thing run your A, 1c, in the sixes. You figure out the nuts and bolts of it. You move past that part, and now you have, like, time and bandwidth to think about the other stuff. Like, you know, and maybe you you'll end up with a more complete person at the end because of that, set it and forget it. You know, hopefully, hopefully they, some people figure it out. Like, I mean, it's not always. I don't see how it can be perfect ever, but, you know, right now, but the algorithms are insane. Like, I'm updating Arden tonight to another algorithm. So, you know, she's been using Iaps. Now she's going to move on to a different one. I love seeing where all this stuff goes and and, and what it lends you back, like, that's the part, man, that like what it gives you back in time and again, bandwidth. I don't think we're even up to appreciating that all yet. You know what I mean, even just like people use the GLP medication, they don't use as much insulin. You think, oh, there's great reasons, like, you know, to not use as much insulin. But how about, like, you know, removing acne or PCOS problems for girls, or, what about just use less insulin? You know, fewer insulin units, fewer lows, less three pound highs from medications like that kind of layer from eating and trying to stop below, like, all of that stuff just removes a layer of complexity, like, over and over and over again. Yeah, anyway, I want to keep doing this. I think the stories might be even crazier. 10 years from now,
Jesse 54:37
you had the one person on who I forget that you brought back. And I don't know if she was an exchange student, and I forget her name, but it was interesting to hear her story, like four years later, or whatever. I think you had her on, initially, a diagnosis, and then like, four years later, where she was, was
Scott Benner 54:54
it from Russia? With sarcasm, yes, yes. Yeah.
Jesse 54:58
That was really cool. See, because, like, you got, you know, the real life version of where they're at. And you know, some things are good, some things are bad. You just, you just deal with it, and, you know, you move on. But no, I
Scott Benner 55:11
agree. Even cool, she had, like, a tragic, personal yep thing happened in her family. And even though you could tell she's dazed from it still. Yep, she's moving. She's still moving in the right direction. And and, you know,
Jesse 55:27
hearing those stories like it's it's huge, because, like, you know, other people can relate. The beginning of her story
Scott Benner 55:35
is crazy. She lived in Russia when she was diagnosed. She's in, I think she's in America at college now, she didn't have access to a lot of the tools and or anything. She didn't really know what she was doing so well. You have to go back. It's called From Russia with sarcasm. She's like, 14 when I'm interviewing her, and she found by herself the podcast figured out all the tools she needed to take good care of herself at 14, went to her parents and said, I need you to find out how to get me an OmniPod and a CGM. And, like, she, she basically tasked her parents with, like, Fine, get these things for me in a country where they were not particularly available. They sourced the things for she puts her a 1c crazy good, takes care of herself completely. And then, you know, like, just has the greatest outlook on things,
Jesse 56:24
that is Brianna. Brianna is very much, here's what I need. This is, you know, and what's interesting to me is, you know, in the beginning, she was, I wouldn't say, showing stuff off, but she she had no shame. Then she moved into, well, you know, I'd rather not talk about it to now. I mean, she listens to your podcast regularly, like, and I'm like, I'm like, All right, Bree, let's, let's turn this off. You know, like, I'm sick of hearing Scott's voice. Let's turn this off.
Scott Benner 56:58
Listen. You can turn the volume down Jesse and let it finish. So I get to download, you know what I mean,
Jesse 57:03
or headphones, something. But, you know, like
Scott Benner 57:06
to the point that, like, listen,
Jesse 57:11
as a parent, like, I think one of the struggles, you know, if somebody's so young, is balancing. It's not all diabetes, you know, let's, let's tune out. Let's go something else, you know, let's not make it all diabetes. But she's also in a place where she she wants to learn which is, which is awesome, yeah, but
Scott Benner 57:32
it's just really fantastic to think that that she might be able to find herself and her answers in other people's stories. And again, there's a thing technology brings to you, right? Because if you go back 1015, years, I don't think in a lifetime, you could meet 1000 people with diabetes and hear their story. You know, 10 years ago, how would you do that now? You just like, you know, subscribe to a podcast. People will ask me times like, Why does it take so long to get on the show? Well, when you stop and look at Jesse's note, I'm going to read your note. Keep in mind it's not even the one you probably started out writing, probably not newly diagnosed child. Resources, support. Learning diabetes is tough, but the emotional aspects is being missed. Everyone is in a state of trauma, and they just react for good reasons, but the mental health element is absent, then navigating these emotions and learning diabetes as time progresses, does the trauma ever end for the child and for the parents? Also, I have to navigate schools and camps. It keeps kids safe, and that was probably written six months ago. You're not even that person anymore. Yeah,
Jesse 58:38
I remember it. I definitely remember that stage, but it's not the part you're in now. We're not trauma, we're not screaming at everything. Yeah, it's definitely different.
Scott Benner 58:49
Yeah, that's the lesson, Jesse. And one of the reasons why it takes six months to come on the show, because you'll actually have something to talk about when you get here, and then this will sit and marinate for months before it goes up, and when you hear it back, I guarantee you'll listen back and think I'm not even there anymore. Like and to me, that's the takeaway for people, is that, you know, train keeps on rolling. I think the biggest mistake people make, and if it's a mental health issue, sometimes it's not a mistake, it's just what happens to you, but it's that getting stuck in the mud and then not getting away realizing that this thing, as important as it seems at the moment, with just a tiny bit of hindsight, will seem irrelevant and just be a small portion of like, my perspective, and not the entirety of my life,
Jesse 59:33
going back to that, that word perspective, I think for me, that's it's huge, because there are many, many moments that are muddy and challenging, and whether it's nighttime lows or just a stubborn high, whatever the case may be like, there's there's moments that are challenging, but the overall perspective and the overall. Overall, like, you know, just moving in the right direction. It's, you know, we're only just over a year into this, and that journey over the past year has been, it's been a roller coaster, you know, looking back at it, but it's, you know, we're still riding it. And it's, it's one of those things that I think when I wrote that note, one of our challenges was the support, you know, just getting her connected with, like a mentor or other kids that you know, she can share, and she has a couple of friends you know who've been diagnosed that she's met along the way, one at camp, a couple at the walk and different events, but nothing close and personal. And I just think she's not ready for it, or maybe it's just not the right connection. But she does occasionally text, you know, all three or four of them with, you know, notes like, Hey, how are things? Check out, you know, screenshots of her sugar pixel or whatever, and different things that, like
Scott Benner 1:01:04
they do talk, but,
Jesse 1:01:06
you know, not super often, but I think she's missing. She was missing, and now is getting connected with like she tends to connect with older girls that share what they have, and she views them as kind of like an authority figure, or like somebody with knowledge that she wants to learn, or, Hey, that's a cool teenager who's who knows, and it's not mom and dad. I think that will be really helpful for our doctor's office actually has just connected us with somebody that, hopefully that works out well for her. She's also the type that wants to be the the ambassador, you know, that wants to teach others.
Scott Benner 1:01:47
And if she can't find those people, she always has a 52 year old guy with a podcast she can listen to, which I think is just a very crazy pairing. But
Jesse 1:01:57
I tell you what, though, like it, it helps. Like I don't, I wouldn't know what it feels like to be in her shoes with the constant Bree, what's your sugar? Brie, did you dose? Bri, you're really high, you know, like it's constant. And me, and me and my wife try
not to harp on that stuff.
But we're also type A and we kind of, we try to stay on top of it as best we can, yep, without harassing her. But you know, it's, it's that balance. And I think by her taking ownership and listening on her own and really wanting to and doing it on her own is pretty cool.
Scott Benner 1:02:39
Well, Jesse, it sounds to me like you guys are doing really well in my questions. Like, my question would be, just, does it feel that way? No,
Jesse 1:02:47
no. And that's, that's the tricky part. Like, I honestly, and I can't say no, like we, we are definitely moving in the right direction. But it's, it's like, one step forward, two steps back kind of thing. You know, there's been some other things that I would say, mental health wise, are not diabetes related, pre diabetes, like, we had her connected with a counselor for like, you know, at three years old, like, she would hit herself, you know, just saying, like, I'm I'm no good, and would hit herself when we'd say, hey, Bri, can you please clean your room up a little bit of it? I'm just no good. And she would hit herself kind of thing. And it's like so that kind of stuff, you know, has nothing to do with diabetes, but I think the diabetes definitely amplifies things to the nth degree.
Scott Benner 1:03:37
May I suggest Jesse to take a cue from your medical stuff and make sure they're tracking her TSH and her thyroid stuff too. So
Jesse 1:03:46
that was just included in her recent orders. I'd have to look back to see if it was ever previously tested going forward, yes, yeah,
Scott Benner 1:03:55
just because some anxiety and even like personality stuff could be thyroid related mood swings, yeah, yeah, for sure. Just keep that in your head. That's all absolutely yeah. And it also, by the way, a well regulated thyroid makes blood sugars easier to manage, too. That's
Jesse 1:04:12
interesting, yeah. So, I mean, what like, there's a pretty good percentage of diabetics who have Hashimotos as well, right?
Scott Benner 1:04:21
I mean, I don't know what it is, but when somebody tells me they have type one and Hashimotos, I don't go, oh, gosh, really, that's crazy.
Jesse 1:04:30
It's, it seems to be a more common theme,
Scott Benner 1:04:33
yeah. I mean, autoimmune can run in families, and it doesn't always have to be like, I have type one. So you have type one, it could be a number of different things. It just can't. I mean, it's clearly in my family, my daughter's got issues that, you know are not are more than type one. My son has Hashimotos. My wife has thyroid, you know, like, my son will talk sometimes about, like, I'm cold, you know, even though he's really good with his medication is and his TSH levels are great art. Is exhausted without a cytome supplement to her t4 supplement when she's taking her thyroid medications. She definitely is hypermobile to some degree. She's creaky and cracky and stiff and, you know, joints ache at times, stuff like that. Probably not Ra, it's all that stuff, man, like, you know, like, you start, my wife started using a GLP, and she's like, Oh, my inflammation went down so much like just from the GLP medication. She's like, I wonder how much this inflammation is just impacting my life. And I, I 100% take her, you know, at her work,
Jesse 1:05:35
I describe my autoimmune as to sum it up, it's an inflammation disorder.
Scott Benner 1:05:40
No, what it is, yeah. I mean, everything's just essentially there. Listen, this is completely unfounded. Then I have to let you go, okay, but there was a time where there were people running around the diabetes community and they were saying, your beta cells aren't dead. They're just frozen there. There's no room in there, so they can't move. I forget the exact way it was put, right. And now, tomorrow I have an episode coming out with a 50 year old, eight year old type one, who took Manjaro for weight and for insulin resistance, and it works so well for him. He's not on insulin anymore. Like I don't even know what to say about that. Like I'm not drawing a conclusion from it, even I'm just telling you, 50 years old, diagnosed, if I'm remembering his timeline right, he honeymooned for a while, four or five years, then for the last couple years, then the next couple years, like heavy usage of insulin, right where you would expect. Then they put him on manjarno, and he does not use insulin anymore. And he's got auto antibodies. He has type one diabetes, and he'll very likely need insulin again at some point in his life, but for the moment, he's not using it. That's very interesting. Ridiculous. Like a 15 year old girl a couple months ago, her mom came on. She's gone from 70 units a day down to four, and doesn't bolus for meals anymore and took off her pump. Yeah, so I
Jesse 1:06:57
don't know, man, that's impressive. I mean, the thing the amount of studies that are going on now, like you can only hope it's very positive. Gonna figure
Scott Benner 1:07:06
a lot. It's not everything's not gonna work for everybody, but some things are gonna work for a lot of people. And that's that's where you wanna be excited and have people continuing to look Jesse, I'm gonna say thank you right here. This is a great time to stop. I thought you were fantastic. I say this every time after I speak with someone like you there. If there are more men out there in touch with their feelings, please reach out to be on the podcast. I'll even talk to you guys that aren't you're fun too, but I don't get as many men, so I appreciate you reaching out. I really do.
Jesse 1:07:36
Also, I could say is I'm definitely, typically not the emotional person. But in this topic, in this realm, it it got me, diabetes
Scott Benner 1:07:45
brought you there, that's for sure. It got me, yep, let me ask one last question. Is there value in that for you? Like, if you can, like, let go of the part that diabetes is what brought it here. Like, are you happy that you have these connections now, or are they hard to deal with.
Jesse 1:08:01
I think it's one of those things, like, as I get older, you appreciate more and you understand more, and you kind of just, you comprehend it better. But I'm not an emotional guy, so it's not comfortable for me. It's not my wheelhouse. It's not like, you know, I don't enjoy having the, you know, range of emotions, or, you know, whatever it's, it's, it's typical. It's not typical of me, but at the same time in the realm that it's happening, and truly wrapping your head around all that's going on, it just gives you a better perspective. And you just, like, for me, it's, it's a growth type thing, like I'm at that age where you just, you learn from it, you appreciate
Speaker 2 1:08:44
it, and it's, it's helped me.
Jesse 1:08:49
I mean, if I were to take it back, I guess I would probably go back and say no, no emotion, and just get things done and do it my typical way. I think there's no other way for me. Okay, best way to put it,
Scott Benner 1:09:04
oh, that's very honest. I appreciate that. Thank you. Wow. All right, hold on one second for me, but you were terrific. Thank
Unknown Speaker 1:09:10
you. Appreciate it. Good
Scott Benner 1:09:11
times. You
a huge thanks to cozy Earth for sponsoring this episode of The juicebox podcast. Cozy earth.com use the offer code juicebox at checkout to save 40% off of your entire order. This episode of The juicebox podcast was sponsored by us Med, usmed.com/juicebox or call 888-721-1514, get started today with us Med, links in the show notes. Links at juicebox podcast.com a huge thank you to one of today's sponsors, gevok, glucagon. Find out more about Chivo hypopin. OmniPod at gvoke, glucagon.com. Forward slash juice box. You spell that, G, V, O, k, e, g, l, U, C, A, G, o, n.com. Forward slash juice box, if you or a loved one was just diagnosed with type one diabetes, and you're looking for some fresh perspective. The bold beginning series from the juicebox podcast is a terrific place to start. That series is with myself and Jenny Smith. Jenny is a CD CES, a registered dietitian and a type one for over 35 years, and in the bowl beginning series, Jenny and I are going to answer the questions that most people have after a type one diabetes diagnosis. The series begins at episode 698, in your podcast player, or you can go to juicebox podcast.com and click on bold beginnings in the menu. If you're not already subscribed or following in your favorite audio app, please take the time now to do that. It really helps the show and get those automatic downloads set up so you never miss an episode. Thank you so much for listening. I'll be back very soon with another episode of The juicebox podcast. The episode you just heard was professionally edited by wrong way recording, wrongway recording.com, you.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#1349 Cross That Bridge
Becky is the mom of a 21 year old type 1 who also has high functioning autism.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
We're back together, friends. This is the next episode of The juicebox podcast.
Becky is 53 she's the mother of a 21 year old, type one, who also has high functioning autism. Her daughter was diagnosed in 2023 the education they got at the hospital wasn't great, and the way they found the podcast is a story in and of itself. Nothing you hear on the juicebox podcast should be considered advice medical or otherwise, always consult a physician before making any changes to your health care plan. Don't forget, if you're a US resident who has type one or is the caregiver of someone with type one, visit T 1d exchange.org/juice box right now and complete that survey. It will take you 10 minutes to complete the survey, and that effort alone will help to move type one diabetes research forward, it will cost you nothing to help to save 40% off of your entire order at cozy earth.com All you have to do is use the offer code juicebox at checkout. That's juicebox at checkout to save 40 percent@cozyearth.com if you're looking for community around type one diabetes, check out the juicebox podcast, private, Facebook group juicebox podcast, type one diabetes.
This episode of The juicebox podcast is sponsored by the continuous glucose monitor that my daughter wears the Dexcom g7 dexcom.com/juicebox gets started today using this link. The episode you're about to listen to was sponsored by touched by type one. Go check them out right now on Facebook, Instagram, and of course, at touched by type one.org check out that Programs tab when you get to the website to see all the great things that they're doing for people living with type one diabetes, touched by type one.org
Becky 2:05
Hi. My name's Becky, and I have a 21 year old daughter named Kara, who was diagnosed July 5 of 2023
Scott Benner 2:14
July 5 2023 Oh, my goodness, just about a year ago. Yeah, almost a year okay, and she's 21 now she's 21 now she was 20 at the time. So I'm not going to stretch this part out too long. You don't usually get a mom on to talk about their adult child, but there's a reason for this, right?
Becky 2:32
Yes. Okay, so my daughter is on the autism spectrum. She's high functioning, yeah, when you say adult, she's definitely adult by age, but not quite there where she can really be by herself at this point. Still needs a lot of guidance,
Scott Benner 2:47
okay? And what made you want to come on the podcast? I just kind
Becky 2:51
of wanted to talk a little bit about, you know, when you're diagnosed as an adult, even if you don't have, you know, any kind of other issue or disability. It's not really always, you know, they treat you like an adult at 18, but at 18 or 20, or however old you are, you still need to learn about this disease. I mean, it's or this diabetes. It's very confusing. And I think if you are not mentally or mature enough, I think that you need a lot of support, and you don't get that in the hospital. And we found that out being diagnosed as an adult, even with her being on the spectrum, it was, it was a nightmare, really.
Scott Benner 3:34
I think that one of the reasons that people like the podcast or the way I talk about diabetes is because the way I talk about it is set up so that Arden can understand it without understanding it correct. Because she's like, she's 20, and Arden's a bright, thoughtful person, etc. But if you really pin her down about diabetes, she's like, I don't know, like, you know, and she manages a low six, A, 1c, at college by herself. That's amazing, yeah, and it's all just because I don't know, I've t shirt slogan her life, the way I've done the podcast. I'm like, you know, like, you know, pre bolus, and don't get high, you know. Like, well, how do I not get high? I'm like, just don't get high. Like, bolus, see, you don't get high. And if you get high, bring it back down real quick, and, and, but don't get too low. So you have to stop it before it gets back down. Like it's not there's nothing technical about it. I think that works really well for her. And then somehow it translates well out to people that I I'm speaking to that can't hear me, but I take your point, like they just sort of blurt the stuff out to you, and then that's it. They're like, Well, we said it now, so go ahead, right?
Becky 4:41
Yeah. And if you're like my daughter, you know, she's very black and white. She doesn't read between the lines on anything. And you know, she takes everything. What you said is what is to be done, right? I mean, I guess in one on one hand, that's a good thing, because she likes she's a rule follower. So, you know, she will follow. The rules, but yeah, she needs to know step by step. It's not like, Oh, do this or here, don't do that. It's, she's more rigid, I guess she should say,
Scott Benner 5:09
So, once you've got it set up, she's okay, yeah,
Becky 5:13
once you've got it set up, she's okay. Like, she's doing really well. Now she she counts her carbs and she well, okay, for first, let me just say we're on the Dexcom seven, so we've been manual and the OmniPod five. So we've been manual since she got a pump, because they don't talk to each other yet, right? So we've learned how to do everything manually, and that's how she knows how to do it right now, until, until the two of them are, you know, interfaced together, I guess. So she's good about, you know, counting carbs, putting it in the PDM is still getting the point where, if she starts heading up, you know, we still have to step in and go, Hey, you know you're getting up, you probably should give yourself some more insulin, catch it before it gets too high. And she's getting better about that, I think a little bit in her mind. She says, Okay, I gave my insulin for this amount of carbs, this is what I gave. I'm good. She expects it to work, right? Yeah, she she did the work. She did what she was supposed to do. So it's all of that, you know, hey, it's heading up, and she is getting better about that now, like, I give her props. Like, pretty much during the day, we don't really bother her. You know, she handles it all during the day pretty good, unless she stayed high for a while, then we might say, hey, you've been high for a while, like, you probably need to, you know, give yourself some insulin, and she'll be she'll usually say, Hey, I've already done it. It's just not coming down. I'm not sure why. So, yeah, for for us to be just a year in and her to be on the spectrum. She's doing amazing. I think,
Scott Benner 6:42
yeah, no, she it sounds, it sounds like, it like, so what happened in the very beginning that made you feel like, oh gosh, here, here are the problems. What was happening that made you go, there's insufficiencies in what we're doing. The Dexcom g7 is sponsoring this episode of The juicebox podcast, and it features a lightning fast 30 minute warm up time that's right from the time you put on the Dexcom g7 till the time you're getting readings. 30 minutes. That's pretty great. It also has a 12 hour grace period so you can swap your sensor when it's convenient for you. All that on top of it being small, accurate, incredibly wearable and light. These things, in my opinion, make the Dexcom g7 a no brainer. The Dexcom g7 comes with way more than just this, up to 10 people can follow you. You can use it with type one, type two, or gestational diabetes. It's covered by all sorts of insurances. And this might be the best part. It might be the best part, alerts and alarms that are customizable, so that you can be alerted at the levels that make sense to you. Dexcom.com/juicebox, links in the show notes, links at juicebox podcast.com, to Dexcom and all the sponsors. When you use my links, you're supporting the production of the podcast and helping to keep it free and plentiful. I was looking for a way that we could all get nice and tanned and meet each other and spend some time talking about diabetes. How are we going to do that on a juice cruise, juice cruise 2025 departs Galveston, Texas on Monday, June 23 2025 it's a five night trip through the Western Caribbean, visiting, of course, Galveston, Costa, Maya and cozmel. I'm going to be there. Erica is going to be there, and we're working on some other special guests. Now. Why do we need to be there? Because during the days at sea, we're going to be holding conferences, you can get involved in these talks around type one diabetes, and they're going to be Q and A's plenty of time for everyone to get to talk, ask their questions and get their questions answered. So if you're looking for a nice adult or family vacation, you want to meet your favorite podcast host, but you can't figure out where Jason Bateman lives, so you'll settle for me. If you want to talk about diabetes, or, you know what? Maybe you want to meet some people living with type one, or just get a tan with a bunch of cool people. You can do that on juice cruise 2025. Space is limited. Head now to juicebox podcast.com and click on that banner, you can find out all about the different cabins that are available to you. And register today. Links, the show notes, links at juicebox podcast.com, I hope to see you on board.
Becky 9:27
Well, I mean, I think it just started with the whole hospital setting, you know, we went, we went into the hospital. So I'll give you a little backstory. So she, she had been complaining of, you know, and I don't, I didn't know much about diabetes. I do have a girlfriend whose son was diagnosed when he was 12, and I just vaguely remember her saying that he was he drank a lot of water, and that he was fatigued a lot when they had found out. So that kind of somewhere in the back of my mind. But she had been complaining of stomach ache for like, three months. She complained that her stomach hurting, and she had ran in. Only thrown up a couple times, but she had just started working at my husband's company, and she was working in the warehouse, and it's hot, you know, it's, we live in Florida, so it's very hot. Yeah, she was drinking tons of water. She was coming home fatigued, she was losing weight, but to be honest, I was contributing all of that to her being in the warehouse, you know, because she went from this kind of sedentary, didn't do a lot, to being in this hot warehouse. So I was just kind of attributing it all to that. So finally, I took her to the pediatrician, and I was like, you know, she's playing on her stomach hurting. It's been going on for a while. I don't know what's going on. They were just kind of like, well, oh. And so backstory, my daughter is deathly afraid of needles, like we couldn't even prick her finger, like when she would go for the like, for her normal, you know, checkups, trying to give her a vaccine or any kind of shot. I mean, got, I mean, holding her down, screaming, craziness, right? It was just crazy. Okay, so when we went to the doctor, she didn't prick her finger or anything. She just said, Oh, she probably has acid reflux. And so she gave her a prescription for acid reflux medicine. And then she said, and I said, Well, anyway, we can get her blood work done. You know, she hasn't had it done since she was little, because she refuses to, you know, go around any needles, yeah, so she gave us blood work to get done. And I kept telling Kara, well, she we got the prescription filled. She took that a couple times. She said, That's not helping. That's making it worse. And I said, Well, you need to go get your blood work done. And she's like, No, I'm not doing it like she refused, refused to go get it done. So three months goes by. That was in April, in June, we went to we went on a cruise. While we were on the cruise, she was sleeping constantly. She was eating like crazy, drinking tons of water. We were with another couple family friend of ours, and I said to them, you know, if I didn't know any better, I would think she has diabetes. And we all went, oh god. Wouldn't that be awful, considering how much she hates needles, right? We were like, oh god. So we just kind of put that out of our mind and went on whatever that was. In June we got home, July 4, we had went to a cookout at some friend's house, and we came back home and she laid on on the couch. She's like my stomach hurts. Of course. She had macaroni and cheese and bread and all this stuff. So I said, Kara, I don't know what to tell you. You know, you won't go get your blood work done. I don't, I don't know what to tell you. You know, I was getting, actually getting a little frustrated with her. I'm kind of, I feel bad now, but I was, like, frustrated with her because, like, I can't help you if you don't want to do what the doctor says. So the next day, July 5, she was still complaining of her stomach hurting. So I said, Okay, I'm just taking her to the emergency room, because I know my kid. I knew that they were going to have to, if they, if they took her in, they were going to put an IV in. And I thought, we can get all the tests done after they get that IV did anything that might be going on, I won't have to, you know, keep taking her back and forth to get blood work done. And so I took her to the ER and told them what was going on. And they were like, she looks fine. And I'm like, Yeah, well, she's been complaining of stomach hurting. And I told the doctor. I said, if I didn't know any better, I would think she was diabetic. They just kind of gave me the stare, like, whatever they went to put an IV in. Of course, my daughter freaked out. Said 20. So acts like a toddler when it comes to, you know, any kind of needles. So we kept telling them, like, Hey, you probably need to give, like, give her a valium or something to calm her down. You need to, like, give her nummy medicine on her arm, like anything that you think might help, because she's going to give you trouble to get the IV in, right? And they finally did. They finally did. It took like, three nurses to hold her down to get it in. So finally get the IV in, and then the doctor comes back, like 45 minutes later, after making the blood work, and says, Oh yeah, she's diabetic. She's in DKA, and were sent her to the ICU. And I was like, what?
Scott Benner 13:43
So they took you seriously when you said that, yeah, they
Becky 13:47
took you seriously. But then, well, sort of, she kind of looked at me, like, okay, whatever. And then when she came back, then she was like, oh gosh, you know, you were right, and sent us to the ICU. So anyway, needless to say, while we were in the ICU, it was a nightmare, just because of, you know, all the shots, you know, them coming in and pricking her finger and every hour on the hour, and all the different IDs they had to put in. It was a nightmare. But I kept saying, hey, like, we don't know anything about diabetes. Like, is there, like, an endocrinologist that we can talk to? Is somebody going to come in and talk to us about this? You know, are we going to get any education? And they kept saying, yeah, yeah, somebody will come in, yeah, we'll send in a nutritionist. And finally, a couple days later, they sent in a nutritionist, and then she sat us down, and we were like, she told us, like, she can't have canned vegetables anymore. She can't have this. She can't have that. She was just going. They were candid.
Unknown Speaker 14:41
Yeah,
Unknown Speaker 14:42
actually, vegetables. Becky, can
Scott Benner 14:44
you give me a second here?
Unknown Speaker 14:45
Sure.
Scott Benner 14:45
I'm gonna ask a question. Don't be insulted. Okay, no, are you? Are you nervous
Speaker 1 14:51
a little bit? Do you have ADHD? I do not. Okay,
Scott Benner 14:56
I'm gonna tell you. Why
Unknown Speaker 14:59
am I speaking? Really fast.
Scott Benner 15:00
I don't know what the we're talking about. Gosh, that does not happen to me that often you're doing that thing that. Have you ever seen Donald Trump's speeches in writing? No, he starts and stops and starts and stops and starts and stops like, he'll go like, I don't know exactly what I'll say, but he'll be like, I'm here today to talk about this dog actually, you know my wife, she had a cat and like, and then you're like, we love pets. When I say we, I mean my husband, I'm like, and I'm like, What the was the first thing he was gonna say and then, but when you hear it, it sounds right, like, I know that's a weird thing. Like, when you I'm using is a bombastic example, but when you listen to him, you go, like, I know what he's saying. Like, like, I understand what he's trying to say. But if you look at it in writing, it's disheveled at best, and I feel like you're jumping around like that. I feel like we're on a roller coaster and watching Pulp Fiction at the same time. And Vincent Vega is alive. He's dead, he's alive, he's dead, he's alive, he's dead. I don't like if I asked you one question, yep, I asked you, what has happened that made you feel like what you were doing is insufficient? Do you think we've answered that question?
Becky 16:10
I guess not. What I mean, not so much, what I'm doing is insufficient. I think the education that we received, or the lack of education that we received when we were in the hospital because she was diagnosed as an adult, right? You know, I hear on your podcast a lot that people that you know, the kids that are diagnosed younger, they're at these children's hospitals, and, you know, they get all this education, or a lot more education. I
Scott Benner 16:34
see what you're saying. So, because she was an adult, yeah, because she was an adult, but she doesn't absorb things like an adult, correct? She got that crappy adult hospital education that we hear about so much they're talking to her, but the truth is, is you basically are the one that's gonna have to still understand it, and it's very incomplete, and then you go home. Okay, correct? I'm happy to go back to that. We are so far into what I think is her diagnosis story that I want to keep going with it anyway, but I want to get you
Becky 17:06
back. Sorry. Yeah, so I guess my guess, what I was trying to get to is, while we were in the hospital, we kept asking for education, and we and they knew that my daughter was on the spectrum, and we kept saying, you know, we need to know what to do when we get home, you know, and but they kept speaking to her, obviously, because she was 20, and even though we have her sign a paper saying that, you know, we have, you know, rights to help her medically,
Scott Benner 17:34
yeah, that's what I'm wondering. Like no one ever just was like, hey, like, pulled you aside and said, Look, are we talking to you? Are we talking to her? No, no.
Becky 17:42
And so we kept saying, my husband and I kept telling them, like, hey, like we don't know anything about diabetes. Like, we don't, you know. We know you guys are coming in, they're pricking her finger, they're, you know, coming in and giving her insulin shots. But nobody was really explaining, like, I had no idea that, you know, it was a carb count. I had no idea that, you know, even what a what the normal range of blood sugar was supposed to be. So when we were discharged from the hospital, the only person who had come in to talk to us was that nutritionist.
Scott Benner 18:15
No canned vegetables,
Becky 18:16
no canned vegetables. Like I was like, what, you know, I to be honest with you, I just kind of ignored what she said, because I was like, she's not being very helpful. I don't even know what she's talking about. You know? I said, well, is anybody else going to come in and show us how to administer this shot prick her finger? Nobody ever came in and showed us how to do any of it until an hour before we were being discharged, I said we're not leaving until somebody shows me how to do like I don't know what I'm doing. I mean, luckily I have a little bit of a medical background, so I did know how to draw up, you know, insulin into a syringe. You know, I didn't draw up insulin at work, but I would draw up saline and things like that. So I knew how to draw things
Scott Benner 18:59
up, but I didn't really know you never stuck in anybody's arm or anything.
Becky 19:03
I never, I never knew how you know. I didn't know how much to give her. I didn't know what the fingerprint numbers meant. We didn't know any of that. And so it was just really, I guess, just really frustrated that there's not some sort of, I don't know, just a better practice around you know, younger kids, even though they're considered adults, 18 to whatever that they I'm
Scott Benner 19:28
gonna break some news to you here. There's not so I found that out. I found that that does not exist for reasons that I've belabored over and over again. I just did a grand rounds episode yesterday. I recorded one with, like, this fantastic person and, and I was like, so how do we fix this? She's like, I don't know. And she was like, really dedicated. Had type one understood honestly, like I was talking to the right persons. Like, what's the fix for this? No one ever knows. Yeah, I think there's a number of. Reasons for it. I do sometimes try to look at it from their perspective. Like, what if I had this conversation with the nurse who helped you, would she be like, Oh my god, there was a 21 year old girl, oh my god. She had autism, and she was like, screaming. We tried to take her blood and everything, and I didn't know what to tell her. Like, do you ever think it would be like, You know what I mean? Like, from that perspective, like, what do you do? Like, what do you do when someone comes in with a 14, A, 1c, and you're like, Listen, are you bolusing for meals? And they're like, Nah, not usually. Like, where do you start? You know what I mean. So I try to put myself in their perspective, but at the same time, they're not always talking to people who aren't going to listen. I think what ends up going wrong is that there's no there's no checklist for them to go through. It's almost like you get the information as they think, to have it fall out of their head while they're working. Does that make sense? Yeah,
Becky 20:52
that makes sense. Yeah, I did get a hold of, you know, I did do like, a big complaint the hospital, just because I I actually worked for that hospital for 15 years, so I knew a lot of, I knew a lot of you know. So I was very frustrated, very frustrated. And so, you know, I did end up going up the ladder a little bit. And somebody actually did come to my house and brought a diabetes book that they were supposed to give us in hospital that talked about diabetes. It talked about all kinds of different, you know, different food options, different different things. And she, she came to my house personally, and she was like, I'm very sorry about, you know, your experience at the hospital, you know, this book they should have given to you while you were there. She said, I went in, I talked, you know, we obviously dropped protocol. I mean, nobody even knew where these books were. She said, when they went into, when she went in to talk to them, nobody even knew about these books. Nobody knew where they were. I mean, not that the book is going to tell me everything, everything, but at least I would have felt like, okay, they're trying to educate me a little bit, you know, here's this, this book that's going to help Right, right? And she said, You know, I she, I just told her. I said, Look, I just, I don't, I don't want this to happen to anybody else. I want, you know, there to be, be a better way to go about this. I said, because our experience here was terrible between, you know, and we kept telling, you know, our child's on the spectrum. She needs different. You know, the normal way of doing things isn't going to work for her. You know, you need to listen to what we're trying to tell you, because we can make it easier for you. You know, if you just listen to us,
Scott Benner 22:28
yeah, we understand the bigger picture here that you don't get right, right?
Becky 22:31
So I do have to say that they, they did, at least, you know, they did, at least, personally contact us the hospital and try to, you know, you know, told us that because of our our experience there, they were working on, you know, a better protocol, how to a better way to do things, yeah, sure. I
Scott Benner 22:52
hear there's not gonna be war in the Middle East soon too. They're getting it all worked out. Don't worry, right? It's all happening. It's yeah, it made me feel
Becky 23:01
better. I know that. You know reality, it was. They were just trying to appease me, but it did make me feel better. I said, you know, I just don't want anybody else that comes in there to have to go through we because when we got discharged, they gave us, and I don't know how it works for Children's Hospital, Children's Hospital, but we left with no nothing. We just left with prescriptions to go get insulin, prescriptions to go get a meter, prescriptions for, you know, test strips, that kind of stuff. And before we left, I told my husband, I said, you know, before we leave, let me just call and make sure the pharmacy even has. I had to call four different pharmacies before I even found the insulin in stock. So they were going to send us home with no insulin, and I couldn't even find it at first. You know what I mean? I was like, I don't know. I just felt like just everything was so crazy and so confusing. So we had said, is there an endocrinologist that we can see? And they're like, No, there's no endocrinologist on site. I go, you're telling me there's no endocrinologist throughout your whole system that can come and talk to us. No, they don't do they don't do that. You have to make an appointment one night, when my husband was leaving and I was staying with Kara, he came, came upon an endocrinologist that was in the same building that we were in. And so he walked over there and he told him, you know the situation, what was going on? And they were, they were kind enough to give us because we said they were able to make us an appointment for a few days after we got out of the hospital, but they were kind enough to give my husband the blood work that they would actually have us draw so they were able to do it in the hospital, so we wouldn't have to go take her again for another blood Draw after we got out of the hospital to answer, you know, whatever the endocrinologist wanted to look at. So we did bring that back to the the doctor, and, you know, they were at least willing to do that while we were in the hospital. So that saved us a, you know, a blood draw you've had
Scott Benner 24:55
this experience, okay? And it's, it's impacted you, obviously, yeah. And you've had time to think about it, and now you know more about diabetes, so I'm going to turn it around on you and say, What could they have done that would have made this better for you? Well,
Becky 25:10
I think just a little bit more education in general. Tell us why. You know, they just said keeper between this number and this number, but they didn't really give us the reasons why? Why do we need to keep her between this number and this number? You know, you know, if she goes below this number, this is going to happen, or if she goes over this number, you know, you're looking at, you know, long term effects. You know, if you stay high for too long, or, I don't know, I just think a little bit more of the reasoning behind why they were doing what they were doing. And why does she get this much insulin for this much you know, I don't know. Just
Scott Benner 25:46
Can I play devil's advocate for a second? I know you will in that moment, if they would have dumped all that on you. Do you think you're on here a year from now going? They really panicked me. They told me that if her blood sugar got too low, she could have a seizure and die, and if her blood sugar got too high, she could have things like neuropathy and maybe lose her feet one day. Like, if they would have hit you with all that, don't you think you would have been like, why'd you tell me all that I was day one. I just was figuring this out. Like, my question is, is it possible that there's no way to make it good on that day? And maybe,
Becky 26:16
maybe you're right, but I feel like, because I have a little bit of a medical background. I think more that way. I think in those terms, more, you know. So I think I would have been okay with it. Maybe my husband wouldn't have been okay with it at the time. I don't know, but I like to rather know the fact, you know what I mean, like, this is why, this is what we're doing, that this is why this happens. You know, at least I'd like to think that maybe you're right, maybe, maybe I would have felt way overwhelmed if they had to throw all that you know more on me, but I don't think so. Knowing my personality, I think I would have felt better knowing the reasons why
Scott Benner 26:49
you would have been okay. Yeah, can you imagine there are people who wouldn't have been Yes, how do they know who's
Becky 26:56
I guess they don't know that. I guess you're right. They don't know that. That's
Scott Benner 26:59
the part that I think we we miss all the time. I'm guilty of it as well, because in my hindsight, I'm like, Oh, my God, you should have just told me this. You should have told me that. You should have told me this. But those are things that I even know, that I should know now because of what I went through. And I think given the totality of the situation, meaning that often those nurses are new, right? There's not a lot of like, 10 year ER nurses, right? That's a pretty, like, high impact burnout job, right? So people go in, they do it for a while, and then they're out of it. Go meet an ER nurse that's had a job for five years, and they're going to be talking about, like, I'd like to get a nice job at a pharma company, pretty much what you'll hear them say, right? I want to move some paperwork around for the FDA. Like, that's, you know, that kind of thing. So you have newer people. They don't have diabetes. Their training doesn't teach them anything about diabetes. The stuff they're telling you, if you really think about it, is just the stuff they know. Like, I know. You want to keep it between these numbers. You're like, tell me why. They don't know why, right?
Becky 27:59
Yeah, no, well, I'm learning that now. Yeah, I didn't know that then, you know, I didn't, I didn't realize that they weren't, you know, educated enough to know the whys right, you know, I just assumed they did, and we just weren't being told. I mean, I know that now, mainly just from listening to your podcast. I mean, really, we've learned everything that we know from your podcast. Well, that's very luckily enough, we found it very quickly. And that was a weird little story. The day we got home from the hospital, my husband and I were like, Okay, we just need to get out of the house for a minute. We just need a break. And so we were going around our neighborhood.
Scott Benner 28:37
Wait, hold on, how many kids do you have? Three? Three,
Becky 28:40
but she, she's our youngest. She's
Scott Benner 28:42
youngest, okay, youngest, and you've been raising her for 20 some years. Is there any chance that, like you're she's never going to not need you? No, I think at
Becky 28:53
some point she'll be able to, she'll be on her own. I mean, she works and drives and all that. So it's just maturity level, you know, she's got to get to a higher maturity level. Me too. Becca,
Scott Benner 29:03
I'm still waiting for it to happen, but, but, I mean, when you guys are like, let's get out of the house, were you like, was there? Do you ever have been
Becky 29:12
in the hospital? Yeah, been sitting in the hospital and then with, you know, it was just so crazy the whole time we were in there because of just her freaking out over everything. And we were like, Okay, we just need quiet. Like, just peace and quiet for a minute. We're gonna just go outside. And we were going around our neighborhood, and this lady was outside in her car, hood was up, and my husband's like, oh, you need help. And she's like, Oh, my battery went dead. And so my husband went and got his truck, he was gonna jump start her. And he ended I stayed home, and he ended up telling her, why, why? You know that our daughter had just got diagnosed, and their babysitter happened to be 19 and had had diabetes, and my husband said, Oh, do you think she would come over and talk to our daughter? And so the next day, the girl came over, and she's the one who told us. About your podcast. Oh, no kidding. So yeah, so we knew about your podcast within a couple days of being out of the hospital. That's crazy. So I started, you know, just binging, you know, your Pro Tip series, and just trying to listen to all of that. And that worked. And yeah, our first, it worked. Our first. I mean, we knew nothing about pre bolusing. And to listen to that, you know, we weren't told about pre bolusing. I wasn't told about, you know, not to let it get try not to let it get over too high. You know, the hospital was like 200 something in the two hundreds, keep it below that. And so after listening to your podcast, our first three month blood work draw her a 1c we had her a 1c to 5.1 Okay, wow, good for you, yeah. And so she's, she's had three a 1c blood draws since she's been diagnosed, and they've been 5.1 was the first one. 4.9 was the second one, and we're at 5.3 now,
Unknown Speaker 30:56
how are you doing that? So
Becky 30:57
listening to what you I mean, we're being bold with insulin.
Scott Benner 31:03
Can I get a Christmas card or something? I mean, I'm not giving you my address, but, like, you know what, I mean, scan it and put it online or something, that'd be nice. So listen, it's crazy, because I expect that, and yet, when you say it, I'm like, Oh, my God, it really worked. Yeah.
Becky 31:17
And we, you know, we were MDI at first, which, you know, was a nightmare because of her. You know, by the time she got home in the hospital, she was very angry. There were, there was, at one point we had to sit on her to give her a shot because she did not. She was like, I'd rather die. I don't want to do this. I just rather die. She really say that. She said that. She said I'd rather die than give myself than have to have shots. And we were like, well, Kara, you know, there's a pump. There's, you know, and she would not even think about the pump that point. She was too scared. She would not even think about it. So we were MDI for the first three months we were we finally were able to get her to get, get the Dexcom on after about a month, maybe, maybe three weeks, my husband had to put one on and wear it first to show her like it's not that bad. And finally, we were able to get her get that on her once we got that honor. Obviously that helped, because we could see where her numbers were without having to prick her finger all the time, because she would fight us on pricking her finger. So yeah, we could we just listen to your podcast and listen to the Pro Tip series, and I don't know I learned so I learned so much now she won't listen to him. I'm always like, here, Kara, will you here? Listen to this one. Sounds really good. This will tell you No, she won't listen to him, but I do, and so I'm trying to teach her, what
Scott Benner 32:36
else is she resistant about? And is it something that you're able to get past or does it pretty much stick,
Becky 32:42
really? She's resistant to too many other things. She just is just like I said, very black and white. So reasoning skills are very, you know, her reasoning skills are difficult because she, she doesn't like to reason. You know, if you, if you say the sky is blue and she thinks it's green, she's gonna say it's green. You know, she's just very black and white. She does pretty well with most things. It was really the needle thing. That's, I mean, when she was younger, there were more things she didn't like certain smells, she didn't like certain sounds, she didn't like, but she's kind of outgrown all of that and moved past all that. It just was the needle thing. Was a big, big, big, big. That was the biggest hurdle we needed to overcome as she's gotten older, because she wouldn't get any blood work done. She wouldn't get she didn't want to get vaccines. She didn't want to, you know, all of that was hard. That's working, okay? I mean, she's now. I mean, it's like I said, come such a long way. I mean, now she puts her own pot on, she puts her own Dexcom on. She will prick her finger if she needs to. Amazed, amazed at how far she's come from us, holding her down, you know, but I think she just had to realize that it wasn't going away. This is part of your life now. It's not going away, and there's nothing else. This is it, you know, there's no other options.
Scott Benner 34:06
I hear you. So can you talk about it from your perspective for a minute? Because when you said you went outside, I imagine you guys going outside and just like, banging your head against a tree for a couple of minutes. What is it like? Like, you know, what's the last 20 some years been like, yeah,
Becky 34:20
like, you know, we have three daughters. She's our youngest of three. And so I knew something was a little bit different when she was probably about three years old. My son's off, and I just used to think she had OCD because, like, if I, if I were to get her dressed, she would shut you she wouldn't let me get her dressed until the drawers were shut or, you know, just really little weird OCD type thing. So when we found out she had autism, you know, it didn't surprise me, like I knew something was a little bit off for me, because I was the one who dealt with all the school and I dealt with all the doctors and the hole in her down every time we had to do something, and I felt like, Oh my god. Why? Why is this diagnosis of diabetes happening to her? Like she's been through enough, and I don't think I can take anymore, right? Because all of her life, I've had to be an advocate for her, you know, advocate with the school, advocate for with the doctors, advocate with everything. So when this diagnosis came along, I just thought, Oh, my God, you know, like, what more? One, can this poor kid be dealt and two, I don't know how much more you know, because I knew the majority of it was going to fall on me. I mean, I'm I'm home now, I don't work anymore, and my husband, you know, works. And so I knew that I was going to be the one doing most of the research. Are you
Scott Benner 35:39
an older parent? How old are you? Yeah,
Becky 35:41
I'll be 53 next week. Okay, so not really an older parent. My first child is 28 so I started at 24 so we have a 28 year old, a 24 year old, and then she just turned 21 in April, you know, not, not an older parent, per se. But for her, she was, you know, something,
Scott Benner 35:59
3031, something, when you had her, yeah, okay, yeah.
Becky 36:02
Her whole wife growing up, I've just had to be an advocate for her, and I've had to deal with her, you know, little eccentricities, here and there, etc, yeah. I just when this diagnosis came, I was just thinking, Oh my gosh. Like, well, we were finally at a point where we, my husband and I could leave, we could go away for the weekend. We could do, you know, and she could be here home by herself, because our other two daughters are, they don't live at home anymore, and so we could go and leave her. And then when this came along, I thought to myself, Oh my gosh, you know, I'm
Scott Benner 36:33
never getting out of this house. We're
Becky 36:34
never getting, yeah, we're never gonna do anything because, you know. But again, it's been a year. She does great. She handles everything by herself during the day and just occasional prompting here and there, but it's the night time that we we have issues with. I think she shuts down at night. I think she deals with it all day long, and then when she goes to bed at night, I think she just kind of shuts down. She doesn't wake up to the alarm. She doesn't want to deal with it, right? And so we have a garage apartment. So she lives in the garage apartment, okay? And we specifically built that knowing that she would probably live with us for a while, but we wanted her to have her own, you know, kind of her own space, and feel a little bit independent before she actually ever does get out on her own, and so, you know, she doesn't wake up. One of us has to truck up outside, up the stage, you know, wake her up, or just grab the PDM and give her, you know, insulin, or wake her up, tell her to drink a juice or whatever, because she's 21 and she's on the spectrum, and mainly because of her age, she you know, we tell her don't eat till late at night, or don't eat something so fattening, because it's going to hit you in the middle of the night, you know. But she's 21 she wants to eat Chick fil A, she wants to eat Chipotle, you know. And that's where we're having most of our issues. Is the night time. This
Scott Benner 37:56
reminds me of that line in the first Jurassic Park film, when the guy running the park asks, uh, Sam Jackson, how it's going, and he says, we have all the problems of a theme park and a zoo. I don't know what that exact line is, but, uh, that's how I feel, like that's the situation you're in. You're like, we have, like, a set of problems from this perspective, and we have a set of problems from this perspective, and her bedroom isn't down the hall or upstairs, it's outside and then in another structure. Oh, and we can't go out. And how you and your husband, okay? Are you? Like, like, POWs, like, just like, keep your head down.
Becky 38:35
You know, we, we did really good for a while. We went through a little rough, a rough patch through through this year, I won't lie, and we're fine now. But, you know, it was, it was a lot. It was a lot thrown on us. And I felt like, you know, for a while I felt like I was the only one. He's always been very involved with our kids. He's always been a good dad. Like, I think, because he knows I'm home, I have more time to listen to the podcast and to, you know, research and do stuff. So, um, oh, wow, I felt like, oh, maybe I'm the only one that cares about whether or not she's high or low. But no, he's, he's really stepped up to the plate, and he he does as much as I do, I would say, with the getting up, even though he has to work, you know, we'll take turns. If one night, if she goes high, I'll get up or goes low, I'll get up the next night. He'll do it. So we work pretty good as a team.
Scott Benner 39:24
What conversations do you have with her that are productive? Like, have you found a way to talk to her about stuff that ends well, I just think
Becky 39:32
a lot of it is just, you know, constant reminder, you know, like, when I when she's high, and we'll say, Kara, you know, the reason why we're on you about getting your blood sugar down is this is going to affect you later in life. You know, this can affect your heart. It can affect your eyes. And she already has eye, you know, some eye problems. So I'm like, this could affect your eyes. Could affect your kidneys, you know, just trying to get her to realize the whys, because she, I think, does better when she knows the whys. Mm. Hmm, but it really is just repetitive, I think, with her, yeah, reminding her why, you know, why you have to do this. Do you ever
Scott Benner 40:09
get something to the point where you think, oh my, this is done. She gets it, and then you wake up a year, a month later, and it's back to the way it was? Or once she gets it, does she have?
Becky 40:20
I feel like, once she gets it, she's pretty good about it, like she, yeah, I feel like, once she gets it, she's got it. And, like I said, with the with the daytime, now she's pretty much got it, you know, she, she handles it during the day. I don't really have to, you know, say too much to her during the day. And if I do, usually she's already on top of it. It's just It hasn't kicked in yet, or insulin hasn't kicked in, or whatever. But for some reason, at night, she hasn't gotten How does she
Scott Benner 40:50
handle being low?
Becky 40:52
She handles it pretty good. I mean, she gets she gets shaky, her hands start shaking, and she doesn't really get too stressed out. In the beginning, I used to stress her out, because if she got to a certain number, I was freaking out, you know, I was like, Oh my God, you know, Here, drink this, do this, because I was so afraid she was going to have like, a seizure or something. Then I was overcorrecting, and then she would shoot high. And I was like, oh god. So I think, in the beginning, I think I stressed her out more than she needed to be stressed, yeah, but now, you know, we're pretty good. If she gets, you know, she gets below 70 or below 55 really is when we really start to get more, you know, worried about it. If she's like, at 70 or whatever, like, I drink a juice, she drinks a juice, it still might go low a little bit, but we know that juice is going to kick in and she'll be fine.
Scott Benner 41:41
Has she ever had a situation where she couldn't respond in that low No,
Becky 41:45
no, not yet. We've gotten down to about 43 is about the lowest we've gotten. Okay? We haven't, you know, we haven't had any issues. Knock on wood. So far.
Scott Benner 41:56
What happens to her when she's lower like, like, as far as personality or ability to break reason. What do you see happen?
Becky 42:04
I feel like it's more when she's high that she doesn't have she gets really a she gets mean, almost like, mean, you know, when she's high, I don't when she's low. I just noticed she gets fatigued a little bit easier. She kind of like gets where she wants to nap more after a low, she's She doesn't seem to get too, you know, strange or anything. But with a high, she gets real like, mean, almost like, and when you tell her, like, Hey, you're high, oh, I don't care, you know, whatever, she just, she gets just real ornery. Yeah, when she's high,
Scott Benner 42:35
I think that's pretty common. I was just, yeah, it's interesting. Does she work? I'm sorry, did you say she
Becky 42:41
does work? She does work after, after the the diagnosis, they took her out of the warehouse and they put her in a on a desk job, so she's she does data entry right now, you know, being out in the heat and all that, we just didn't want her after she first got diagnosed. We were like, Yeah, we don't want her in that environment, just because we didn't know at that point how to handle anything, you know, we we were still trying to figure everything out. And, um, so she just, she just fine. Just fine. Working.
Scott Benner 43:11
What about wearing devices? So does she have any, like, tactile issues with those things
Becky 43:17
in the beginning, like I said, she would not. I mean, it was, it was the nightmare, trying to get her to try the g7 trying to get it on her. It's just a for her, she is. So we have to use, like, in the beginning, we had to use numbing cream for everything we did. Like, if she, if we, you know, had to not pricking her finger. We finally got to a point where we could prick her finger without doing anything. But we had to get, you know, when we got onto the devices. We had to do numbing cream for everything, and then, so then you it would take, you know, an hour to do a change, because we would put the numbing cream on, and we'd have to wait 30 minutes for the numbing cream to even take effect. And that was all really, I think, just a mental thing for her. I think she thought if she had the NAMI cream, it would just not hurt as much. So in the beginning it was just a mental thing. Now she does it all without numbing cream, like we've graduated, you know, but, yeah, in the beginning it was like it was this, itches this, you know, our she still says it itches. So we'll use, like, the nasal spray that people say to use. We'll put that underneath her pod before we put it on, and that seems to work for her. And again, I don't know if it's just a mental thing for her, thinking that she has the nasal spray, it works and it doesn't, you know, doesn't itch, or if it's just kind of like the numbing cream was that made her feel better to know she had it on, yeah,
Scott Benner 44:35
who cares? As long as she's happy, who cares? Yeah,
Becky 44:37
that's what said. Who Cares she's and like I said, She's pod changing on herself. Now she puts the Dexcom on by herself. Now, you know, if she, if she's putting it somewhere, she could do it. She still can't put it on her arm by herself for whatever reason, but she'll put it on her leg or whatever else. So, yeah, like, I mean, I guess my point is, you know, we, we went from not knowing anything to finding your. Podcast now feeling like we're, we're still learning. We still, I mean, we did, we did we do see Jenny, which we found through you guys, oh, cool, or through you. So we've been working with Jenny for the past three months, just to kind of learn some of the things that we we just couldn't seem to get control of, like the fat, protein rises, and, you know, things like that. She's been a big help for any other moms out there that have kids that are on the spectrum. You know, the spectrum such a wide, you know, there's such a wide variety of of where kid falls on the spectrum. You know, we're blessed enough that she's high functioning. Now, I just feel for any other moms that are going through this, because if they have a child that's not as high functioning, I can't even imagine how they're dealing with it. What
Scott Benner 45:49
happens, you know? Yeah, yeah. I mean, have you even been able to wrap your head around like I asked you before? Do you think she'll be okay on her own one day? But do you think she'll be okay on her own one day with Aya babies?
Becky 45:59
Um, it's definitely thrown a brunch into the, you know, where I thought we were going to be. I do think she'll be able to be on her own someday and be able to control the diabetes. I mean, the first step is handling it during the day, and she's got that down, you know, she's, she's pretty good at that, if we can just get her through the night to realize that, you know, and it doesn't happen every night, you know. Luckily enough, we don't have to get up every night with her, but on the nights that we do, you know, if we can just get her to the point of of self care in the night, then I don't think she'll be too far off from living on her own, you know, with the room, maybe with a roommate or something. I mean, I think totally alone. But don't
Scott Benner 46:39
let this scare you. But last night, I got into bed and like, an hour and a half later, Arden's blood sugar was going up, and I'm like, what is happening? And she's home for for school right now. And I looked and I'm like, why? This doesn't make any sense. Like, the I can see the algorithm, like, pumping insulin. I'm like, what's happening? So I look a little deeper, and this pump is, like, been expired for four hours, and it's getting ready to shut off, like, four more hours from now, right? I go in a room and I wake her up. I'm like, Hey, and she goes, what? I'm like, you're at the bed with a pump that's almost dead. And she went, Oh,
Unknown Speaker 47:09
I said, so that's what you have to worry
Scott Benner 47:11
about, right? I mean, so good luck is what I'm saying.
Becky 47:16
I know, I know. I maybe it's wishful thinking on my part, but I do think someday, I do, I do hope someday she will be able to live on her own.
Scott Benner 47:26
Do you guys feel an immense amount of pressure about saving money, like, for after you're gone and stuff like that?
Becky 47:32
Oh yeah, oh yeah. Like, we've already, you know, we've already set up a whole thing of, like, in case she doesn't have insurance, you know, we need to have money set aside to cover all of her diabetes supplies. And, yeah, yeah, that's been a real concern. And, you know, she has two older sisters who, you know, to be honest with you, they don't really care to learn about they're not in the house. They're not around it, you know, so, and they shouldn't have to be the ones to take care of her. Something happens to us, right? I mean, so yeah, we do have, we do have a system set up in our will that sets aside money specifically for diabetes supplies and her future, you know, health, in case she's not working or doesn't have a job with insurance or whatever. But, yeah, that's scary, because, you know, you got to have enough to last something. We just
Scott Benner 48:23
started looking to the idea of setting up a medical trust. And I don't know how much money we'll be able to get into it, but at least maybe it would be something, you know, and that's, I mean, I find that frightening, and an Arden is not, you know, doesn't have autism. So exactly, what about other autoimmune in your family? Is there any I have?
Becky 48:44
Hashimotos dad had thyroid issues, and like, rheumatoid arthritis runs in my family a lot. I don't have it. And as far as I know, Kara doesn't have any other autoimmune so far, thank God, but yeah, and I'm the only one with autoimmune in our family. My other two girls don't have anything, and my husband doesn't have anything, so she's probably got it from me, I guess, interesting. Yeah,
Scott Benner 49:09
do you feel better?
Becky 49:10
I mean, I do feel better. I guess I do feel better a little bit. Hopefully, I didn't just rant
Scott Benner 49:15
No, no. I mean, I mean, no, no, you were fine. Don't worry. Trust me, you're fine. I stopped you before it got away from you. Don't worry about it. I let you go a little bit in the beginning, because I thought your stream of consciousness was the interesting. I just thought that if I didn't, like make you aware of it, that we'd still be in it, like a half an hour later. Yeah, and
Becky 49:33
you're probably right, yeah. I think that was nerves in the beginning, though, and
Scott Benner 49:37
it's unfair, because people are nervous and when they come on at first and stuff like that. I can also see where, if I'm in your situation, this would feel like calling a friend with coffee and being like, can I just tell you what's going on? And you don't realize that a half an hour later, your friend's like, just going, Uh huh, yeah, right,
Unknown Speaker 49:54
yeah. Like,
Scott Benner 49:55
oh God, but not even listening to you anymore, because you're like, you have to get it out. And they know. You need to get it out everything. But I wanted you to be able to get some out. But then I wanted to ask you some specific questions as well. And we're not done yet. I just wanted to make sure that you were okay. Yeah, okay, I'm good. Do you or your husband go to therapy? No. Do you think you should? Maybe
Becky 50:14
I do. I don't know if he needs to. You mean as a couple, or do you think as like individuals? I
Scott Benner 50:19
don't know. Becky this whole thing,
Becky 50:22
we're good couple wise, we're good individually. Maybe I could probably use it, even Kara could probably use it. But no, we haven't gone
Scott Benner 50:29
more so since the diabetes. Or equally, equally, I think equally, because as she gets older, am I right? It seems to me like you're in this weird paradox where you're having a an adult child relationship and an adult, adult relationship at the same time. And then how do you exactly right, right, right? And then, good, yeah,
Becky 50:51
I just gonna say it's, you know, it's she, she, you know, wants to be treated as an adult. She thinks she's an adult because of the number of her age, right? So she wants to be treated like an adult, but, you know, she's just, she's just not there yet. So there's still just so many, you know, so many things I still have to just kind of step in and help with. How
Scott Benner 51:11
will you know when she's there?
Becky 51:13
I don't know. To be honest with you, I don't know. Is there
Scott Benner 51:16
a fear that she'll get there and you won't know how to, like, let go?
Becky 51:21
Yes, yes, because I am kind of an A type personality. Get
Scott Benner 51:26
out of here, seriously.
Becky 51:29
So, yeah, that could be, that could happen, for sure. I mean, because she'll always say, I got it, I got it, you know, if I'm saying something, I got it like, but I, you know, I'm like, you know, little, you know, I'm gonna make sure she's got it, you know, instead of just letting her do
Scott Benner 51:46
it, it seems to me that the worst mistake you could make is pushing to the point where it ruins your communication relationship. Yes, like, we want to do that, yeah, where she just writes you off, and then legally, can go do whatever she wants.
Becky 52:00
That is a fear like I've talked to my husband about before. I'm like, you know, she doesn't, she hasn't quite realized yet that she could just go and say, Oh, after you I'm leaving. You know, I don't have to listen to this, or you can't tell me what to do. You know, she hasn't quite figured that out yet. So I'm lucky enough that she still, you know, still kind of listens, but yeah, there's a real scare that one day she might go, What
Scott Benner 52:26
about like, real adult things, like, like, drugs and alcohol? How do you manage that stuff? Okay,
Becky 52:32
so she's never, you know, drugs has never been an issue that I'm aware of with any of my girls. We went. Her birthday was April 21 and we went to Nashville for a birthday. She loves music. She wanted to go to Nashville. She wanted to drink. And we're like, oh, gosh, you know, how do we handle this now? Because we didn't really even know it was
Scott Benner 52:51
in her mind, alcohol, yeah, what would affect anything? Oh, I see, okay, yeah. Like, we didn't know we wanted
Becky 52:57
her to be able to have a drink. I mean, she's 21 we wanted to be able to be able to have a drink, but we also didn't know how it was going to affect your blood sugar. So I'm looking through your, you know, your podcast, trying to listen to, you know, alcohol related podcasts, so I knew what to look for. Luckily enough, she's not a spritzer kind of drinker, you know, you know, what are those? Seltzer? Seltzer? Yeah, the
Scott Benner 53:19
thing in the can they look horrible. Not
Becky 53:22
much in there. That's really all she drank while we were there. So that was easy enough to handle, like, and she hasn't really wanted to try anything else. So, so far, you know, we've been okay. But I did talk, I did have a talk with her about alcohol and how it, you know, can affect her sugar and how can make you low in the middle of the night. You know, later down the road in the night, if you're sleeping, it can make you sleeping, it can make you, you know, get low, right? So, you know, we've had to talk with her. She, she says, okay, you know, that's, that's all I know, you know. But
Scott Benner 53:51
she has money, right? Yeah, she has money. She drives, she has autonomy, and she's aware alcohol exists. Yes, this is an interesting question. I think, what are the largest gaps of time where you're unaware of her location?
Becky 54:05
Not too much. There's not to me, I usually know where she's at. Most
Scott Benner 54:08
of the time, okay, she doesn't, like, leave work and then show up two hours later and you're like, Hey, where were you? And she goes nowhere. Well, yeah, sometimes,
Becky 54:14
like, she'll leave and I'll be like, Where were you? I went to Target, you know? But I do, I do have a tracking app on my phone so I can look to see where she's at if I really wanted to. But usually she'll tell me, hey after work, I'm going to target or hey after work, I'm going she has a boyfriend. I'm going over to boyfriend tunnels. Oh,
Scott Benner 54:31
whatever. Oh, my God. And even think about that, there's a boy.
Becky 54:34
Yeah, there's a boy. So how'd you let
Scott Benner 54:36
that happen? Becky, geez,
Becky 54:39
I know, right? I have to say, though he's been great with the diabetes, like he has learned all about it, he makes sure when they go somewhere, she's got her bag packed with her low supplies. You know, he follows her on the on the follow app. He's in a little group text with us, and so if she's low, he'll text. Say, Hey, she's good. She just drank a juice or something like, they're both very good about keeping us, you know, does he have autism? Important? I would say there's something I don't know if that's if that's been a diagnosis 100%
Scott Benner 55:14
is it a weird thing to ask? It's not a weird thing to ask, Oh, because I had a hard time asking if you had ADHD. I was like, Oh, I don't want to make her upset.
Becky 55:23
Okay? No, no, no, no, no, probably I would say he probably does. I don't know 100%
Scott Benner 55:28
if he does or not. Do you think there's a moment when you look at him and go, I
Becky 55:31
just know he likes all the weird things that she likes. Just to see,
Scott Benner 55:35
wait, what are some weird things that she likes?
Becky 55:38
She's just really into, you know, like she loves the Comic Con stuff, the dress, you know, anything that she can dress up. You know, she's, she was a Harry Potter freak. She was Disney freak, universal freak. You know, we live near the theme parks, so, you know, she's got passes and he, you know, and she loves music and Taylor Swift, and like things that she just takes him to the extreme. You know, where
Scott Benner 56:00
is there a world where you imagined getting him in a corner one day and looking at him going, so what's going on here? Or do you or do you like? Don't think you will I asked, I
Becky 56:09
did ask him one day if he was on the spectrum, and he told me that he was okay. But then the way he said, it made me I was kind of confused, because he said, Yes, I was on this spectrum when I was younger. But I'm like, you don't just go off of it, you know what I mean, like, you either have it or you don't, interesting. So, and I didn't, I didn't, like, keep prying. Of course,
Scott Benner 56:32
it feels delicate to me, you know, yeah, like, I
Becky 56:35
just kind of assumed he, he probably is high functioning, like she is okay, would be my guess. But they both work, they both drive. They both, you know, did you have
Scott Benner 56:45
to have a sex talk with her? Yes, how was that? Course, I did have a good time with that one.
Becky 56:50
What, you know, what? Because she doesn't, her social cues are off. You know, she doesn't really read social cues very well, and so she's being very black and white. I can have those conversations with her and be very open and very black and white about it. And she's good. Oh, interesting, yeah, much easier than having them with my other teachers. They're like, Ah, my god,
Scott Benner 57:11
shut up, lady, yeah. Like, really,
Becky 57:14
you know, but, like, but hers, I can pretty much talk to her about anything. She's pretty she just kind of, she doesn't have a filter, you know, she has no filter. So you can pretty much talk to her about anything that
Scott Benner 57:25
sounds kind of nice, actually,
Becky 57:27
that part of it, it could definitely have its moments where it's easier, right? The no filter thing, though, can also, yeah,
Scott Benner 57:35
I wonder, Oh my God, you listen now, you're making me want to, like, interview, like somebody like your daughter. And I just want to know what foreplay looks like. Is it like a contract? Is it like real black and white? You know what I mean, be super interesting. I could tell you that part. No, I don't think she was, you know what I mean, like, is it like, Hey, do you think we should have sex at 1030 right? And it might be sure that sounds reasonable. Scheduled in, yeah. I mean, if we're done with television, like, you know what I mean, like, because instead of like, actually, I gotta tell you something that sounds much better to me. Like, all the other stuff that happens and you're like, signaling, and signals get missed, or they get ignored, or vice versa. Like, ah, actually, I think it sounds nicer that way. Yeah, it might be. It might be, I don't want you to think about that though. Make you upset, yeah? So I tried. My husband's
Becky 58:27
like, oh, I don't want to talk about that. He didn't want to think about that with any of his daughters. So,
Scott Benner 58:33
so you have to talk about birth control with her. Yeah, she's
Becky 58:35
on birth control. She's on birth control. Yep. Now she was on birth control before, like, from the time she was like 16, but I'm sorry, but from the time she was like 13, because she had just horrible periods, or real heavy, heavy periods, so she was on birth control for a long time. But yeah, now we did have to, have to talk about, you know, how important it is now that you don't miss one, right?
Scott Benner 58:58
Yeah, a lot of things we can forget, not this. Yeah. Do you think she has PCOS?
Becky 59:04
No, she does not. Okay. No, I used to do ultrasound for a living. That was my job. Yeah, she's been checked out. Gotcha?
Scott Benner 59:13
Yeah, I would imagine, once the heavy periods come, you probably looked Yeah. Okay, all right, so Becky, is there anything we haven't talked about that we should have. I don't think
Becky 59:22
so. I guess I just want to say thank you for your podcast. Because really, I don't think we'd be where we're at without it. I mean, we even did a six week diabetes class with a diabetes diabetes educator right after she got diagnosed, and we came out of there still not knowing anything. And everything was so old school. You know, everything was the just like we didn't have any technology. And I was like, I learned absolutely nothing from this six week class, really. And, yeah, I didn't learn anything, but your podcast has been a lifesaver for us. Yes, I mean I literally, or I say we have learned everything that we need to, even the endocrinologist has been no help. But your podcast has, I mean, thank you for doing it. Because, I mean, we obviously wouldn't be in five, you know, five, a one, Zs for sure on the Plus, you know, not being a year out, I would have known nothing about pre bolusing. I would have known nothing about where good range is. Yeah, we just left. We just left the hospital so uneducated, and even the endocrinology office just uneducated, like we just, we didn't, we didn't know anything.
Scott Benner 1:00:36
Are you near Orlando? I am. I'm speaking in Orlando this year. Oh, are you? Yeah, touch by type one.org. Go there. Look at their programs tab. It's free, okay, yeah, if you want, if you're interested in a day of like, that kind of stuff, if you think maybe that would get her interested in something like sitting and listening to somebody talk if she was interested or not. But
Becky 1:00:56
touched by type one, yeah. I've
Scott Benner 1:00:58
heard you talk about that, yeah. So, so seriously. Like, thank you. It's very it's lovely to hear. And I'm, I'm super happy it worked for you. Like, I really am, like, I'm sure there are people who listen or, like, I listen and nothing happened. So I'm,
Becky 1:01:11
I'm telling you, if you follow, if you thought, you know in your and I think the thing, you know, you're bold with insulin. You know, when you say that, you know people are scared. Like, I still get nervous. Sometimes I'm like, I know she needs more, but I'm afraid to give it to her, right? Like, I don't know why I get nervous about it, but as we go along, the more we're getting more. Like, yeah, she needs more. She needs more. Just give it to her. You know. Why are we afraid to give it to her? You know? Just do it. It works.
Scott Benner 1:01:37
I hear you. It's hard. Listen. It's hard for everybody, not just you, it's me, it's everyone, you know. Like, you start looking, and you're like, wow, there's OmniPod more in, you know? And, yeah, you start going through those variables in your head. Like, well, what if the site's bad, like, Am I really even putting it in? Or, like, what if it's like, Is it food? Is it did I miscount a carb? Like, there's so many things that run through your head, and when there's all those variables, you freeze up because, yeah, it's just what happens. So because,
Becky 1:02:05
if you know, we just give her, you know, and she's a high carb eater, you know, we haven't gotten her to where she you know, every once while, she'll have a chicken Caesar's salad, but she's pretty high carb eater. So her bolus is, she's a 5.5 ratio right now, so she gets a lot of insulin. Wow. And you know, when you've just given her, you know, 12 units of insulin, and you know, she's still going up an hour and a half later, you're like, dang, I gotta give more insulin, you know, or she needs to give herself more. How's
Scott Benner 1:02:34
her variability? How's her what variability? Like highs and lows?
Becky 1:02:38
She always seems to go high after eating, and when I say hi, seems like she always gets up to around 180 and then she'll come back down if we've done it correctly, right? There's a lot of times she's sitting at the 180 mark, 180 you know, 185 and we cannot get her down. And we're like, what did we do wrong? You know? Like, what have we done wrong, and we don't know yet. You know, we're still we're still learning. We're still learning. I would love to keep her one below 150 like never go above 150 would be my idea. But we haven't reached that, reach that mark yet. We're still trying to figure out the whole food thing. But I think a lot of her stuff ends up being the fat and protein prizes that we get later. And
Scott Benner 1:03:22
the last thing I wanted to ask you, I'm so sorry, is that like your g7 and OmniPod five, but you're OmniPod five and manual? Because at the moment, OmniPod five doesn't work with g7 but are you going into automation once it does?
Becky 1:03:33
I mean, I we would like to, but now I'm kind of nervous about it, because we have such tight control with our a 1c right now, the way we're doing things, yeah, like, I'm almost a little nervous about going into automation, because I have heard that it's, it's harder to keep, you know, as tight of control, not as aggressive as you're being, yeah, because we're pretty aggressive. I don't know. I mean, maybe for night time, it might be good, but during the day, maybe she'd stay, man, I don't know, interesting.
Unknown Speaker 1:04:01
Yeah, well, I
Becky 1:04:02
can't wait to cross that bridge when it gets there. I
Scott Benner 1:04:04
bet your whole life is we'll cross that bridge when we get there,
Becky 1:04:06
pretty much, pretty much. But, yeah, I just wanted to, I just wanted to rant a little bit about, you know, not get enough education as an adult. And even though they're adults, they're still kids. In my mind, at 18, you know, 19, they still need a lot of listen guidance. Autism
Scott Benner 1:04:21
or not, 21 not exactly the pinnacle of common sense and rock solid thought. You know what I mean. So it's, it's a tough situation, whether, no matter your situation, yours obviously more so. But listen, my son's 24 and the other day he was like, very like, honestly, looked at me. He goes, dude, in my head, I'm like, 14, just so, you know? And I was like, Oh, I was like, well, if we're being honest, I'm like, 15 of mine, so don't worry about it. I
Becky 1:04:46
know I still feel like I'm in that, you know, like I'm in my 30s when I, you know, I know I'm think of yourself, but I'm like, yeah, yeah, when I think of myself, I'm like, Ah, you know,
Scott Benner 1:04:55
we had this conversation last night, and Arden's like, How old am I? In your mind? And and I said, Oh, you're like, your current age. And she goes, How about Cole? And I said, I think of Cole more like 17 or 18. Is that just because it's a boy? No, not because of how he acts. I don't even know. I think it's because he's so stark he looks so he's like such a man now, like he looks so starkly different, that the bulk of my time with him was when he was younger. So if I just think of him my head, He looks younger in my head. And I'm sure that five or six years from now, after spending more time with him as an adult, when I think of him as an adult, he'll be there like that. But Arden, I don't know like I don't I honestly don't know why it happens like that. I
Becky 1:05:38
know like my daughter, my oldest daughter is 28 and I still, I It's still hard for me to think of her as 28 almost 30, you know, almost 30, right?
Scott Benner 1:05:47
Yeah, by the way, she's three years shy of the last baby you had age. You know what I mean, right? Yeah, right,
Becky 1:05:53
yeah. She's, she's, she wants no children, so I'm not worried about that. With her, she's stuck to that. But, yeah, in my mind, she's still, you know, she's still just my little kid, you
Scott Benner 1:06:05
know, all right, okay, well, Becky,
Unknown Speaker 1:06:07
you appreciate your time.
Scott Benner 1:06:08
I appreciate it.
Becky 1:06:10
Thank you. Thank you for the podcast and for all the info you put out there. It's very much needed.
Scott Benner 1:06:16
Oh, it's a pleasure, and I it's very kind you to thank me, but it's not necessary, but I will absolutely accept it and let it bleed my my whole day will be higher because of this. I have a lot of sit here, boring work to do for the rest of today, and if I get upset, I'm gonna think there's a 21 year old girl out there who has autism and type one diabetes. She's got a great a 1c and you did it, Scott, that's right. And I'm just gonna make myself feel better also, by the way, you guys obviously did all the hard work. I just made the podcast, but, well,
Becky 1:06:44
seriously, that was the hard work. The podcast is the hard work, you know, listen, implementing it is, you know, just what you got to do. I
Scott Benner 1:06:51
think what you did was the hard work. I think probably the reason why I have so much trouble taking the compliment is because it's like, I showed you a map, but you still had to climb up a mountain like it's hard for me to take like credit for that, you know what I mean? Well, you should, you should I understand what you're saying? I'm fantastic. All right, now, all right. Well, you were delightful. I thank you for coming on. Thanks. Have a great day. You too. Hold on one second. You
a huge thanks to touched by type one for sponsoring this episode of The juicebox podcast. Check them out on their website, touched by type one.org, or on Facebook and Instagram. You can use the same continuous glucose monitor that Arden uses. All you have to do is go to dexcom.com/juice, box, and get started today. That's right. The Dexcom g7 is sponsoring this episode of The juicebox podcast. Tickets for the 2025 juice cruise are limited. I'm not just saying that they actually are limited. We have a certain window to sell them in, and then that's it. Juicebox podcast.com, scroll down to the juice cruise banner. Click on it. Find a cabin that works for you and register right now. You are absolutely limited by time on this one. I'm so sorry to say that it sounds pushy, but it's the absolute truth. Juice cruise 2025 I hope to see you there. We're gonna get a tan, talk about diabetes and meet a ton of great people who are living with diabetes, if you or a loved one was just diagnosed with type one diabetes, and you're looking for some fresh perspective. The bold beginning series from the juicebox podcast is a terrific place to start. That series is with myself and Jenny Smith. Jenny is a CD CES, a registered dietitian and a type one for over 35 years, and in the bowl beginnings series, Jenny and I are going to answer the questions that most people have after a type one diabetes diagnosis. The series begins at episode 698, in your podcast player. Or you can go to juicebox podcast.com and click on bold beginnings in the menu. I can't thank you enough for listening. Please make sure you're subscribed or following in your audio app. I'll be back tomorrow with another episode of The juicebox podcast. The episode you just heard was professionally edited by wrong way recording. Wrongwayrecording.com. You.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!