#213 NEW Dexcom G6 Mobile App (Now With Siri)
Jake is back from Dexcom to review the all new G6 mobile app.….
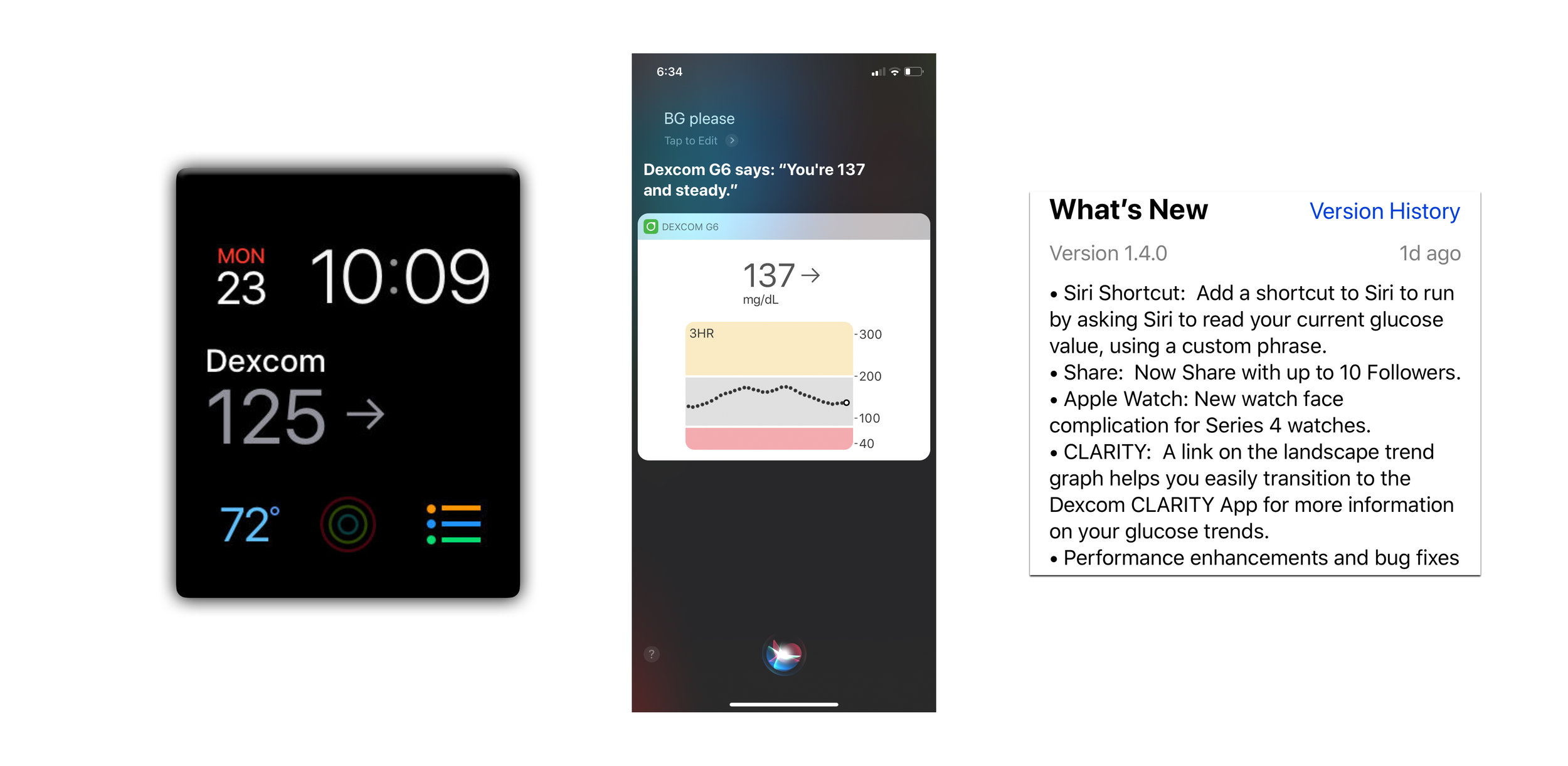
Jake from Dexcom is here to review the all NEW G6 mobile app. That's right, version 1.4.0 is available now and it features Siri, MORE followers and a lot more!
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Alexa - Google Play/Android - iHeart Radio - Radio Public or their favorite podcast app.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
This episode of The Juicebox Podcast is sponsored today by Dexcom and Omni pod, you can go to my Omni pod.com forward slash juice box right now to get a free no obligation demo pod sent directly to your door and go to dexcom.com Ford slash juice box to get started today on the dexcom g six continuous glucose monitor. If you can't remember those links, don't worry, you can find them at Juicebox podcast.com or right there in your podcast player showed us.
Hello and welcome to Episode 213 of the Juicebox Podcast. I did not expect to be bringing you this episode today. But when Dexcom called last night to tell me the new g six mobile app was going to be released in a couple of hours. I thought I need to get Jake leech on from Dexcom. So we can go over the upgrade and see what's there. Not only are we going to be talking about the additions to the G six mobile app, we're going to talk about the timelines for the Dexcom g seven year me right health Canada's approval for G six, and a couple other little tidbits that Jake is thrown in. When you're done here today, you'll understand everything that's coming in the new upgrade. You'll know when your Android app is going to be available. And you're going to be practicing your Hey Siri. Please remember that nothing you hear on the Juicebox Podcast should be considered advice medical or otherwise in the Always consult a physician before becoming bold with insulin or making any changes
Unknown Speaker 1:36
to your health care plan. Scott, Jake, how are you sir? I'm great. How are you?
Scott Benner 1:47
I'm excited about the new GCC mobile. That's how you know you're short on time. So I'll jump right in RNN. I downloaded the update last night which is 1.4 point. Oh, is that right?
Jake Leach 2:00
That's right, one, version 1.4 point zero.
Scott Benner 2:04
And that's the G six mobile app have any other apps? Were any other apps updated last night or are going to be soon?
Jake Leach 2:12
Yeah, the so that was the G six app for iOS. And that was updated when live in the store yesterday, February 27. And we have the updates through the G six Android app that we'll also be getting the Play Store very soon. It's targeted to be right around the same time as the iOS, the iOS when first Android will be very soon.
Scott Benner 2:39
So so even today being February 28. I think just days from now, you shouldn't get should be up in the Google Play Store.
Jake Leach 2:46
Yeah, it probably won't be up. You know, today, but it will be in the real near distant future. We're just we're just basically doing a couple final tests on it. But it has the same features, General features as the 1.4. It obviously, Android doesn't have the unique Siri feature that comes with iOS. But it does have the some of the other features, as well as a new feature where we're sharing data with Google Fit on the Android platform, so that other apps similar to the way health kit works on iOS. On the Android version, we'll have the fit database. If the user selects, they compare their retrospective CGM readings with another app on the phone. So encouraging developers to develop apps that consume the dexcom CGM data and give users a even better experience.
Scott Benner 3:42
I always love that thinking. And there's a I'm seeing in the notes here a three hour delay for the information to go from the Dexcom into the Google Fit. That's pretty standard, though. Does the Health app have the same delay? On the apple side?
Jake Leach 3:52
Exactly. Right. Yeah, it's it's retrospective information. So it's three hours delayed. That was the kind of agreement we got to the FDA A number of years ago on the two different classifications. The idea is that the rest of retrospective data can be used for a therapy decision making in real time like, such as how much insulin to take. So it has a lower level of regulatory oversight. And so the FDA was kind of comfortable with us putting that data in healthcare where basically any app that the user selects, they have to authorize it, but they can authorize any assets able to consume that data to consume it and do offer a, you know, a unique experience around.
Scott Benner 4:32
So we're hoping developers jump in and try to take advantage of that.
Jake Leach 4:37
Yeah, yeah, we've had health kits been enabled on my iPhone for quite a while through the G six, and even the G five apps. And on the Android platform, we have S Health, which is a developed by Samsung, but is available on all Android devices. We've been using that database and now we're adding the Google Fit database as another option.
Scott Benner 5:00
Okay. All right, so I'm seeing a handful of new features in the app, I'm going to start with what I'm going to consider to be the slightly less exciting ones first. But I do want to address so you can submit a technical support inquiry through the through the mobile app. I mean, what, what's an example of something I might want to submit through that.
Jake Leach 5:22
So the technical support, send technical support feature has been in the app for a while, the unique thing about the new feature is that it puts you into a browser, which allows you to select the, you know, the issue that that you're experiencing. So for example, if you're having signal loss issue with the connectivity, you know, some some users do run into that. And our technical support has quite a few things that they can work with the user to resolve that issue. And so that would be a nice example, you can select that and then send it in tech support. And so it's easier for the user to describe in terms that our tech support will understand quickly. That's kind of basically it's about facilitating the the technical support conversation with this sense of technical support.
Scott Benner 6:15
How does the back and forth happen, then do I receive an email back for you? Does that happen within the app,
Jake Leach 6:21
but it can it's generally a phone call will result after you send it in. Sometimes we do over email as well. But the real idea is, Hey, I'm having an issue, I need some help. And to help facilitate that, make it easier.
Scott Benner 6:37
Great. Okay. And then you don't have to go to a Facebook page and wait for someone like me to come in and explain it the 9000 time I've said it, and it starts coming out my typing where I'm dropping words. And I just, I want I once just said to somebody just cycle the Bluetooth, then that launched me into a problem where I had to explain what I meant by cycling the Bluetooth, which then made me think, Jake, why did I do this? I should actually just minding my own business. Okay, so now within the app, there's a button to launch clarity. So there's still two separate apps, though, correct. But I can like I can be in my mobile app. And then is it only on the 24 hour view? that that that link is there or is it somewhere else that I'm not seeing it?
Jake Leach 7:24
It's, it's in two places. So you're right in the in the landscape mode, when you turn the phone sideways and shifts, it shows you the more detailed information in the 24 hour view. In the top right corner, there's a little icon that has the clarity link icon to click on that. And it launches you automatically into the clarity app. If clarity is not installed on the user's phone, it'll redirect them to the store either the App Store for iOS or the Play Store for Google and prompt them to download that clarity yet, so it isn't on landscape screen. It's also in the event screen. So when you go to enter events down, down below on the menu in there, there's also the clarity Link button in there.
Scott Benner 8:13
I'm going to just say that I absolutely I adore the clarity app. And there are days and weeks and months where I think that my daughter doesn't even need to go to an endocrinologist anymore because I have that app which is obviously a stretch but it has so much information it really makes me feel like I know what's going on kind of behind the scenes with her blood sugar's you know that that's how when the when the nurse walks in the room and says, Oh, we know what tre one says, I'm always I'm always like, Oh, I know what our average blood sugar is. I figured that out. Is it this? And I guess and it's incredibly accurate for art. And so it's a great app. If you don't have it. Absolutely. Check it out. Now, you'll be able to bounce back and forth between your mobile app and clarity app with a touch of a button, which is excellent. Apple Watch Series four face complications. Did you add to or are there more and I'm not seeing them?
Jake Leach 9:02
So the with the new series four has the more round complication features. Yep. So in a different series for watch faces, they have places for you to add your complication. So we've added the the round one that's compatible with that watch. So that's a that's a unique one. That's only four series for that we had that that level of compatibility, it shows the arrow and the number. And there are a number on on the watch face. Oh, nice, nice feature kind of, we expect to bring more. That was our first one. We're starting with the simple round complication. But we we have others that are now capable on that platform. we're experimenting with a trend graph. complication that's
Scott Benner 9:49
a rectangular kind of complication. Now you can add so we're working on those but in this release, we've introduced the first one which is the round one and this is liveview. It's my blood sugar number. Right, they're not just touching it to open up the Dexcom app.
Jake Leach 10:03
Correct? Yeah, true, it's realized value.
Scott Benner 10:06
Is that for just the where, like for the person with diabetes wearing the transmitter? Or can that be for a follow watch as well?
Jake Leach 10:15
If not yet, we are in the midst of doing a refresh of the follow app. But a few updates to the follow app. But as the right now for this release, it's the features for the user of the CGM, the personal device, okay.
Scott Benner 10:33
I won't hold you to I'm not gonna ask you how long till I get a new follow up. But just coffee if it's in like the next few months, or something like that.
Jake Leach 10:40
It will be. There'll be a steady stream of updates, but there will be one coming soon.
Scott Benner 10:46
2019 the year of the app, I love it. exploration. So now Now I can get a 24 hour sensor exploration reminder. It'll happen automatically. Is it user definable? Can I shut it off? Or is it always on?
Jake Leach 11:03
Great question, Scott. So it's a, this was feedback from our users about the having the 10 day sensor, they wanted a reminder at, you know, 24 hours in advance of when that sensor is going to expire so that they're sure to be ready to switch the sensor out when it does expire. And so it's, it works just like the six hour and three hour warning, but it just happens at 24 hours. And if the user doesn't have to do anything, it's just automatic.
Scott Benner 11:34
Is that going to exist on the follow up when it comes out?
Jake Leach 11:37
Are you able to say because here's what that is a great that features in our in our backlog of items to implement is not going to be in the near future. But that's definitely one of the features that we want to put in there. It's a great use case where a parent wants to know a when does that sensor need to be replaced? And you'll be able to see it from within the follow up not just on the user's app. Yep, that's a great, great idea.
Scott Benner 12:03
I see two things happen with us, first of all, are no get the like the two hour or the six hour reminder that existed prior to this one. And she clears it out so quickly. She doesn't even know what it said. So I was gonna suggest if maybe a cartoon hammer could come out of the phone and just like donker on the head and yell, tell your dad this. That would be really helpful, because then later, I'm like, hey, the CGM says it's expiring and I didn't warn you. And she goes, Oh, is that what that was? And I was like, yeah, that must have been. But yeah, anything, maybe even just somebody could grab her and say, now would be a good time to stop focus for a second and remind someone that you've gotten this alarm. But yeah, all that kind of stuff on the follow would be fantastic. Okay, so you guys have expanded share functionality in regards to how many followers we can have, how many Can I have now used to be five. I just had a very interesting experience. Last weekend, I was somewhere speaking. And outside of the conference room, I spoken, there were vendors and they all had insulin pumps, and glucose monitors and stuff like that. Now, this event had a lot of newly diagnosed or newer diagnosed, people living with type one diabetes, and I watched a number of them hold up these insulin pumps from other companies at the table with all this tubing on it. And you could see on their face, they were like, what am I gonna do this. But when those same people made it over to the Omni pod table, and they just held this tiny little pump in their hand. And that was it, it was all self contained this little pod. When the people behind the table explained to them that you know, you don't have any tubing with it on the pod, you just wear it on your body. And that's it. There's this handheld controller that you know, you tell it how much insulin you want, set a Temp Basal rate, maybe or start a bolus. When they realized that that controller wasn't attached to the pump that they weren't going to have to wear tubing hidden in their clothing. Just this beautiful feeling of comfort came over their face. They were smiling at the other tables grimaces and What is this thing? But at the Omni pod table, everything seemed hopeful and happy. I am not making this up. This is my honest to god evaluation of what I was seeing happening in the room. And those people all left with what you know, a free no obligation demo of the Omni pod. They had them right there. They took them home now, I don't have one to hand you but if you go to Miami pod.com Ford slash juice box, you can have a free no obligation demo pod sent to you right now. If you're considering insulin pump therapy or switching pumps, the best way to understand the comfort and convenience of Omni pod is to try a free no obligation demo today. My Omni pod.com forward slash juice box with links in your show notes or Juicebox podcast.com. How many can I have now? It used to be five?
Jake Leach 14:45
Yeah, so we've expanded it up to 10. This one again was based on customer feedback, where you know you've got pediatric patients in particular who have a pretty heavy you know, family and diabetes support network. Quite a few individuals, often more than just five. And so we've expanded it up to 10 followers. And so it works in the same way as the previous version did where you can invite your followers through your G six app, but just now you're allowed to invite up to 10.
Scott Benner 15:18
Alright, well, that's gonna be great for I know, people who actually, like have to, like, drop their school nurse every weekend, and then re add them. And it's so that's spectacular. I know, they're going to be grateful for that for sure. Okay, now, what I consider to be the big one, I'm jacked up about this, I think it's great. I can now ask Siri what my blood sugar is. And Siri tells me and not only tells me, but it shows up on the lockscreen. So first, tell me like what made you? What made you work on this? Was this something people asked for? Is this something you were considering on your own?
Jake Leach 15:53
A little bit of both. It's something that we, you know, it's basically a hands free feature. And so it makes it if you're in a situation where you really driving a car or something and you don't maybe don't have an Apple Watch, this is easy to glance at. So you, instead of having to pick your phone up, you can just ask Siri, what your glucose is. The key enabling technology, though, was with iOS 12. Apple opened up the Siri shortcut, which allows us to develop as an app developer allows us to make a shortcut within our app that uses the Siri library. And so and so this feature has to be set up, it doesn't come automatic because you have to record yourself saying Siri, what's my glucose, and each person has to do that on their own phone. And then you can set it to be able to operate when the screen is locked. And you don't have to write so you can if you don't want it to Siri to be activated for this feature when the phone is locked. And you can select that. But most people want to be able to with their own voice ask Siri, what their glucose is without unlocking their phone. So great use case for driving or when you just can't pick up that phone, but you got to know. And when Siri, when you do ask for what's my glucose. Siri will repeat the glucose value. And the trend arrow lets you know if it's going up or down. As well as things like urgent low alert, it'll explain going low will be able to go back to be 55 within 20 minutes. So there's quite a bit of information that she'll she'll repeat to you, which is important to have.
Scott Benner 17:30
And I actually we set it up last night. So somebody from Dexcom was nice enough to let me know what you and I be talking today. And so I knew when it was I knew it was coming out in the App Store probably before the general public and we got it very quickly. So you have to once you update the app, you have to go into the settings and turn on the the Hey Siri functionality. And then what Jake's saying is 100%, right, you have to record yourself saying it. But the great thing is is you don't have to say hey Siri, what's my glucose? You can say anything. So if you don't want the people around you to know what's going on. You could quite easily say hey, Siri, wire porcupines purple, and then it'll pop up and tell you what your blood sugar is. You know, so you're right, you can say absolutely anything you want there. If you want to be private about it. Arden set hers up where she just said BG please. And and now when she says hey
Unknown Speaker 18:23
Siri, BG please.
Scott Benner 18:26
76 and steady. pops right up on the lock screen, you get a nice set of three hour view that you get there along with the arrow and the number of the graduate. Yes, it's really it's really well done. Congratulations. Very nice. Do you really not have a dexcom? g six yet? Come on people? What am I gonna do here? You need to go to dexcom.com Ford slash juice box right now we hear Jake talking about the dexcom.
Unknown Speaker 18:55
It's insane.
Scott Benner 18:57
Every week on this show, you hear me talk about the strides we make with my daughter's health because of the data coming back from the dexcom g six continuous glucose monitor. Have you not at least gone to the link and look@dexcom.com forward slash juice box? That's where you're going to go to get started. Get started with what you ask? How about sharing blood sugars? How about asking Siri what your blood sugar is? What about seeing the direction where the speed that your blood sugar is going at? How would you like to know if you're 75 and stable versus 75 and falling? Big difference right? You've probably always wondered how long do I need to put my Pre-Bolus and you know, you can find out by putting insulin in and watching to see when the fall starts. You know how you could figure that out without testing eight zillion times with the Dexcom. I mean, I think this is obvious what I'm saying here you got to go to dexcom.com forward slash juice box you have to click on the links in your show notes or Juicebox podcast.com and get started today. I really can Not stress enough how important this is. Results are ours and yours may differ. But I mean, come on, you're never going to know unless you try. Buy a Dexcom get a Dexcom, you should buy Dexcom dexcom.com forward slash juice.
Unknown Speaker 20:18
But in business.
Scott Benner 20:29
Okay, Jake, I rushed a little bit so I could throw in some extra questions, which I'm assuming you were expecting. You went over follow apps? And the updates of that. Oh my god, you should see my Siri is like everything I've said to you for the last minute and a half at ditch trying to answer so far. You heard her name? Yeah. And just and just started recording the podcast. So follow up updates coming, you know, this year. I wanted to ask you just very quickly, g seven. I always feel weird asking about what's next one, what's new is so new. But is there timeline for G seven?
Jake Leach 21:08
Yeah, yeah, we are working hard to, we intend to do what we call a limited launch where we launch it into a market, you know, that smaller, smaller volumes so that we can make sure everything's working the way we want it to. We've got everything handled, we did that with G six. And we'll be doing that with our D seven product as well. That'll be around the end of 2020. So the end of next year. And then the real broad launch will be in 2021 is our plan. And before everything is on track for that. So b seven is a is a new wearable. And it's all in one. So there's, it's a completely disposable device. So there's no longer a 90 day transmitter to keep track of each sensor is combined along with the electronics, the transmitter, the radio, everything you need for Bluetooth. And it's all in one piece, and deployed very simply on the body with a very simple applicator and has the same functionality that we're expecting, you know that your customers are used to which e6 the back of calibration, the performance to be able to make diabetes treatment decisions, all of those things are part of G seven. And then we also intend to extend the sensor duration which is seven beyond the 10 days of G six. So you're getting great performance in a much smaller wearable, the wearable for B seven is substantially smaller than g six in all dimensions. But in particularly in the hype. It's a very low profile to the body, the still still a lot of work to do on it. We still have our big clinical trials that will be running early next year for the device approval. But yeah, we've got a large, large focus quite a few folks working on that program right now.
Scott Benner 22:59
I have to say, I think this is the first time I've ever heard you guys like give like a reasonably solid date two years out before. So things must be a be going along the way you expect, which is very exciting. So basically about two years from now by around the beginning of 2021. If everything goes right g7 should be in a wide release. said about right jacket that right
Jake Leach 23:20
there. That's their plan. That's so cool.
Scott Benner 23:22
Hey, everyone needs a plan. Hey, oh, Health Canada has g six now. Is that correct? You can get it in Canada.
Jake Leach 23:28
Did that just happen? It's approved? Yep. Yep, it's approved. And I think it just it just happened. And so they're we're working through launch timing and availability of the product. But yeah, help candidates approve it, which is exciting. because our goal is to transition as many folks as we can as fast as possible from G five to G six g six platform.
Scott Benner 23:51
So Canadians should very politely start bugging their healthcare providers know.
Jake Leach 23:55
Exactly.
Scott Benner 23:57
Is there is there I don't know you might not be the right person because I know your your research and development is your forte, but how are you guys handling? product need? You're obviously growing and getting bigger and the company shifting. And there was a time where there was a you know, if you ordered a you know, they were like, well, we don't have enough supplies, but that seems to have gone away. Now. How did you handle that? Did you open up more manufacturing? Or do you do someone else manufacturer for you? Did you just have to ramp them up? Is it a case of having to tell an outside company? Look we need more of these than we planned on or how does that work? And why is it working now and how are you going to keep it moving for the future?
Jake Leach 24:42
It's a great question, Scott. It is a little bit of all those things. So the supply chain are the folks that we procure the materials for G six from there's some actually build what we call sub assemblies, so they put together certain pieces for example, There's one supplier that makes the plastic parts for the applicator and assembles the needles into them. And they we purchased that the custom design effects come designed with manufactured by what we call a contract manufacturer. So it's fire. So they make those parts. And then we bring them in and we make the sensors in house in our index comm facilities either in San Diego or in Mesa, Arizona, are two locations where we manufacture sensors, and we bring the applicators in, and then we basically assemble it and put it into the packaging, all those things. So in the situation we ran into was the demand for GS six was substantially higher than we had forecasted, which is a you know, it's a good problem for a company have, but it's not great for our users. And so we really worked hard to ensure that we could build a more capacity for G six. So really, that's what patients have seen. And the reason it's more available is because we've added more capacity, and we were adding significantly more capacity this year than we had originally planned. Because the demand for G six is so great. So we're gonna keep doing it. It's scaling both our manufacturers, or suppliers as well as their own operations. So yeah, it's a tremendous amount of work. Kind of, I call it below the waterline right now that customers don't see it. But we're doing everything we can to make sure we can build enough supply everybody with sensors. Well,
Scott Benner 26:28
I really appreciate it. I will tell you that. This this, this I'm gonna try to use English this last quarter of Arden's life with diabetes may have been the most challenging in in regards to her insulin needs and volatility of her blood sugar, and do in, in large part to the information we get back from her g six. I'm forecasting her a one C to be 5.8 when she goes in a couple of weeks, so I just I don't I can't even imagine where it would be without this technology. It simply wouldn't be possible. I can't imagine how to do it. Otherwise.
Jake Leach 27:07
That's incredibly that's good. It's great news.
Scott Benner 27:09
Yeah. Now I just I couldn't I couldn't thank everyone enough. I was actually out in Phoenix. So a couple days ago, I wish I would have realized you were so close by I could have I could have wandered over and said thank you partner person to a bunch of people who would be like, I don't know who you are. Please get out of here. Jake, I appreciate coming on. I'm gonna let you go early, which I don't think I've ever done before. And the next time you have something you want to share, please let me know. I love it when you come on.
Jake Leach 27:35
Great. Great. Appreciate the time, Scott. And I look forward to doing it in the near future.
Scott Benner 27:41
Take care. Have a good day. Thanks, guys. I don't want to ruin the surprise. But guess who's already booked Jake, back on the show. Again, things are happening at Dexcom. Anyway, thank you very much to our sponsors, Omni pod and Dexcom. You go to my omnipod.com forward slash juice box to try a free no obligation demo pause today. And of course go to dexcom.com forward slash juice box to get started on the Dexcom g six continuous glucose monitor. And you know what? They weren't even part of this episode. But why not go to real good foods calm and save 20% on your complete order by using the offer code juicebox at checkout. And do not forget to go to dancing for diabetes.com. That's dancing the number four diabetes.com. Appreciate Jay coming on at such short notice to talk about the app upgrade. I hope you liked this little bonus episode at the end of the week. So much easier than reading about what's on the app. Jake, and I'll talk to you while you're driving home. Ease of use, not just the Omnipod and Dexcom but the Juicebox Podcast
Unknown Speaker 28:51
76 and steady.
Scott Benner 28:54
Please don't forget if you're enjoying the Juicebox Podcast, share it with a friend let somebody else know say hey, this is how you get a podcast. Let me show you right here. Let me give you a link. Let me tell you the name of it. Let me walk you through it because not everybody understands how to get podcasts. Also, if you're enjoying the show, please leave a rating and review at iTunes. We just hit 300 ratings. Yay. Absolutely stunning. I cannot somedays believe it. I know a lot of episodes went up this week. So just let me remind you that just a few days ago, the first three episodes of my series with Jenny Smith CDE called diabetes pro tips went live if you haven't heard them go back. The first one's called newly diagnosed or starting over. The second one is called all about MDI. But trust me there's more in there than just MDI. And the third is called diabetes pro tip all about insulin. There's more coming next month and the month after with Jenny. And when we're done, we're gonna have a nice series that walks you through the ideas that we talked about on the podcast. deep dives into diabetes management
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#212 Diabetes Pro Tip: All About Insulin
Scott and Jenny Smith, CDE share insights on type 1 diabetes care.….
I am thrilled to welcome Jenny Smith, CDE back to the show. Jenny will be joining us for an extended series of conversations that focus solely on the management ideas that we discuss on the podcast.
Jennifer holds a Bachelor’s Degree in Human Nutrition and Biology from the University of Wisconsin. She is a Registered (and Licensed) Dietitian, Certified Diabetes Educator, and Certified Trainer on most makes/models of insulin pumps and continuous glucose monitoring systems. You can reach Jenny at jennifer@integrateddiabetes.com.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Alexa - Google Play/Android - iHeart Radio - Radio Public or their favorite podcast app.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:09
Hello, welcome to the Juicebox Podcast. I'm your host, Scott Benner. This episode is the third in a series with CD Jenny Smith. If you haven't heard the first two, go back and find them. The first one is called diabetes pro tip newly diagnosed or starting over. The second is diabetes pro tip all about MDI. And this one, of course, diabetes, pro tip all about insulin. They're designed to be listened to in order. Please remember that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise. And always consult a physician before making any changes to your health care plan for becoming bold with insulin.
What is it about insulin that people need to understand at its core? And I'll start by telling you that it just a very simple story that that I was in my nurse practitioners office one day, you know, I like to say we're at the end. No, but honestly, I never see the end. Oh,
Jennifer Smith, CDE 1:13
right. It's always a nurse practitioner who is? Yeah, yeah. And most often they've got more time anyway. So that's a good gap. When people
Scott Benner 1:22
say who's your I know, I sometimes have to pause. I'm like, Huh, right.
Jennifer Smith, CDE 1:25
I don't really know.
Scott Benner 1:28
So this was a number of years ago back before I think I would quote unquote, say that I started to understand. And I would say that I've understood diabetes on a different plane for about the last five years or so. Okay, but the run up to understanding it was reaching out into the world and picking these little ideas and really wrapping my mind around them. And as much as I tried to understand bolusing, or understand, you know, the, the peaks and the valleys my daughter was seeing and all the problems we were having. It wasn't until the certified diabetes educator and my daughter's practice, answered a really simple question for me. I asked her if you had a magic wand, and you could change the way people do one thing around diabetes, but would it be and without hesitation, she said, I teach them not to be afraid of insulin. She said that would be the core step one. Nothing else matters if you're afraid of the insulin. And I took that to heart. So I guess let's start with why are people afraid of insulin? What do you think it is? I think
Jennifer Smith, CDE 2:40
the main reason is because the initial education includes so much about hypoglycemia. Insulin, I mean, insulin is one of the very, very few medications on the market, that doesn't have a tremendous amount, but really doesn't have any effect on anything else, you know, it's not going to cause your eyeballs to turn green or you know, your toenails to grow extra inches or anything funny, right? It's its side effect, let's call it is hypoglycemia, low blood sugar, if you don't understand how to use insulin, right, so that I mean, it's drilled into you, if you be careful of low blood sugar. This is how to treat low blood sugar. These are symptoms of low blood sugar, I mean, low blood sugar, low blood sugar, low blood sugar is drilled in. And so what are you going to get from that? I mean, if you're told every time you come to the stop sign that some car is gonna come and swipe you. You're not gonna like go into a stop sign either, are you?
Scott Benner 3:45
It's funny, I think of when you say that I thought of driving in my mind right away a little differently. I thought of when you first teach someone to drive, you teach them about the brakes. Right? Right. Right. So it's the it's the first thing you think, right? Like, even if they steer wrong, or anything, they're doing wrong, if they can stop, maybe they won't get hurt too badly. Right. And so it is really the same idea. I guess for doctors, they look at the giant picture that is type one diabetes. And they say what's, what's the thing where these people could run into a wall, they could use their insulin incorrectly cause a scary low a scary low might mean if you're an adult, loss of your own function, inability to stop that fall from continuing. Right, right. And then so let's talk about granularity for a second because I don't think we do this enough about diabetes. Insulin extracts sugar from your blood. Is that right? Yeah, yeah. And unlike my body, which knock on wood has a pancreas, it's working it my body knows when to stop. It gets me to a nice level, and it stops. manmade insulin is going to work until it's not there anymore, and work
Jennifer Smith, CDE 4:54
and work and work and work and it's going to work in an interaction setting with The food that it's meant to work with or the glucose that's in the in the bloodstream for it to work with now, there's too much insulin there, and there's not enough glucose for it to continue to work with. And it's still gotten a whole hour of action. Absolutely low blood sugar.
Scott Benner 5:14
Yeah, it's not going to cause a low blood sugar. Like you said, if there's impact of carbs impact of body function, then that's what the insulin is working against a minute, the carbs are going from your system or the adrenaline you had is gone. This insulin, if it is still there, if you've missed timed, it, is going to continue to work. So that we know what we are scared about. Let's be more more honest about it. I'm gonna test myself and you'll tell me if I'm wrong. Sugar is the energy that our brain works off of. It's the the gas for our brain, right?
Jennifer Smith, CDE 5:51
It is. Yeah.
Scott Benner 5:52
And if there's not enough sugar in our blood, our brain shuts off like a light switch. Is that correct?
Jennifer Smith, CDE 5:59
in an easy way of saying it? Yes. If our brain is not getting the that sugar? Yes, we that's why all of those strange symptoms come about with low blood sugar, your brain is being deprived of the food it needs to function to think the right way. Yes.
Scott Benner 6:19
Let's just throw it on the table, what everyone's really afraid of right. Nobody wants to die when they're sleeping. That's what everybody's concerned about. I don't want to say that that's not an issue, because if it happens to one person, it's an issue. I would say that I do think of it again, like driving like I, I think driving is incredibly dangerous. But I do it every day. If I happen to have an accident one day where I'm killed, I will not be thrilled about that, as I see the telephone pole coming for me, right. But I think that's maybe the cost of doing business for being alive, I have to get around, I have to travel. Right? I think the same thing about diabetes, you need to use the insulin in an effective way to make your life healthy, longer, happier, you know, all that stuff. So you have to learn how to do this. And then the rest of it just like driving, you throw it away, you're like, Okay, I'm going out there, and I'm going to do my best. And the first thing that happens is people get dizzy, confused, they're easily agitated. But then as your blood sugar continues to drop, you lose the ability to what, like what happens as you continue to get lower.
Jennifer Smith, CDE 7:21
And again, this is where symptoms are different for everybody. But truly what can what really continues to happen is the loss of the right way of thinking you it just continues to decline. And if it gets far enough, you could lose consciousness, you know, you could certainly no longer be awake, doesn't mean doesn't mean daft, but it does mean that you could certainly pass out, um, from a low blood sugar. Yeah, you'll
Scott Benner 7:51
hear it adults sometimes say they knew it was coming, they consumed a ton of food, then wake up on the floor, because then the food gets in and it turns things around for them. Wow. So I'm gonna I've said this before, but, you know, for context in this episode. Prior to technology, I mean, honestly, back when we were needles and little tiny like I've said before, like a diabetes bubble gum water, right. I have caused Arden to have two seizures. One right after she was diagnosed, she was only maybe a few months into it. And I had this grand idea that I had figured the whole thing out, which probably meant she was honeymooning. Right, right. And we go to the mall one day to pick up some stuff real quickly. My wife's going on a trip and we need I think another bag or something. Everybody gets hungry while we're running through the mall. And here's this like, mall Chinese food. And I thought this does no big deal, right? I'll just count the carbs and I'll shoot the insulin and she'll eat the food and she ate and it was good. And she was little two years old. She ate a little bit of food. I gave her No, not a lot of insulin for a 20 pound person. Right, bought the bag went home. She fell asleep in the car later in her crib. My wife and I are helping her. I'm getting her packed up for what she's doing. And then I hear what sounds like a wild animal in my house. grunting and snorting and like like that. And I go into the room and there's my daughter. She is having a seizure in her crib. And so I pick her up and I don't know what to do. I mean, I know the doctor told us about glucagon. But for the life of me in that moment, I couldn't. I couldn't hold my hand. Still, I couldn't reconstitute it. It was a disaster. While she's on the floor, and my then seven year old son is dialing 911 for us My wife is rubbing glucose gel in her cheeks. And as I'm fumbling with the glucagon and really messing it up, Arden is blind. If you touch her she overreacts in a way like she thinks she's being shot like right like he or she is grunting and incoherent and then it just ended. Like when the glucose gel was And she came back and the police came into the house and the rescue squad and we went to the hospital and now I look back, we didn't even have to go to the hospital. Like the hospital was nothing. By the time we got there, her blood sugar was back up, and she was fine in this whole thing.
Jennifer Smith, CDE 10:14
But it's scary. I mean, just, you know, you're saying it. Yeah. You know, I mean, and I talk with and work with so many parents with little, little little, you know, and it is, it's, it's scary when it's when it's your child, and it's not even you. You know, the worst thing now can tell the scary story to tell what I think is the funny story.
Scott Benner 10:39
Yeah, so a year and a half later, we're at Disney for the first time. So our first time outside in the heat. On a big day with diabetes like diabetes, the whole day is going great. Again, no CGM still using needles. end of the night we're walking back to the hotel and coming at us is a vendor holding these giant popsicles. Remember looking up and seeing them and thinking we're like 200 yards from the hotel, like make a left turn, what are you doing, you know, but it's hot out and it's late. And my kids see those and they're like, Can we have them? And I thought, sure, I'm gonna do what the doctor told me to do. I counted the carbs, I gave her the insulin. And of course, it turns out I know now, you know, I could have just let her eat that popsicle. It would have been It was a fast acting car but might have hit her spider a little bit and gone away. I didn't eat any of it. But there we are back in the hotel room. Packing again, always packing with seizures in my house. And so we're packing because we're leaving the next day. She's laying in a bed often another room sound asleep, and I hear that noise again. And this time instead of being confused and thrown off, I say to my wife Arden's having a seizure. Now remember, it's been a year and a half since it happened before. And my wife runs and grabs Arden brings her back, she's holding her and I have the glucose gel and this squeezy tube. Now the gel we owned, you had to screw the top off of them pull the foil thing often, I guess CalFresh
Unknown Speaker 12:08
and then you can use as a gel spoil.
Scott Benner 12:12
Cuz you never cut you know, because honestly now in the of course the ensuing 12 years later, we've never Arden's never had a seizure since then, but right, so I unscrew the cap, and I go to squirt out the gel, and I don't pull off the foil cover. And I squeeze it so hard with so much enthusiasm that a pinhole breaks on the opposite side of the thing. And I'm squeezing and I'm like what's going on and then I look up and on the ceiling of the hotel room is a kaleidoscope of gel, I'm shooting all over the ceiling. So I don't even pause I flipped the thing upside down. And now I just scored it from the pinhole into Arden's mouth, we rubbed around, she wakes up, we put you know, get everything straight, put her back to bed, we were traveling with my brother, when it was all over and to say that it might have been a four minute experience, right? When it was all over, I look in the corner and my brother is cowering in the corner, just with a look on his face. Like he can't believe what he just saw. And my wife and I look up and see the gel on the ceiling, we crack up laughing, wipe off the ceiling, clean it up and go back to packing
Jennifer Smith, CDE 13:14
experience is a good example of the fear.
Scott Benner 13:18
That's exactly right. Because no matter how much I explained it to him, and I said, Look, you know, I don't want to call this the cost of doing business. But we've never been in this situation before we're completely blind. We don't know what our blood sugar's doing. I think the point is this. My point is this. I don't think my point is this. I know my point is this. I don't want to have a seizure. But in Geez, two to 15. In 13 years of having type one diabetes, it's happened twice. It was both when she was tiny. It was both when I didn't know what I was doing. And it was well before the technology that exists now.
Jennifer Smith, CDE 13:52
And before experience of walking around. I mean, in this example, walking around a park all day and not really knowing, hey, she could probably get away with having this little bit of extra sugar, she'll climb, she'll come back down, the exercise is going to hit all night long. She doesn't need insulin, you didn't know that
Scott Benner 14:09
no idea. And now I do. And now Arden can go play softball for nine hours on 105 degree day and she doesn't get low at the end of the day. Because now I know what I'm doing. But I fear that exists exists for that reason. And so I don't know how comfortable you are talking about this because I haven't asked you ahead of time, but how real and this then we'll get off the fear and we'll move on to other stuff about insulin, but how real is the concern that I'm going to go to bed one night and not wake up the next
Jennifer Smith, CDE 14:41
day? I would say that the concern? It's a real concern. 100 Absolutely. It is. Is it a concern that it could happen? wildly out of the blue with and I bring this up With the technology we have today, I would say is that piece is, it's not going to be as common. And it's not because we have alarms and things that set now is technology always perfect. No mean, we can get alarms and alerts for blood sugars that are ultra low or look like they've dropped off the map and you do a finger stick, and it's that the sensor was not right, you know, it was a, you know, a kind of a compression low, or you could have a low alert, and you could actually be lower than the low alert already, right. However, the fear of going to bed and not waking up. While I would believe that it's there, for 90% of people with diabetes, the other percent, maybe don't even think about it or know that it's a potential again, education piece there. But I think that there is the knowing about insulin and action going into that time of the night. I think that's a piece that can really help to prevent that from happening.
Scott Benner 16:10
As we move forward, you'll hear me say a number of times that I think that highs cause lows, because highs create situations where you have unbalanced insulin. And and eventually, like we talked about earlier, body function, blood sugar will will be pushed away by the insolence they're leaving more insulin behind. And there are a lot of times that people will say to me, you know, I get low at 2am. Or, you know, it always happens. And I think well, I don't know that you get low at 2am. It's very possible it's something's happening hours before or you're using insulin hours before. And it's and this is what the residual of that. Right. And so when you use insulin more thoughtfully, I guess is the word. Right? Yeah, that's a great word. You don't have as much of it laying around later in your body that has nothing to do except for to make you low. Correct. And I'm hoping that we get to that as we speak, you've addressed fear and insulin, it's a real thing. It exists for most people. There's good reasons why you should be afraid. But how do we stop people from being afraid?
Jennifer Smith, CDE 17:16
But I think the fear too, and just to kind of clarify there, it's okay to be afraid. But it's also really important that you do something to understand and, and be able to get rid of the fear. It will be there it is certainly, but it's important to learn how to not worry so much with the fear. Let
Scott Benner 17:41
it overtake you. I think of it let it overtake you. Like they tell you with fire when you're three years old? Yes. You have to respect fire. But you can't be afraid of it. Right? Yeah, be afraid of it. Exactly. Yeah. And that that's what I do. I it was the first leap that I made that brought me to the place where I am now. And I think that I think that no matter what tools you give people, if they're afraid to use them to kind of, it's never going to work out quite right. And it's always going to become unbalanced, they're always going to end up in a situation where they go see, look, this is diabetes is unpredictable. And and this is always going to happen and then you know, and that that's that so Okay, so all right. So what's the first step to not being afraid? It's got to be understanding how to use the insulin, right? Absolutely. Okay. All right. So we're gonna get
Jennifer Smith, CDE 18:31
100% 100% Yeah,
Scott Benner 18:33
so let's understand a couple of things. First, that the insulin can do the cause issues for people and one, right people say, I started using insulin, and I started gaining weight. Okay, now, very recently, I had an interview with Chris Rutan, where Chris said, That's not as really nearly as much about the insulin is, as it is about calories. And that was his take on it. Like if you eat extra calories, you're going to gain weight. And that a lot of times we have low blood sugars that we treat with food, but we don't think of that food as we think of it as as necessary because it is not because you're alone, right. But what is the act what is the what is the the technical reason why people see weight gain with insulin. Elizabeth forest was diagnosed with Type One Diabetes. At 10 years old. Then a student in Holly recurs dance class, Elizabeth decide to start a nonprofit organization. Now this wasn't something that she had considered previously, but either was being diagnosed with type one. But after her diagnosis, she was driven to not let diabetes negatively impact her life. And she was inspired to start dancing for diabetes. She did this as a way to bring attention to the stories of the 1.2 5 million Americans who are living everyday with type one and to offer support to those who have been diagnosed and on top of all that she's raising funds to find a cure. started as a community fundraiser organized by a middle school student and a small group of trusted advisors has blossomed into a full scale theatrical production involving hundreds of local dancers and community supporters. Dancing for diabetes has been impacting people through dance for almost 20 years. It has grown from a middle school auditorium to filling Orlando's Bob Carr theater, and is well considered one of Orlando's premier charity entertainment events of the year. I spoke last year at one of their events, and had such an amazing time that I'm going back again in 2019. Elizabeth doesn't have a ton of money to do advertising, but she wants to spread the word about dancing for diabetes, which is why you hear during some of our episodes, I just pop in and say the name really quickly. They're trying to build awareness for their organization, while building a better future for people with type one. So you've heard me say before, and I'm going to say it right here. good at dancing for diabetes.com that's dancing the number four diabetes.com check out what they're doing. It'll put a smile on your face, and maybe you'll decide to get involved. Real good foods believes in making delicious foods, high in protein, low in carbs that are made from real ingredients so you can feel the goodness. You'll never find weird sounding words on their ingredients labels, nor will you find processed grains, flours or other fillers. For example, instead of flour. Their Single Serve pizza crust is made from two ingredients. All natural chicken breast and parmesan cheese. Real good foods family sized cauliflower pizza crust is made from cauliflower, egg and cheese, and all of their foods are grain free, gluten free and use natural ingredients. That includes my wife's favorite enchiladas. The poppers that I love so much the chicken crust pizza Arden adores, and the cauliflower pizza that my mom can't get enough for being a listener of the Juicebox Podcast real good foods would like to offer you 20% off of your entire order. All you have to do with Checkout is use the offer code juice box. And as if that wasn't enough, they also have free two day shipping. Let's hold up some of real good foods products against popular competitors. Their Margarita cauliflower pizza has nine grams of carbs and 20 grams of protein. That other pizza that you know about has 37 grams of carbs, and only 12 grams of protein. Real good foods enchiladas has four grams of carbs 20 grams of protein, and that other one that you know about has 18 grams of carbs and nine protein. Now on to the poppers, there must be even somewhere right? Nope, not even close three grams of carbs for real good foods 29 for the competitor, and protein 22 to four, you can use the links in your show notes or Juicebox podcast.com for both dancing for diabetes and real good foods. And don't forget when you get to real good foods calm to use the offer code juicebox at checkout to save 20% Why do some people see weight gain with insulin?
Jennifer Smith, CDE 23:04
The easy answer there is that the insulin is being it's being mismanaged the dosing of it is being mismanaged and mismanaged Why? That takes in depth analysis of what's going on in the person's individual settings. Right? The and I work with a lot of people weight management wise, type one who I you know, I just I've gained weight or I've done this my blood sugar's are no better, but I've gained weight. Now, if the start with if you're running really consistently high blood sugars, you're actually eating out calories. you're peeing out glucose, because that's how your body is trying to get rid of the excess because there's not enough insulin there to bring it into your body and utilize it. So you may be maintaining a weight that you love. Your blood sugars are high that it's that healthy. On the second side, once you do reign in control, and you're now taking insulin to contain blood sugars, you may be gaining weight, because your body is now retaining some of those calories that were being lost before that you didn't realize, right? So that comes down to the point of understanding lifestyle and the management of insulin. And I bring up a really important piece that people don't, people don't realize. Insulin insulins job is a storage hormone. Insulin job is to pack the food into different places in the body. Right? It either packs it and moves it into your muscle cells or at packs it and moves it into fat. Right? It's usable or it's going to be hopefully used later. If there's too much of it, your body has to pack it away and utilize it later. So that's a that's a lifestyle piece. That's something to look at and say okay, where's my activity? level where it is my nutrition intake need to be is my insulin matching that, am I driving my glucose values too low and like you said, am I taking in too much because of low blood sugars that are consistently happening, and then you're adding more insulin to correct the high that follows and then you're dropping and you're adding food and you're correcting and add. So it becomes this vicious cycle of management, if you don't understand how insulin works. And in a body, I think a good point is that in a body without diabetes, insulin plays a very big role in weight management. And people without diabetes aren't injecting it, their pancreas is making it. So if they're themselves not managing lifestyle, they're having to produce a heck of a lot more insulin, to bring food out of their bloodstream for their body to maintain that normal blood sugar, the way that it's meant to do, they will likely gain weight too.
Scott Benner 25:58
So do me a favor and go over that cycle for a second. I take something in through my mouth that has carbohydrates in it, it goes into my stomach, my bag, my body begins to break it down. It basically those carbs are leached out that sugar, which is the you know, sugar is carbs a sugar comes out. And the insulin actually helps it go into my blood, right it or how does it
Jennifer Smith, CDE 26:24
insulin takes insulin, you know, we take it, we inject it or we pump it into our sub q tissue, it gets absorbed and dissipates that into our bloodstream is I guess the easiest way to say how it works. Insulin in the bloodstream then matches with the glucose from the food that we've eaten in whatever form you know, it could be rice, it could be celery, it could be an apple, whatever it is, sugar in the bloodstream, the insulin and combines with the glucose, they latch on together, and insulin is then the key to the door on the cells. With insulin, the doors open, the key unlocks the door on the cell, the glucose is allowed to enter the cell muscle cells then use it for energy. fat cells, pack it away. So
Scott Benner 27:16
that's how it works. And so with so without insulin, we go into DK, right and so and DK is what is it technically, but what what is it that's happening.
Jennifer Smith, CDE 27:29
So technically, with DK a, it's a significant deficit of insulin with high blood sugars. Right now there are cases of aka at more normal blood sugars. dk however, really is it's a deficit of insulin, meaning that your body is has no way to clear the glucose out of the bloodstream and move it into the places it needs to go. Now your body tries to compensate, like I mentioned before, with the weight management piece, if it tries to compensate, you get really, really thirsty with higher blood sugars. You take in more fluids your body up because you're drinking more, and your body is trying to flush a lot of that extra glucose out. And the only way it can if it can't do that forever, though, at a deficit of insulin. And so your body at the point of not having energy from glucose, it starts to break down fats and proteins. So ketones are produced with the breakdown of fat.
Scott Benner 28:31
Is that why? When I think back on Arden's diagnosis prior to it, she was ravenously hungry at the end, because she her body was starving, and it's telling her eat, we're starving, except the food went in. And then there was no insulin to move it into the cells where it was needed.
Jennifer Smith, CDE 28:49
Correct? Correct. I mean, I could have I remember, I mean, I was older than your daughter and I very, I very much remember the two weeks leading up, especially the week leading up to my diagnosis. I very much remember it. I mean, I at the lunch table in school with my friends. I was asking them for their milk. I was so thirsty and so hungry. And so they would they would get two milks, and they would bring one for me. I mean, I was consuming probably six of those little cartons of milk at every lunch and between classes in the hallway. I needed to get to the water fountain. I mean it was it was unbelievable. The unquenchable thirst and hunger.
Scott Benner 29:35
It really is. A threw me off for a second think of it. No, I won't get back on Arden's diagnosis in it. It just it always just makes me think like how do I not see her dying because she was, you know, no insulin in her body and she was withering away. And he looked back at a two
Jennifer Smith, CDE 29:51
year old it is. I think for kids, it's hard to because kids are hungry all the time. I mean, I've got a two year old and a six year old and man, like every hour, they're like I'm home. Hungry rabbits. I am hungry. Can I have that kids are hungry? Yeah. But it's a different it's a very different ravenous
Scott Benner 30:08
in that setting. Oh my god. Yeah. And so let me ask you something when a blood sugar starts to get low with a person who's being managed, but maybe they have there's their insolence on balance and they're getting lower. Arden will say she's hungry prior to a low blood sugar. And I always tell her Hey, if you feel hungry, first thing we should think about is is Are you hungry? Hungry? Or is your blood sugar getting lower about the same function right there?
Jennifer Smith, CDE 30:33
in a in a similar way, just in an opposite, you know, high blood sugars, you're hungry because your body is starving for the energy. Right? And it's not getting it. Low blood sugars. You're hungry because again, as we talked about, initially, your brain is being deprived. Okay? Your brain is saying, hey, you're hungry. There's not enough go grab something. There's not enough food here. I there's, there's too much of this insulin, it's calling. And sometimes even that precipitous drop in blood sugar that can happen. That's why overindulgence is there with low is I mean, you could literally go to the refrigerator and eat the whole roof. I mean, there there are people who have done that, or just the whole box of cereal. And they're like, okay, where's the next box? You know?
Scott Benner 31:24
It's Yeah, and it's commonly referred to as ether kitchen. Right? Yeah. So yeah. And, and, and so but when Arden was younger, and before sensor technology, and I was staring at her trying to figure out ways to understand where her blood sugar was. One of them was if she said she was hungry at what I thought were odd times of day. I thought, ooh, she might be low. And yeah, yeah, because the looking for the bags under their eyes was not working. I'll never forget, she's diagnosed and the nurse practitioner goes, you know, dark circles under the eyes could be signs of low blood sugar. And then she paused and she goes, or high blood sugar. And I was like, Wait, what? Was that gonna help me? And by the way, it never came to fruition. I spent No, I spent the first year for diagnosis, staring at her face looking for a sign of something wrong with their blood sugar, and it doesn't exist.
Jennifer Smith, CDE 32:13
I have never heard that before Scott in that, right. Yeah. Never heard that as a symptom of high.
Scott Benner 32:21
And it makes me think of the insanity of like when the Arden will say to me, like, you know, you'll be in the middle of a CGM changeover. And I'll say, hey, look, it's been an hour since we reset the CGM, or since we put it on whatever, why don't you go ahead and test let's just make sure we are very thing. Sure. And she'll say, I feel fine. And I always go, ironically, how you feel is not the best indication of what your blood sugar. So and so she still won't wrap it, she still doesn't wrap her head around that right away? If she feels Okay, then she thinks I'm okay. You know,
Jennifer Smith, CDE 32:54
well, and there are some children that have not quite even gotten to the point of realizing what the difference of body feeling is. Right. And if they've lived with diabetes long enough, they may not necessarily know what quote unquote, normal should feel like, right? They may not know that your diagnosis at two or three, they're not even realizing outside of like an ear ache that they're like screaming in pain, or they're pointing at their mouth, because they're two hertz or whatever it might be a kid that young are not in tune with
Scott Benner 33:35
other bodies supposed to feel
Jennifer Smith, CDE 33:36
and and associating it with Oh, I'm low Mommy, or I have a high blood sugar. And so then moving on through life, because they've had diabetes, from such an early age, when you do start to make those connections. It's very difficult to translate that then into, you know, older age.
Scott Benner 33:56
So I was it's funny, you brought that up, because this was gonna be my next question for you. So I just was interacting with somebody on Instagram, who, you know, found the podcast is bringing their blood sugar down, and they have a beautiful stable 85 blood sugar where they feel dizzy. Yeah, okay, now, so I'm talking to this woman, and she says, I'm going to ignore it. I know, it's not real. Like, I know, I'm not in trouble. So I'm just gonna power through maybe I'll give myself a little bit of carbs to you know, kind of help it a little bit, but I'm gonna power through it. Because I know my body's going to adjust to this. And I spoke to a different person who said that they got to that that nice, stable, good number and they stopped themselves from eating too much. But it still they had trouble doing it. So my question is, when you've spent such a long time with an elevated blood sugar, you know, thinking 180 was a great day, you know, or your 250 for six of the hours of the day and you finally get this all under control. You keep listening to these podcast episodes, and you get to A place where you're 85 and stable. When that first happens, you feel like you're low? What's the function of that, first of all, and tell people that it's going to get better, please?
Jennifer Smith, CDE 35:11
Yeah, I mean, the function of that is because your body is having to adjust the values that it hasn't seen as the norm, you know, an average of one at an average of 200, an average of 250. While it's high, you're you may feel normal at that, because you don't know what a normal value or a target value feels like. So as you start to notch things down, your body has to readjust to that new normal value, and it does take some time. So hovering, you know, now at even 110. For somebody who is averaging 200, they may feel low, that may very well feel low, it doesn't mean it needs treatment, is it's truly not a low value, but it does feel low. And so it's hard. It's hard to work through that. I
Scott Benner 36:10
don't know. But I can imagine. Yeah,
Jennifer Smith, CDE 36:12
yeah, yeah. So I, you know, I think as far as CGM, especially I think that's, that's good technology now that at least they can also see where things are going. I mean, if they're at 110, feeling low, and they're all where, all right, they're consistently still dropping very much, especially, you know, fingerstick wise, they might be lower than that. If they're on a trend, if they're hovering nice and stable, nice horizontal line at 110.
No need to treat that fight through it.
Scott Benner 36:39
How long does it I realized it'll be different for everybody. But what's the average amount of time before stable in range, blood sugar starts feeling normal,
Jennifer Smith, CDE 36:48
usually, at least a couple weeks. I mean, from starting, you know, the end, depending on timeframe of how long things were higher, it may take a couple of weeks for that to feel normal at those lower in target values. And again, stability there, and lacking this big jump up and down and whatnot, that makes a difference for resetting those symptoms in your body.
Scott Benner 37:16
Okay. I have one last question. And then we're gonna move on to something else. Can
Jennifer Smith, CDE 37:20
I show you my line right now? Yeah, Jerry.
Scott Benner 37:22
But look at you. Okay, I'm looking at at a Jenny six, our Dexcom line that looks like it's been right at 100 it might have dipped to was that Where's your low at 60 or 70? Below that? 7070 it hit 70 for a little while, maybe for about an hour, and then it banged up at 85. This is very, pretty good for you. Are we? Are we gonna? Okay, here we go. Let me compare. So Arden has one compression low in the last 12 hours. That isn't real. But other than that, let's see if you can see that.
Jennifer Smith, CDE 37:59
Very nice. Thank you. She's even averaging lower than me right now.
Scott Benner 38:03
And we as a new it's a new pump too. So I think you've got the best day. Yeah.
Jennifer Smith, CDE 38:09
I know those pod change days are like, it's almost like magic. Well, can be almost like magic.
Scott Benner 38:17
I actually got walked through walk somebody through how to pod change without a high. And we'll talk about that when we talk about pumping. But yeah, so here's my last question about insulin. Let's get I'm gonna go back to something scary for a second. But I think it's, well, I know how impactful it was for me. So back when I had to dispense with my fear of insulin, like we talked about at the beginning. How do you do that? Right? Like how do you make a leap like that for me, and it will probably be different for a lot of people. I started thinking more about long term health, I realized that the doctor was telling me to leave Arden's blood sugar high so that she wouldn't get low. We were trading today's health for tomorrow's right, like we won't die today. But we might not live a long healthy life either. And I thought that can't be okay. But I still couldn't make the leap. And finally, I thought about it in as technical and scientific way as my brain would allow. And what I what I came to, to think about was I actually spilled some sugar out on the table, and I looked at how kind of coarse and granular and sharp it was on its edges. And I thought well at its, you know, at its microscopic, like existence, it's probably still course in sharp like this. And our bodies are built to handle a certain amount of it flowing through our blood. But if you pack that blood with too much, that must be and this was me thinking my way through when people say I he died of a heart attack, you know, because of his diabetes or he went blind because of his diabetes or he couldn't feel his foot anymore. What that really means is that the sugar has basically sandblasted you from the inside, damaging right making damage to the inside of your veins and capillaries, all the places where bloods covered, right? If you have a heart attack, and they say it was because of diabetes, it's because the flesh in your heart got rubbed thin. And it
Jennifer Smith, CDE 40:10
burst. And I mean, and beyond that, beyond that are the other the other pieces of those complications, such as heart disease that come about, and most doctors don't teach this. And I think it you know, it may be a time thing it may be that they don't want to get the in depth piece of it. I think we
Scott Benner 40:35
should I think to bring up on day three of your dying day.
Jennifer Smith, CDE 40:38
Right, exactly. I am blasting yourself. I have a good and I wish that I could show this to everybody. But this is a tube full of a glucose solution. Do you see how slowly those little they're supposed to be particles of sugar are flowing through the bloodstream, yeah, sugar or nutrients, right, I like to refer to them as nutrients. Because this is the other piece to overall Long, long health with diabetes is, as you mentioned, glucose I love your rough part of that example, because it is high glucose levels cause your cause your blood to get sick, almost like molasses in winter, okay, which means that all of the nutrients, your bloodstream are also flowing very slowly to all the places in your body that need to get those wonderful, micro macronutrients. So healing and everything gets slowed. If your glucose levels stay as high as the the roughness of that sugar that you're talking about, or the high glucose values, it is it's very damaging to vessels almost creates like rust on a car, it creates damage on the inside of the vessels, your body tries to heal itself, it's a self healing machine, your body actually makes cholesterol. It's like a band aid. So even if you never eat cholesterol, again, your liver is meant to make cholesterol and cholesterol is like it does a lot of other things. But it is also a patch, the more damage, the more patch, you see how narrow my vessel is now getting the more and more patches, those vessels that narrow, that leads to high blood pressure, high blood pressure damages your kidneys, high blood pressure puts a lot of pressure on the vessels in your eyes. So it's a it's a snowball effect, with consistently maintained high blood sugars now have a 200 blood sugar because you decided to eat the whole, you know, Disney Princess cake or whatever. And then you bring that blood sugar down. That's, that's a different story than this consistent maintenance of high glucose. That's different.
Scott Benner 42:54
Yeah, right. I think that when people when I say that ardens A once has been between five and six to four or five years, I think people imagine a steady 85 blood sugar forever, which is not the case. Right? She spikes up just like everyone else, you know, if you're gonna if you're gonna eat with diabetes, and not have, you know, you know, not not have boiled it down to low carb or no carb or something like that, right? You're gonna miss sometimes I miss on boluses. You know, insulin pump sets aren't as effective on day three as they are in day one. There's reasons why right? Yeah. So it really is. It's not a perfection you're looking for it's a it's a fluidity of fluidity, it's a consistency to how you manage that's what keeps your eight, one clo, right, as you were describing cholesterol coming in and making patches on, you know, arteries or veins. And it it thinning, you know, that's what people would commonly think of as needing a stent in their heart, right? Like, eventually, it has to open up that space again. Right. So for me back to what I started to say, I got past the fear by saying to myself, I can't let my fear of something happening to art and today affect her entire life. Right? I just can't do that. And, and if that means she's gonna have something bad happened to her or my life's gonna be a little more hectic managing insulin, then that's got to be what it's got to be. right because the alternative is I put all this effort and heart and love into my daughter and at the end of my life when I'm 65 7080 years old, and I'm looking back at my 40 year old daughter and she's in incredibly poor health. I'm gonna think like, what was this all for? Like, you know what I mean? Like what I spend my whole life doing so I'd rather get in the game now and do the best I can let the chips fall where they may a little bit. Then just to ignore it. I can't I am not across that bridge when it comes to IT person. I find I find when you think about life like that. People have heard me talk about it on the show before you get a bill. The mail you can't afford it. And you know, you can't before you open up the envelope, just open it anyway. Right? Be an adult and go, I owe the electric company $400. Like, right?
Jennifer Smith, CDE 45:09
No, that's not going to be better tomorrow, it's gonna be the same bill. Absolutely.
Scott Benner 45:13
It's the same idea with your blood sugar. Like, don't ignore it. Don't say to yourself, that's okay. I'll deal with it later, because later is going to be worse. Now Sox laters worse. So, get in the game, do it. Now.
Jennifer Smith, CDE 45:27
I've always thought about myself, personally, I've always thought about all the things that I am able to do be, because I choose to manage because I have chosen to understand how to manage. I mean, I, I've done a lot of awesome things. I've had two kids, I, you know, I want to see those kids grow up, I want to be around with them. And that, that is the biggest thing to look out to future wise. And remember every day
Scott Benner 46:01
it is, and that's why you and I are doing this like series inside of a it's a it's a series of podcast episodes inside of a podcast. Right? Right. It's because somebody is going to hear that and think, yeah, that's nice, buddy. But I don't know how to keep my kids blood sugar at 70 and blah, blah. But I'm telling you, we're going to talk about how to do that in a way where you don't have to, when you hear the idea of keeping your blood sugar stable to lower number, it doesn't make you think, well, that's impossible. We're, we're going to talk about the tools that make it possible. And I'll leave this episode with this thought. Three nights ago, a man in his 40s I saw him on Facebook, and he was basically begging people, he was at the end of his rope. And he had had diabetes for a long time. And it was just not going well. And people are all jumping in giving them giving him their best piece of advice. And I always think the same thing. When I see people on social media. I'm like, wow, that's valuable. But how do you make sense of it, you know, then somebody else say something else. And I go, Well, that's not really that valuable at all in this situation. But I say why it's well meaning. And so then the person's frazzled, to the point where they thought to reach out into the world to strangers, right. And now these strangers are throwing 20 ideas at them. None of them are cohesive, even if they're good. And so I just couldn't take it. And I, I stepped in and I said, if you want to message me, I'll see if I can help you with this. And there were very kind people who all jumped on and said, I would mesh it, Scott if I was you. So we got we got on the phone. And 45 minutes later, we got off the phone. And the next morning, he sent me his steady overnight graph. And to that day, he sent me his 30 day graph, and the next day, and the next day. And my point is, I can't talk to all of you on the phone and Jenny can't speak personally. But I think we can give you enough tools to get you to that spot. So so keep going with the with this series. And I think you're gonna be happy that you did. I hope you're enjoying the series, I want to take a moment to thank the sponsors dancing for diabetes, real good foods. And even though they weren't mentioned in this episode decks comment on the pod. There are links in your show notes, and at Juicebox podcast.com to all of the sponsors. But you can always go to dancing the number four diabetes.com real good foods.com use the offer code juicebox dexcom.com, slash juicebox. Or my omnipod.com slash juice box to find out more. And don't forget that Jenny does this for a living. And you can find out more about her services at integrated diabetes calm. This episode with Jenny Smith is of course part of a series if you missed the first two, there was diabetes pro tip newly diagnosed you're starting over and diabetes pro tip all about MDI. This, of course, was diabetes pro tip all about insulin. Now if you enjoy these episodes and found them useful, please go to iTunes and leave a rating and review. Over the next few weeks, you'll get the same interview style episodes that you've come to enjoy. And then towards the end of the month, three more episodes coming your way. All About bolusing basal rates pumping glucose monitoring the next steps in this bigger picture. And when Jenny and I finished with these 10 episodes, it's our goal for them to be a roadmap sort of a blueprint for how to use insulin and manage day to day with type one. I also imagine that there may be times during conversational episodes where you hear an idea brought up and you may be able to come back to these episodes for you know a refresher on the concept. Thank you very much for listening to the Juicebox Podcast. I'll see you next week.

Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#211 Diabetes Pro Tip: All About MDI
Scott and Jenny Smith, CDE share insights on type 1 diabetes care.….
I am thrilled to welcome Jenny Smith, CDE back to the show. Jenny will be joining us for an extended series of conversations that focus solely on the management ideas that we discuss on the podcast.
Jennifer holds a Bachelor’s Degree in Human Nutrition and Biology from the University of Wisconsin. She is a Registered (and Licensed) Dietitian, Certified Diabetes Educator, and Certified Trainer on most makes/models of insulin pumps and continuous glucose monitoring systems. You can reach Jenny at jennifer@integrateddiabetes.com.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Alexa - Google Play/Android - iHeart Radio - Radio Public or their favorite podcast app.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:06
Welcome to the Juicebox Podcast. I'm your host, Scott Benner. And you're listening to the second installment of my series with CDE Jenny Smith. This episode titled all about MDI is just that it's a conversation about multiple daily injections. Please remember that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise, and to always consult a physician before making changes to your medical plan, becoming bold with insulin.
How frequently does someone leave a diagnosis with an insulin pump?
Jennifer Smith, CDE 0:50
I would say never.
Scott Benner 0:55
Johnny Smith has lived with Type One Diabetes since she was a child. She holds a bachelor's degree in human nutrition and biology from the University of Wisconsin. She's also a registered and licensed dietitian, a certified diabetes educator, and a certified trainer on most makes and models of insulin pumps, continuous glucose monitors, and continuous glucose monitors. And besides that, I just really like the way she talks about type one. Jenny Smith is a CD. But she's also a consultant at integrated diabetes, where she helps people who are struggling to figure out their type one, you can find out more about what she does at integrated diabetes.com.
Jennifer Smith, CDE 1:37
Part of the reason for that not leaving a hospitalization or a doctor's office with a pump is because of all of the red tape that you have to sort of go through for ordering and you know, that kind of stuff. I would say the rare case, this is probably 10% of the time, maybe even less, somebody's pretty quick to get the order written by their prescriber. And in fact, I worked with somebody maybe a month ago that her little boy was diagnosed and how to pump within about six weeks. Okay, but that's pretty quick. It's not typically that fast. And
Scott Benner 2:14
most people are going to get diagnosed with Type One Diabetes and leave with either pens, or syringes or syringes, right, yeah. And so whether you are a person who thinks right away, I have to have a pump and you hammer through insurance and get it six weeks later. Or if you're a person who gets told, we don't give pumps to people until you've had diabetes for six months, or any of those arbitrary times that doctors throughout one year
Jennifer Smith, CDE 2:36
or until you're in perfect control, then you can have a pump.
Scott Benner 2:40
You know how to do this so well that you'll never want a pump, we'd be happy to give you one, which will never come. And so some people are going to need to know what managing with just MDI looks like. So multiple daily injections. These people are going to get some sort of a fast acting insulin that they can use it meal times and to try to adjust highs and they're going to get a slow acting insulin, that's going to be their basal insulin. Right, though, so let's start slow with the basal insulin. There's a lot of them on the market at this point. Back when Arden did MDI we were using 11 mir. And we found that we had to split it half a dose every 12 hours. How? How much of that is really good advice about slow acting basal insulin,
Jennifer Smith, CDE 3:28
specifically, that what you found with 11 year as a specific brand or type is very common.
Scott Benner 3:36
Okay? While while you know, the makers of love of beer will say that it is a 24 hour acting insulin. What we find, especially with the smaller doses, is that dosing twice a day or two injections of it works much more optimally because it doesn't carry a full 24 hours. That was absolutely my finding. I think a lot of people find that. So that's the first thing to understand. If you say to yourself, every day is certain time my blood sugar goes up. And I can't understand why I bet you it's about 18 to 20 hours after you've injected your long slow acting insulin. And so the important thing to remember when you if when you make the decision to split your basal insulin is that it might not be a 5050 split. So right say you have your five units or a one unit, it doesn't matter. It doesn't mean you're going to put in a half a unit and then a half unit again, 12 hours later, it might end up being three quarters of a unit or one and then a half later, there's your because your body has different needs at different times.
Jennifer Smith, CDE 4:40
Right. And that kind of goes into understanding the needs of the different age groups. kids and teens tend to have a much more profound increase insulin need in the overnight like literally like as soon as their head hits the pillow kind of thing and through and into the overnight. So splitting dose for, you know, multiple daily injections with the basal insulin, you may have a heavier dose in the evening than you do with that morning time, the heavy dose in the evening carries you through the increase in need overnight as well as the morning which is a little bit higher resistance as well. And then your dose in the morning kind of carries you through the day when you're more active, right? And you likely will need a lower bazel amount.
Scott Benner 5:26
And so all we've really said here, and I I repeat this a lot to people is that setting up your slow acting baseline so when you're on MDI is about amount and timing, right, yeah. We're gonna say this in the next episode, but so make sure you get to that next episode, but you have to balance the impact of the insulin against the action of carbs or body function, right. So it's just, it's about a tug of war between those things. And that again, I'll talk about a little later.
Jennifer Smith, CDE 6:00
And that's we're watching you know, glucose values, especially if you are privy to getting a CGM early on, which I do encourage over I've said it a million times to people that I work with, if I had to decide on a technology piece
Unknown Speaker 6:14
between CGM and a pump. If somebody was going to take one away, I would 100% keep my CGM, right 100% take my pump, I'll figure out my multiple daily injections. As long as I've got the data and the trend of what's happening. I can figure it out. If you were gonna I would 100% agree with you if you're going to say that one thing's more important than the other, which I think is a bit of a, you know, yeah, you're right. I I'm not looking to give one of them away. Well, they're my way Endymion. When you when you lose your pump, when you're using MDI, what what that means is that if you want that kind of like, tighter control, I guess, you're going to be injecting more. If that doesn't bother you, then right on, you know, like, that's absolutely fine.
Jennifer Smith, CDE 6:56
You also actually what my friend ginger does. Ginger Vieira, who I wrote the book with the pregnancy book, which, you know, she long term has been multiple daily injections. She uses CGM, she is not scared to give 12 1620 micro dosing adjustments through the course of the day to keep things tightly managed.
Scott Benner 7:19
And so and i think so I always say the same thing. Here's what you gain with a pump. You don't have to inject all the time. And you now have the ability to manipulate your basal insulin. Yeah, but other than that, there's no more
Jennifer Smith, CDE 7:31
precisely right, we can manipulate bazel with injected bazel. We don't, we don't recommend it. Like we would on a pump, it's difficult to difficult, it's difficult to manipulate. But you can use your precision to do that on a pump. Yeah,
Scott Benner 7:48
the first time I thought about getting on a pump, and I didn't know anything about them, and I went to a pump class at our children's hospital. You know, even back then I didn't realize that, that my basal insulin would just be fast acting insulin given by the pump, but in smaller doses, like, like spread out over minutes and hours, right. And I didn't, I didn't think about that. It was explained to me in that room. And then I thought I could shut it off. Like because how many times I thought, Oh, I wish this level Mir had an off switch right now. Right? Turn it off, she's stable, and she's at but I know she's gonna go down because this, this level here, she's gonna keep working in the
Jennifer Smith, CDE 8:25
bank. And I don't want to feed her three juice boxes just to prevent it right looking for that.
Scott Benner 8:30
I have become adept at manipulating Arden's blood sugar with basal insulin through her pump, but that's not what we're talking about right now. But we'll get to it in a different
Jennifer Smith, CDE 8:39
kind of leaves in it goes very well with MBI because you can manipulate differently even if you are on MDI.
Scott Benner 8:48
And so so I guess the first thing I would just very basic ideas you're injecting you need to pick multiple sites keep rotating your site you can put in so on and over and over in the same spots it's it's incredibly important because you your your spot, your spots will become saturated, you can actually what do they call that when that when you can actually see like bumps under this under your skin from
Jennifer Smith, CDE 9:11
Yeah, it's it's really a either a scar tissue development or potentially fatty tissue under the skin that that light, light bow hypertrophy. Other big, you know, fancy words for it. But really, it's just when you inject in the same place over and over and over and over again, you're damaging the underlying skin tissue. And it can lead to like I said, either scar tissue or fatty deposits, and unfortunately, then the absorption in those areas, is quite variable, quite variable, if anything at all,
Scott Benner 9:46
and you could lose your favorite place and never be able to use it again and walk away. So when your doctor or your nurse practitioner tries to scare you with whatever gin, whatever Jenny just said, they're like, something like that just thinking of myself. Just think to yourself, Well, that sounds scary. what she meant was rotate your sights,
Jennifer Smith, CDE 10:02
rotate your sights, and there, you know, there's so many places on the body to use. I mean, the backs of the arms, the lower back the upper, but the legs, the tongue, the tummy, the sides of your tummy. I mean, you've got a lot of places to use. So I think with little kids,
Scott Benner 10:19
that's always a it's a question with parents, you know, mainly because little kids, there's, there's so little, I mean, Arden was too, right. So it's, it's like it's finding the place on such a little body. And I'm let me veer off for a second to say something that I think people will find valuable, especially parents. I did some quick math, and in the time between art and being diagnosed, just after her second birthday, and when we got her on an omni pod, when she was about four and a half, I think we ejected or, you know, or stuck her fingers a combination of 10 to 15,000 times those years, right? Or a lot. And every time broke my heart in a way that I find difficult to put into words. and years and years later, we had been on the on the pod for years, before we ever ran into a situation where I thought I should inject here just to see if my site is bad, right? So we had had, we were on a just a really great run with with insulin pump sites. But one day, a number of years after we switched from from MDI. I said to Arden, hey, I'm not sure if this site's bad, and I don't want to change the pump if I don't have to. So um, you know, in Jackson, and so on, if it starts going down right away, I'm gonna say the pumps, sights bad. And if it doesn't, then you're just resistant for some reason, we're gonna give you more insulin. So I put it up on the counter. There she is, you know, she's like, six, seven years old. I pull out the insulin, and she's just going along. And I bring out the syringe and she says, What is that? And I was like, it's a syringe. It's a needle, I'm gonna put the insulin and then she goes in then what? And I said, Well, I was thinking of injected. And she was like, Well, well, well, well, well, wait a minute. Like really? Like, what are you doing? I'm not getting a needle. That's not something I do. And I was like, do you not remember these? No idea. no recollection of ever getting a shot ever. So I know, it breaks your heart as a parent. But I don't want to say kids are resilient, but time has a way of, you know, blurring the past. So yeah,
Jennifer Smith, CDE 12:27
absolutely. Absolutely. And that's, you know, even pump sites then, you know, same thing with rotation. Yeah, yeah, they all need to be rotated. And that becomes a, I think it as an as an omni pod. Plus, there are so many more places that you can put that pod. And easier, especially from the kid standpoint, or anybody who has dexterity issues or whatnot. You know, because there's no tubing, there's no tubing, and you can pop it on. And that's even easier than an injection.
Scott Benner 12:59
I've seen people put them backs of arms. Arden wears hers, you know, the left of the right of her navel on her stomach, and you can even and she wears them on her thighs. You can even rotate within a rotation. So you could put it on your stomach canula facing your belly button and then the next day turn it and you know, put it the other way like you can. If you have four spots, you have 20 you know maybe because you can just kind of start moving around a little bit. I've grown grown women who wear them on their breasts like that one. Like I show that every once in a while somebody will kind of like pull their shirt down online. I said it's the Arden arms like I've never done that though. Yeah,
Jennifer Smith, CDE 13:37
yeah. I've not tried that myself. Although, you know, this year, Chris Freeman.
Scott Benner 13:43
I was gonna bring Chris on.
Jennifer Smith, CDE 13:45
He wears he wears it on his chest. Yeah. And I know he also wears it on like his upper back. And I've seen people on many of the like the Facebook, diabetes groups and whatnot. The places that I mean, people wear them on their calf. I've seen people wearing them on their forearm. Now, although not approved site. Again, this is where your diabetes will vary. And you figure out what works for you. But you know, yeah,
Scott Benner 14:13
for people who don't know Chris is a four time Olympian and a cross country skier. And there is a picture that he shared years ago that is to this date, the most popular thing I've ever put on my website. So ladies, you might want to look at why you're clicking on things, but it's Chris without his shirt on. And he has no body fat to speak no, because we're the reason he wears it where he does and my point is he still pumping and using a dexcom and so if someone tells you you're too skinny for this, or I've heard it both ways, so funny. Oh, you're too your kids too chubby for that pump. Your kids too skinny for that pump. I there have been I've heard a million different excuses. But okay, so MDI, so rotate our sites. What are other good practice? is around MBI.
Jennifer Smith, CDE 15:01
Other really good practices, make sure you are changing the syringe, if you're using a pen, really, really important as syringe itself, as well as the pen needle caps. In fact, one of the very, very common practice for people to do is reuse the pen cap. And by reusing, they actually store the insulin pen with the needle cap, screwed on to the pen. Really not a good idea, it can introduce air into the pen. And it can change the way that the pen dialing and actually dose the insulin. So if you are going to reuse the needle cap, I don't recommend doing it. But if you are going to do it, take the needle cap off in between those uses. Always make sure that you're wiping the top of the needle, or the insulin pen itself, you know, with an alcohol swab, just cleanliness. Those are kind of the basics.
Scott Benner 16:01
Okay, well, what about and I realized to go back for a second, you were starting by saying don't reuse a syringe, which never in my wildest dreams even occurred to me, but you're telling me people do that, too.
Jennifer Smith, CDE 16:10
People do that. Absolutely. And, you know, having worked with people across the spectrum of economic setting, just like insulin is expensive. I mean, even though a box of syringes is not expensive, even off of the shelf, it's not expensive without a prescription. Again, it may be something that people are reusing because it's an expense that they could decrease somewhere, right? You know, so if you
Scott Benner 16:40
could avoid that, please do. So I have a question. And here's a good place to put it. I'm probably gonna bring it up again, we talked about pumping. So the quickest story would be that one day I took off Arden's pump, and I saw a little redness under where the adhesive was. And I was quite literally standing in my house, rubbing my hands together thinking, because I was scared Oh my God, is she allergic to this adhesive, and we can't pump any more like my brain was racing. And I'm rubbing my hands together and rub my hands together. And as I was doing, and I thought, Why are my hands so dry? And then I realized I'm constantly touching alcohol. Yeah. And so I do a little research and I find out that in Europe, it is not common practice to clean anything, a site with alcohol. And I was like, Huh, so I stopped doing that. And Ardennes never had that problem again, and my hands don't crack as much in the wintertime. And so is that a lawsuit? decision? Like do you say to somebody clean this with alcohol first, because every once in a while someone's gonna get an infection or why do we teach it and some other places don't.
Jennifer Smith, CDE 17:53
Alcohol itself is not a I guess the best thing that that I can call in layman's terms, it's a degreaser. It literally wipes clean, that area of any freeze any any skin moisture, any lotions, anything that could be on there. It's not antibacterial, okay, it's wiping the area in Sure, right. But the real reason for cleaning the site is just to make sure that you've you've taken care of anything that could be there and as far as adhesive component, it's very likely of course that the adhesive isn't going to stick as well if you've got body lotion on it or if you haven't taken a bath in two days and you're putting it on your skin and your skin has done its normal thing and you've got oily skin so the adhesive isn't really gonna stick as well. What do I tell people, I also do not use alcohol. Oh my gosh, a CDE that doesn't use alcohol swabs. But I do of course have a clean site. And by clean site I make sure that I wash the area. Soap and water make sure that it's clean dry it and that's what I you know apply on top of then you're entirely 100% right? Alcohol is it will dehydrate the skin and used over and over and over especially for kiddos little kiddos who have very sensitive skin to begin with. You're just asking for more. I mean, there are skin barriers if you do truly have a you know, a site problem. But yeah, even for injections though, making sure that the injection site is just clean. I mean obviously if your kids been outside rolling in the mud or in the sandbox or doing whatever they've been doing in the rain puddle, clean the site,
Unknown Speaker 19:47
jacked into it.
Scott Benner 19:48
Do the same thing. I use warm water, clean towel, a clean towel to dry it, let it air dry, something like that. It goes on, you know, schedule your pod change around your shower, you know Get out of your shower. Sometimes, you know, I see some people like, they call them naked showers where they change all their gear, they take it off before they jump in for free or for a couple minutes, they jump out and they do it, then there's a bunch of different ways to do it. But I think the important thing here is to use your common sense, right like to. And that's all I did that day, I thought I'm drying her skin out, and then throwing this adhesive on top of her. No wonder there's a reaction here. Absolutely. There is a wonderful post on my blog about how to treat real severe adhesive allergies, it is one of the most popular posts over the last five years. And I'll link it in this so that people are great. It was written by a mom who devised a infallible plan. And when you see the pictures of the reaction that her poor kid was having, it was an all over body reaction. And she figured out a way for it not to happen and him to keep using this stuff. So that was really good. I remember the first time Arden was in like a thin pair of like yoga pants as like a four year old, and or a three year old or four year old and I wanted to give her a shot in her leg. But we were out and I just was like, I'm just gonna jab the knee right through the pants. And that's what I was like, okay, maybe all these rules aren't that important. And and you know, and so she was like, Oh, my God, what are you doing? And I said, No, it's fine. I brought it up in you know, now I say I've done that in the past and she was mortified. She's like, why would you? I was like, Listen, we were in the mall, you know, like, like, what do you want me to? Because I and here's something I really believe. And I think this is a great place to bring it up. I don't think you should hide when you give yourself injections. No, I agree. I think that not just not hiding. But why in a public place? Would you go to what is arguably the dirtiest, the bathroom to write up a hole into your body?
Jennifer Smith, CDE 21:56
Absolutely. kind of goes along with nursing for women. Why should you have to go to the bathroom to nurse when it's the same thing. It's the comfort level of other people. It's not your comfort level that you're worried about.
Scott Benner 22:13
The Dexcom g six CGM is now FDA permitted for zero finger sticks. That's right, the continuous glucose monitor that Arden has been using forever, does not require calibration from a blood glucose meter any longer. But do you know what it does do? It allows you to see your blood sugar, speed and direction. Are you rising at two points a minute falling at three points a minute, the dexcom CGM will let you know with customizable alerts. And if you're the caregiver or someone who loves someone with type one diabetes, and you'd like to be able to see their blood sugar when they're not with you, that's possible too. Because Dexcom has a share and follow feature that is available for Apple and Android. My daughter's in school right now. We just gave her insulin for her lunch, and I can see her blood sugar. Her blood sugar started to creep up on us a little bit. So I got an alert and we added some insulin stopping arise. The dexcom g six features an applicator that is virtually painless. My daughter says she can't feel it at all. And it's completely automatic. One button push and the sensor bed has been applied. You snap in the transmitter and you're on your way. You can see your blood sugar's on your Apple watch or other smartwatches on your iPhone on your Android phone. You can share it with anyone in the world anywhere. I can tell you without hesitation that the Dexcom continuous glucose monitor is without a doubt one of the main reasons why we've been able to keep my daughter's a one c between 5.2 and 6.2 for five continuous years. To find out more go to dexcom.com forward slash juice box or the links in your podcast player show notes or at Juicebox podcast.com. It's going to be the best decision that you ever made. In 2008, we made the decision to get my then four year old daughter an insulin pump. It's a decision that I wish we would have made years sooner. After seeing everything that was available. We easily settled on the Omni pod that was back again in 2008. Today Arden is about to turn 15 years old and she has been wearing it on the pod every day since then, every day. And as I mentioned in the other ad, Arden z one z has been between 5.2 and 6.2 for five solid years. How do we do that? Well, we start by seeing an insulin pump is more than just a way to not have to take shots. The Omni pod gives you the ability to do temporary basal rates, that's increases or decreases in your background insulin, extended boluses which will help you spread out your insulin over the life of a meal and so much more. The Omni pod has no tubing at all. The pod is self contained. You wear it on your body You control it with a wireless controller. So there's no tubes running through your clothing, and no pump that you have to jam in your bra or down your pants or wherever people have to put their palms that just doesn't exist with the Omni pod. What does exist is the ability to swim while you're getting your insulin bathed while you're getting your insulin and live life untethered. The Omni pod even features self insertion, just push a button. Now I want you to go to my Omni pod.com forward slash juice box. And when you get there, you'll get a free, no obligation demonstration pod sent directly to your house. Check it out and see what you think for yourself.
Jennifer Smith, CDE 25:46
It's the comfort level of other people. It's not your comfort level that you're worried about. Exactly.
Scott Benner 25:51
And so let me tell you, the briefest story. I'm in a restaurant one day with my kids. Were leaving that day. And there's this little girl seriously a little girl injecting at her table. And I stopped at the table, none of my business. I said, Excuse me. I just want to do it. May I say something and they looked up at me in horror, I realized now and I said, My daughter has type one diabetes too. And I want to say good for you for injecting here at the table. There's no reason for you to hide. You're doing a great job, little girl. Last year, I got to do the math. Last year, seven years later, I had to make a phone call about jury duty. And I said, Look, I would like to skip jury duty because I'm the sole caregiver for my daughter, I help her make her insulin decisions. And if you listen, if you'll let me be on my phone while I'm there, I don't care. But if you don't want me on my phone, I need to ask the skip. Right. And the woman says oh, I completely understand. My daughter has type one diabetes too. And I gave her my name. And she says is your daughter's name Arden and I was freaked out. And I thought Yeah, why? And she goes, I read your blog. And I said great. She goes, actually you're gonna find this strange. You've been a real help to my daughter through her life. And I said why? And she said, because you bumped into us in a restaurant, the week a week she was diagnosed, and you told her she was doing a good job and she shouldn't hide. And she's like, and it's been such a big deal in her life. And I was like, wow, oh, touching. I'm gonna get out of jury duty. Right? And, but, but absolute 100% honest story. Like Don't, don't hide, you know, and because Jenny's right it is for other people. It's not for you, and it quietly you'll you feel shame like it quietly will make you feel shameful about what you're doing and you should not be ashamed of accounting type on
Jennifer Smith, CDE 27:50
that at all. It's just like, you know, I mean, everybody wears it I mean, it kind of goes along with everybody wears their pump differently. And there are a lot of people especially Omnipod wares who wear them you know, only in like, unseen locations. Man I like I wouldn't bipod there get decorated with stickers and I used to like color them with markers and now that now that you know we have the 3d printer kind of thing. We don't but I ordered a Wonder Woman 3d print pack snaps. It snaps over the top. It's awesome. I actually got my six year old pick it out because he was like, wow, all those are cool. You have to get Wonder Woman mommy are wonderful. I was like great. I missed that one.
Scott Benner 28:38
But mommy was ours but okay.
Jennifer Smith, CDE 28:41
In fact, one of my favorite places to wear it is on the back of my arm because honestly because it isn't visible. Yeah, not like the other places on my body aren't good. It's just I like to wear it good spot visibly, you know,
Scott Benner 28:54
I would tell you that Arden has in the past seen other people using insulin pumps on the pod and CGM. And it she's not the kind of person who runs around excited about it, but it has quietly given her a lot of comfort. Yeah,
Jennifer Smith, CDE 29:08
yeah. It's always fun to when you run into I call it diabetes in the wild. Like you run into somebody at the grocery store who's like, you know, boldly got their pump, like hanging off their pants or, you know, clip to their jacket or you know, something like that, because I I always reach out I'm always like, Hey, you know, look, you
Scott Benner 29:26
pumps we've all got pumps, and it kind of starts up a conversation and it's, I don't know it just because diabetes is so like, it's such a silent on scene. For the most part. It's just a nice way to bring it to a visible and make it make it normal because when and here's why that's important. I interviewed a singer A long time ago, a Broadway singer named Kelly. And if you go back and listen to Kelly's episode, which I'll link in the show notes, she hid for a long, long time. And it was not good for her. When she finally decided not to do that it was freeing. So I'm saying don't put yourself in a position to begin with, you know, just be yourself and write and this is who you are. And look, I'm not judging you, if you can't bring yourself to do it in public. I'm not saying. But I'm saying if you can do it, do it, you know, you'll be happy with what happens. So, okay, so what are we not? I haven't, I haven't injected insulin in a really long time. So let me tell you one thing that happens to me all the time, every once in a while when I have to give a needle I'm not good at it. tells me I'm not good at it. And so what, what is, like, what should I be doing? Is there a pinch? Is it quick? Is it slow? Like, what's the right way to stick that needle in there?
Jennifer Smith, CDE 30:49
Do it? Yeah, I mean, you know, obviously, the age old recommendation is to pinch up. To put the needle in, when I was initially diagnosed 30 years ago, we were told to inject at an angle almost at like a 45 degree angle. Quite honestly, now the the recommendation is just like most 90 degree pump sets, just straight up, putting it straight in, no angle is needed. A lot of people have questioned to about the needle length, and all of the research and studies that have been done. Regardless of body type, and body stop body size. Even those really, really micro looking needle lengths, they give you the same, the same ability to put the insulin under the skin in the place that it needs to be, which is the sub q tissue, like the that kind of fatty layer for absorption. So pinching up the skin, putting the syringe or the the needle that's on the the pen straight in 90 degree angle, and then just push the insulin in,
Scott Benner 31:59
that I have to keep the needle in for a second or is that a pen thing?
Jennifer Smith, CDE 32:02
That's for the pen. Really, the recommendation is it does vary. I've heard people being told that they're supposed to count to 20. I've heard people say that they're supposed to count to five. When I was initially educated, we were told to tell people count to 10. So that is what I educate with. And it's interesting because if you have ever given a syringe injection versus a pen injection, you will notice the difference if you pull that pen needle out right after and you don't give that count to 10, some of the influent can leak out. Okay. So that's the reason for that count. And whether it's a basal insulin or your rapid acting insulin or a regular insulin. If it's a pen, you do need to do that count.
Scott Benner 32:49
Okay. All right. Um, let's see what you think of anything that I'm not asking you about because I'm at a disadvantage when talking about MDI.
Jennifer Smith, CDE 32:57
I mean, the only I mean, we kind of, you know, bazel insulin, of course, rapid acting insulin, you know, there are multiple of them on the market. And there also is still some use of regular insulin which we called short acting insulin, it had a longer profile of of working in the body than our rapid acting insulins have, it also didn't work as fast. So again, this is where figuring out what your needs might be. For the most part, the rapid insulins on the market, the three age old ones, you know, human log novolog, a Piedra, technically, they're all supposed to work pretty much the same way I can tell you my personal and have one is that human log and Nova log work pretty much the same for me, a Piedra does not I've tried it, it doesn't work the same for me. Then there's also of course, Vf, which is faster acting insulin aspart, which is just faster acting novolog insolence. It does have a faster onset of action, and has, in my experience, having used it for a bit of time, it seemed to have almost a more clean finish to working. It was done and and that was kind of the end of its actual in my bazel was kind of kicking in and doing what it was supposed to do. But you know, determining what again, works for you insurance wise, many insurance plans have a preferred or a tiered kind of both bazel and rapid acting insulin for you to choose. monetarily, if you can go outside of you know, tier one or tier two, most influence are tier two. If you can go outside of that, they'll usually be a tier three and your copay is just going to be more. But if you prefer one over the other, that might be the course of action you have to do. If you can't, then you're kind of stuck using what the preferred is
Scott Benner 34:52
okay? And I'm gonna ask you one question and then we're gonna switch to another episode and talk about insulin. So the one thing I've found That when I talk about Pre-Bolus with people, and you know Pre-Bolus thing is a pumping word, it just means putting your insulin in before your food, right. So you can, you can pre inject you call it whatever you want. But but some, but a lot of times what you'll hear from especially parents is I don't want to inject them twice at a meal time. And I say, look, I understand that, but but if you can't be sure of how much insulin, how much food the child is going to eat, you still need to get some moving first. So if you're on MDI, and you're seeing crazy spikes at your meals, it's because you're not Pre-Bolus thing, I'm guessing, or a lot of other reasons that you'll hear through the next bunch of episodes. But you're gonna have to make that leap in your head like I'm gonna, if I can't trust he's gonna eat all this or she's gonna eat all this, then I need to put some in now, and summon later,
Unknown Speaker 35:49
right.
Scott Benner 35:52
Please remember that the Juicebox Podcast wouldn't be possible without its sponsors for today's episode on the pod, and Dexcom Dexcom, the makers of the G six continuous glucose monitor, and of course on the pod is the tubeless insulin pump that Arden has been wearing for over a decade. You can go to my Omni pod.com forward slash juice box to get a free no obligation demo of the pump sent right to your house. Or you can go to dexcom.com. forward slash juice box to find out more about art in CGM. Heck, you could do both. The next episode of my series with Jenny Smith is called all about insulin. And it's available now at Juicebox podcast.com. are right there in your podcast app. If you're enjoying the podcast, please leave a rating and review on iTunes and take a moment to share the show with someone who you think it can help. Thank you for listening for being bold with insulin, and for remembering that nothing you hear on the Juicebox Podcast should be considered advice medical or otherwise. And to always consult a physician before making any changes to your health care plan.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!