#387 Somebody Call 911
Handling a type 1 diabetes emergency
Ginger Locke is paramedic and the host of the Medic Mindset podcast. She's here to talk about handling type 1 diabetes emergencies, medical tattoos and much more.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or their favorite podcast app.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:10
Hello, friends, and welcome to Episode 387 of the Juicebox Podcast. Today on the show, we're gonna dig deep into an issue that I see people talking about a lot. It's their concern about what happens if they should have to call 911. And moreover, what happens if emergency services arrives, and they can't figure out that you have diabetes, or they don't know. This is such a concern for people that I wanted to get a very learned response on it. So I have a special guest for you today. My guest today is ginger lock. Now besides being the host of the medic mindset podcast, Ginger is a paramedic, and an associate professor of MS professions at Austin Community College. In other words, Ginger can do it and teach it. And she's had the experience of helping people with type one diabetes over and over again. So we're gonna get your answers for you, you're ready, you're gonna like ginger. Please remember that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise. The Juicebox Podcast is sponsored by touched by type one, visit them at touched by type one.org. We're also sponsored today by dexcom, makers of the G six continuous glucose monitor, you can find out more and get started with dexcom@dexcom.com Ford slash juice box, how would you like a tubeless insulin pump, you can get it the same one in fact that my daughter has been wearing since she was four. It's called the Omni pod. And to get a free, no obligation demo sent directly to your door, all you have to do is go to my Omni pod.com forward slash juice box. After a couple of quick clicks and a little bit of typing on the pod is going to put that pod experience kit in the mail. And then you're going to be able to wear it and see what you think. Both people want to understand this topic. But it's it's two different reasons. The parents want to put something on their kids so that you know, emergency emergency situations they can see they have diabetes. And adults mainly want to know if tattoos are a good way to to signal. And I started thinking about the topic and I just thought why don't we just like why don't we find somebody who has probably had this experience a billion times right? I did my research and you seem to have the most popular well liked podcasts on the subject. So
Ginger Locke 2:49
Oh, thank you for saying that. Oh, of course, um, introduce yourself. Sure. My name is ginger Lok and I have a podcast for especially for paramedic students. That was the original idea and but paramedics that are in the field, listen as well. And it's called medic mindset. And so most of what I dig into is the psychology of paramedics. And a lot of people think when I say psychology of paramedics, I think that means I'm talking about PTSD and anxiety and all that mental health issues. And we do you know, that does come up occasionally but more I'm interested in how they make clinical decisions and their thought process under what's usually a stressful environment. But but but not always how they continue to kind of show up emotionally for their patience even after like long hours of exhaustion or, you know, you flip flop back from like one a really acute patient and then the next call, maybe something very kind of low acuity kind of Monday, and if someone just needs help, you know, standing up right in they live alone or something like that. Yeah.
Scott Benner 3:57
How long does shifts usually run? And are you there throughout the country? My expectation is that there are some who volunteer and do this work. Right. And there are some who are paid, depending on your municipality, is that right?
Ginger Locke 4:09
Yeah, yeah, I think most cities, we are paid kind of paid services, sometimes embedded within the fire department. But sometimes like, for example, I'm in Austin, Texas. It's a third city service. So you have police fire and emfs. And they're three separate kind of independent things. But then for sure, there's small communities that have volunteer based system. Yeah. It doesn't mean they're lower standard or anything like that. It just means that there's people are sometimes there's a longer response time because people are responding from home, right. So.
Scott Benner 4:47
But well, we used to where I where I grew up. So when I was when I was growing up the entire time. My father was always involved in a local volunteer fire department, which I've sometimes come to think of as a way to get away from my mom. I used to drink beer that wasn't our house. But they but they also, you know, I saw him while I was growing up, there were a number of like significant emergencies in our town, from car accidents to people, you know, trapped in buildings and serious fire some there were some pretty big fires as I was growing up, and my dad was the guy who ran out of my house and went to the other place and got changed and got on a truck and went and took care of it. So I tried it a little bit in my late teens from when I was 16 till I was 19, or 20. And I did hundreds of hours of training, just to be a volunteer fireman. Oh, yeah. And then we had, you know, an ambulance service in the town that was partially paid and partially volunteered. And they would even the volunteers would spend their time, you know, in the house waiting for calls. And it was really fascinating. We really dedicated people, oftentimes not making a ton of money doing something really difficult. You know, it was, so what about you? How did you get involved? And how do you practice?
Ginger Locke 6:06
Yes. So I'm a full time faculty now at Austin Community College, I teach future paramedics now. I still get to be around patients, because we do clinical rotations in the ers that are precepted by the faculty. So we go with the students, and we, you know, do patient assessments and start IVs. And rounds is probably the common term that people have heard clinical rounds. But prior to that I was in the field for about five years working as a paramedic, and I still where I teach is in the same kind of area where I work. So just kind of networked within the MS community here and, and thinking about your question about the tattoos, I actually talked to some medics, some friends of mine to make sure you know that my my experience and what I thought was the answer. I didn't want to make sure it wasn't unique. Just to me that it was it was kind of the common thought process about tattoos or markers. Right, you know?
Scott Benner 7:05
Yeah, that's cool. So all right, so we have your INSIGHT Plus some other people's. What's the steps to becoming a producer, isn't it? Our paramedics and EMTs are two different levels of qualification? Is that right?
Ginger Locke 7:17
Correct. So an EMT. Generally, if you think of it in terms of college based programs, and you can become an EMT, in one semester, it's a certification course. Whereas a paramedic is often an associate degreed person much like this, the similar links of training as a Rn, for example, who became an associate degree nurse, so two years to become a medic,
Scott Benner 7:43
I remember listening, I'm older than you, obviously, I'm looking at you and you have here but younger than I am, but I am I'm, we used to have these little squawk boxes in our houses that they gave to us that just kind of like alerted this high pitched alarm to tell you there was a fire, and then you could kind of scratch easily here, the dispatcher, and it must have all been like FM or UHF, or I don't know how it worked back then. Because there was no internet, you know. And you could hear as you were kind of running out the door of your house, you could hear the dispatcher talking. And I always knew if it was an accident, that it was going to be bad because the police on the scene would always want to skip over the medic or over the paramedic and go right to the EMT, they'd ask for the EMTs like to be so there was not I always felt like there were two different rigs that were kind of, you know, stocks are
Ginger Locke 8:38
right, sorry to cut you off. EMT EMT. We classifies basic life support and then a paramedic is advanced life support.
Scott Benner 8:45
I have a backwards. Okay,
Ginger Locke 8:47
yeah, the way you said it was was reversed.
So EMT might, you know, most firefighters are EMTs they come and they can do these basic life support things. But then often a paramedic arrives in an ambulance for the for the transport, and they've got a higher level of medical care IVs cardiac medications EKGs ultrasound, more toys. Yeah. And, and additional schooling, additional education. So they think in a more complex way about you know, what could be wrong with the patient, they do get what's called differential diagnosis, they think about what disease could be causing this problem. Obviously, if it's correct, it's trauma, it's pretty straightforward. But in thinking about diabetes, you know, we've got to differentiate things like diabetic ketoacidosis, from sepsis, and those two can look a lot alike or maybe it's both and, and so a lot of our education is teaching medics how to think about diseases and how to sort them without all of the benefits of things like blood labs in the hospital, we do have glucometer so we do know blood glucose levels, but we don't have things like lactate ions and some of the advanced stuff that's in the hospital.
Scott Benner 9:58
So after I I decided that I was going to ask you, I put it out to the community that listens to the show. And I got a lot of questions here for here. So I apologize, but I'm gonna probably hit you with some rapid questions at some point and see if we can't give people a full idea of what they can expect from the emergency response if they have a problem. So a lot of people just want to know, do you open up the health apps on people's phones to look for the information that they put in there?
Ginger Locke 10:25
Yes, we would if they were unresponsive. I think if someone is obviously talking, we would never do that, you know, they're kind of in full consenting ability to just have a dialogue. But when people are unresponsive or in cardiac arrest,
yes, but
it's not the first thing we do. It often comes into play a little later into the call. So the one mindset of medics is a find it fix it approach, right. So if, if the person is on their back, unresponsive and they're snoring or they're gurgling, right, we just open the airway, we do some suctioning. So it's just we find this we fix it, we're not yet thinking what caused all of this. It's just some if they're bleeding, we stopped the bleeding a lot then minutes into the call when you start thinking, what caused this? And is there anything any additional treatments than Yes, we start, we start looking through you know, looking for insulin in the in the refrigerator looking for papers that look like they might be prescription, you know, papers from the pharmacy or things like that,
Scott Benner 11:36
go through purses and stuff like that look at your possessions.
Ginger Locke 11:40
But on the iPhone, there's this functionality to get into someone's medical ID and I teach that I teach that to paramedic students of how to get in there that different iOS is and talking specifically about the iPhone. Sorry to just be talking about Apple but there for a while there was a functionality where you just tap I don't know what button that is. This is volume. I guess it's one of the menu buttons right on the side. You do it five times. I think it opened up the medical info. That's interesting. Don't do it. I don't know. Sometimes it does.
Scott Benner 12:15
Let me try. Don't try to now pay with my credit card.
Ginger Locke 12:21
Doing an emergency SOS right now
Scott Benner 12:23
versus calling for help. I they just added these tap functions to the back. But that's
Unknown Speaker 12:29
that's bad calling 911 Are you really cheap?
Scott Benner 12:34
At least they'll know it's you. Right? Are you gonna say hey, it's ginger. I'm sorry.
Unknown Speaker 12:40
Oh, my gosh.
Scott Benner 12:42
She says
Ginger Locke 12:44
I'm sorry. It was a missed call. I hit my phone five times on the site, because I thought it opened up the medical alert. info. All right. Thank you.
Scott Benner 12:57
Oh, my gosh.
Unknown Speaker 12:59
Okay. Well, we won't sprint. That was great. Please leave that in the podcast.
Scott Benner 13:03
Oh, I'm not taking anything out of the podcast. Don't worry.
Ginger Locke 13:05
Now it did open up my medical ID it was the third step apparently
Scott Benner 13:09
123 opens it? I don't know. But let's go again. Hold on. No, no, don't do it. I so I know two clicks is to open up an app like Apple Pay. And so I keep running into that. But I will figure it out. I'll tell you what, I will figure it out. And I'll put it in here. But, but I think it's gonna be of great comfort to the people who asked the questions that you do look, because I I mean, listen, especially for not, you know, it doesn't matter. I should say whether you're a parent or a person living with Type One Diabetes, your thought is Oh, my God, if my kids alone, is someone going to know if I'm alone? Is someone going to know? And and that kind of brings me to what should someone do when you arrive? And there's a person with diabetes who's struggling? What should I be telling you? Hey, they have type one diabetes, like what do you want to hear from people? That's, that's helpful and actionable. And what's too much? You know what I mean, when people start telling you their life story in a weird situation?
Ginger Locke 14:08
I, of course, yeah. Um,
Unknown Speaker 14:12
so generally,
Ginger Locke 14:14
we want to listen.
And that's called the ope that, that what you just said this telling them the life story that's called the opening monologue. And we, it's actually part of training to try not to interrupt that initial what's called the chief complaint. It's like, why are we here? What are what is, what is your need, and what are we trying to address? But I think of you, for example, being a parent of someone or having a family member who has type one diabetes, and let's say they were critically ill, I think because you've lived with the disease for quite some time. Now you would know to say they have diabetes, they're unresponsive. And then we're gonna do a little bit of work, you know, for a couple of minutes, but then also That additional info is going to be port important. Like when were they last seen, okay. And it's helpful to tell us that they have diabetes, but that that can also do something called I think it's called triage cueing where you're basically sitting us down a path. Accidentally. Yeah. So it's, it's good that we know, but we don't want to only think, is this just diabetes? Could this be also could this be something else? Could this be a stroke or something else? So
Scott Benner 15:29
it's funny, I employ a similar idea, when I'm interviewing people on the podcast, you don't want to say something that takes them away from their thought, or leads them to, you know, believe that they've come to some conclusion. And they might be false, you know, like, so. This person has type one diabetes, they use insulin, we just ate and now she's unresponsive. I think she had too much insulin, or she's generally like, would it help to know this is a generally healthy person versus someone who's struggling? But yeah,
Ginger Locke 16:00
if we know this is out of norm, normally, this is well managed diabetes, this never happens. This is something and then then we think, oh, that it's important that we know that the patient has diabetes, but maybe I don't want to get tunnel vision on that one possibility. I want to remember Oh, just because they have diabetes, doesn't mean they can have all these other health problems, right?
Scott Benner 16:23
And and indicate quickly, type one to type two as well. I'm using insulin not using insulin.
Ginger Locke 16:30
I think knowing that someone uses insulin helps because that means that they're at higher risk for sudden drop in their blood glucose levels, right hypoglycemia,
Scott Benner 16:40
so in an emergency situation that the person is not expecting. The difference between type one and type two is not as important as they use insulin or they don't use insulin because Metformin is not going to make you pass out for instance, like that. I get that. Okay. Do you guys use glucagon do you carry it? will use the person's How does that work? Yes,
Ginger Locke 17:00
I have when I was in the field, we had glucagon, we used it. And then I also had patients who had it at home and what could give it to themselves and they had already used like an auto injector to give themselves glucagon. And when I got there, they were starting to get a little better, right? It takes some time. So glucagon is, as your listeners, I'm sure now releases glycogen stores from the liver. But yes, we have glucagon for that. And then also for
some other things to look at actually
has indications for other non diabetic emergency close down
Scott Benner 17:35
GI tract, right. Is that one of the things that does I had somebody told me they use it in some surgeries to keep people to slow people's gi tracks down and oh, it's interesting. I guess it does a lot of different things.
Ginger Locke 17:46
Yeah, it very well could, as I'm thinking about kind of its mechanism of action. Yeah.
Scott Benner 17:51
Okay, so do you have any stories that stick out because I'm thinking about a close friend of mine who lived his whole life with type one and you know, fell out of bed because his blood sugar was low and broke his arm, you know, got so low that his family couldn't help him? I'm wondering if you have any that that stick in your mind?
Ginger Locke 18:10
I think the the extremes, right, the hypoglycemia is and the hyperglycemia. I think they all stick in my mind because they're pretty extreme presentations. Okay. Right. The DK a patient, that's a perfect, they're profoundly ill, those are ICU Intensive Care Unit, they're going to end up in the ICU. And so they're very obviously, profoundly sick. And same for hypoglycemia, right? When they're unresponsive or altered. They're those two decay and hypoglycemia are not very quiet presentations, right? They're very in your face. The one that's sneaky, is the hyper molar hyperglycemic nonketotic syndrome.
Scott Benner 18:55
We all know that one Tell me,
Ginger Locke 18:56
well, you don't know it, because type one usually results in DK whereas type two diabetes can result in this other hyperglycaemic condition when they're not. p todich. They're No, they're they don't have keto acidosis.
Scott Benner 19:10
But their blood sugar still super high.
Ginger Locke 19:13
Well, yeah. And so they're just sitting there actually, not looking particularly sick, because there's no acidosis but their blood sugar is very, very high, and they're very dehydrated, and all that.
Scott Benner 19:22
Wow. I know, I just had somebody on recently who talked about as they were going to decay. He described it as it felt like the devil was inside of them, just a burning chest and I thought he was gonna die just kept telling people when he got to the hospital, I feel like I'm gonna die. So that's crazy. So you guys have to show up in all of these situations. It really did strike me when you said earlier and I let it get by and I shouldn't have that you could go from a situation that's, you know, an overdose and get back in a rig and drive somewhere else and somebody cut their finger making you making dinner, and you're probably still all like, like, how do you how do you do level? Or is it not possible all the time?
Ginger Locke 20:04
I think the fact that it's work helps a little bit of you can be more objective right then if it's your family member, so that what you know what you just said that we, it's our goal to not really get to maintain just a little tiny bit of emotional or professional detachment, right? We don't get quite that we have empathy. But empathy can get so deep that you're actually experiencing the other person's trauma. You know, it's, that would be terrible. If you kind of went down that Yeah,
Scott Benner 20:34
you're there to help so far not to forget that right? Yeah, I have to say that
Ginger Locke 20:37
I think I think we have it tough, but we get a little bit of wind down and wind up time. So we get to, you know, clean up the truck and do a kind of tidying up and then wait for the next call. I think I've also I've watched er, Doc's that we'll be doing cardiac arrest in one room. And then minutes later, I'll see him in another room, just sit and talk him with a family member about something kind of mundane. And I'm like, that seems like a lot of whiplash.
Scott Benner 21:04
There's definitely a scope. We we came up on a car accident one time that seemed kind of benign. And we were told to, we were going to we're gonna have to extricate, they told us and as we were getting stuff together, I sneaked. I looked in the car, to kind of try to get my vibe for what it is we were going to do. And there was no one in the car. And so I turned back to the the officer on the scene, I was like, there's no one in the car. And he pulled me aside and said, it's an older woman, she was like, in her 70s. And she had not been wearing a seatbelt. The force took her into the footwell, and she was under the dash, like, folded in half under the dash alive. And I was I just that that was the moment for me, where I realized I actually did have it in me to hold it together and still do a thing. Because I feel like, if I didn't, I would have found out that one day, you know, I mean, like, I'd seen dead people dead people wasn't too bad. I've smelled burning bodies like that. That didn't get me too bad. But this one for some reason. Like as I as I was living through it, and then look back at it later, I was like, Oh, my God, she was she was broken in half, you know? And, and I still did my job. So that's like, cool. I might I might be okay at this, you know? Because was it that exact same thing? Because if anyone was going to go running and screaming, that would have been the time it was horrific, you know, really crazy. When a persons with another person with diabetes, say they've had or they're having a seizure? Is there a way to articulate this without you believing that they've odede? Like, are there words to use or not use so you don't get confused?
Ginger Locke 22:41
Hmm. So you're saying you're you're the person you're with is having a seizure? And you believe it's because of a diabetic origin right? hypo hyper hypoglycemia is what we call hypo. Right?
Scott Benner 22:54
Yes. Where they're unresponsive, or they're, you know,
Ginger Locke 22:59
yeah. You want to quickly communicate, hey, we're not doing opiates here. This is a part of the
opioid epidemic.
Scott Benner 23:06
Right? Right. How do you start with this is not narcotics, this is diabetes in a way that we'll believe it, because people will lie about drugs thinking that there's legal ramifications on the way right. Okay. Uh, no, yes, sure. I'm sure
Ginger Locke 23:20
they do. We try to get that you know, across to them that we would never end it's in fact illegal for us to as healthcare professionals to that's your protected health information. We try to communicate that but sometimes we arrive in uniforms that look a lot like cops and it's it gets real messy and confusing, or the cops show up also. Right.
Scott Benner 23:37
So they're there at the same time. Yeah,
Ginger Locke 23:39
um, I think, you know, saying that you know, the person that they have diabetes that this sometimes happens when they have hypoglycemia, and probably just saying if you're concerned about you know, recreational drugs we we don't use or we don't use anymore we haven't used today are just directly saying it. I think medics are incredibly non judgmental about recreational drug use. And they really just want to know what they're dealing with. They're not it's not zero judgment. And it's understandable that the general public wouldn't know that right? So clarity, just
Scott Benner 24:17
just just throw it out there. Yes, I'm, we're, we're This is not drugs. This is diabetes. Please think about that as you're going towards it. Or I know this could look like something else, but it's not. Does DK look like intoxication.
Ginger Locke 24:30
It can smell like it unfortunately. So you breathe off ketones. It has an acetone smell that to some people, it can smell like metabolites of metabolizing alcohol,
Scott Benner 24:44
okay, like fermentation almost.
Ginger Locke 24:46
Yeah, just kind of smells sickly sweet. Yeah, the way
Scott Benner 24:50
sweet breath is one of the ways we figured out my daughter had diabetes all those years ago. And then again, she was too so I guess I wasn't thinking maybe she had too much right brandy or something like that. That Okay, so there can be that. What about the combativeness with those low blood sugars? Like I've heard stories of grown adults whose blood sugars get low, not so low that they're unconscious, but then all of a sudden, they're like the Hulk and about half the weight of they can't think either and that situation.
Ginger Locke 25:19
Yeah, I've, I've run those calls.
Scott Benner 25:20
Yeah, what do you do?
Ginger Locke 25:22
Um, so often they're sweaty to a lot of
pale and sweaty and so
it kind of be I can kind of be a handful.
We have general approaches to what you might call an agitated patient or combative patient. I don't really like to use the word combative, I think of it as more agitated, like, it's often in fear, yeah, that people become so non, you know, not able to kind of follow along with the sequence of events that a normal person would
Scott Benner 25:56
lose the society, you know, I guess combative. I get your feeling. I didn't mean to cut you off. But combative gives the overtone that they're purposefully not Yeah, doing it. Right.
Ginger Locke 26:07
Yeah, I hate that word. Yeah, I prefer more agitated, because it gives you a sense of what's going on in their head, right, they're going through anxiety and
confusion. So
we basically have two, two approaches. One is physical, like if someone were truly combative, like swinging at you, there's basically two approaches. One is physical restraint. And the other is chemical restraint. And both can be used in conjunction as well. I think chemical kind of sedation is the humane thing to do, you wouldn't want to physically hold someone down, right? Because that could be dangerous for them. But then also just like, psychologically
terrible.
We usually try to give them glucagon or some dextrose, you know, we try to first discover that their blood glucose is level. So that means we have to stick them to get a little bit of blood. So that's sometimes exhausting. Just even get a little blood there. They're not liking that.
Scott Benner 27:05
I can tell you that even at a reason there's a spot in my daughter's blood sugar, will she'll stop caring, like the kids like in you know, I'll say hey, test your blood sugar shekel, I will. And then it say keeps falling. And it gets to a certain level. And you'll say like, Hey, this is becoming a problem. Like you really need to check and eat something at this point. And she'll get like, it's it for her. It's very jokey still, but she's like, well, if I die, I die. Like she and she's not being funny anymore. But she just gets into kind of like a it's like a twilight almost where she's just like, hey, whatever happens happens. Yeah, a little detached is a great way to put it or dissociate. And you kind of have to keep pushing her towards it or kind of, you know, take something to her and say, Look, do it now. It doesn't happen a lot. But I've seen it happen enough to to recognize the repetitiveness of it. Mm hmm. Let me ask you a couple of questions about about how people can help you if they're by themselves. So people want to know about tattoos, IDs, you know, watch bands, people now have like, you know, Apple watches and there's they make these little snap on things on the bands that people put stuff on there. a QR code bracelets, do you guys scan QR codes. If you're using an insulin pump with tubing, or you're on multiple daily injections, and you'd like to be on a pump, this little bit here is for you. The Omni pod tubeless insulin pump has been a mainstay in my daughter's life. Since she was four years old, she's been wearing it on the pod every day for I think about 13 years now. And it's been a friend in her life with Type One Diabetes. Not only is it tubeless, which is amazing, because you can wear it anywhere you can keep it on while you're swimming or bathing or playing soccer. You know, are you whatever you're doing with like friends or acquaintances, you get what I'm saying? adults, right? Like you can just keep it on. So you're getting your insulin the way you're meant to be while you're doing everything. But for those of you who are still MDI and you're like, I don't know, it's going pretty great. I'm sure it is. And I'm not pressuring you, you don't need an insulin pump. But I want you to think about do you get low, like at the same time every day, like three o'clock in the morning or something like that? Or do you rise up at the same time every day? How cool would it be to be in charge of your basal insulin to be able to make it stronger or weaker. So that things like that don't just, you know, quote unquote, happen to you. If you're always getting low at 1am you could set a basal rate that begins you know, like an hour or so before that would impact that. Same thing for rises that happened in the morning. All kinds of stuff. Being able to manipulate your basal insulin with a pump is next level stuff, being able to do it tubeless Lee, that's even better. But here's the greatest thing about on the pod In my opinion, I mean this, you don't have to listen to me. Because they'll send you a free, no obligation demo, you can try it on to see what you think. And then if you like it, you move forward with the process. And if you don't, it's no big deal. It's up to you. That's how it should be my Omni pod.com forward slash juicebox. Get that pod experience kit coming to you in the mail right now.
Guys, the dexcom g six continuous glucose monitor is maybe one of the most important tools you can have while you're managing insulin. Why? Because you can see the speed and direction that blood sugar is moving when you were the dexcom g six, you can see it right there in real time. And it's not just I'm rising, or I'm falling. It's I'm rising. And this is how fast I'm rising, or this is how slow you're falling. It's spectacular technology. Imagine you're just doing a finger stick and you find oh mama, my daughter's blood sugar. It's 135. He's at 135. And stable, is it going up? Is it going down? There's no way to know where the finger stick. But with dexcom. There is. And you can see it right there on your cell phone. They're saying I'm saying you can follow a loved one a child or a spouse, brother or sister on your Android or iPhone device. Not only can you follow them, but look at nine other people because the user can have 10 followers if they want to. That could be a school nurse, a babysitter, so many options. So many people who are able to help you with your blood sugar, hold on a second, my wife's walking in, okay, I got rid of her so that I could tell you dexcom.com forward slash juice box Dexcom is going to give you an honest chance to keep your stability where you want it, you're a one seat down. So the time that your blood sugar spends in range is greater. How's it going to do that? Well, it's gonna tell you what your blood sugar is, and how fast it's moving. And that's going to give you an honest chance to use your insulin. Trust me, it's how I do it with my daughter. And her a one C has been between five, two, and six to four coming up on seven years. There are links to all of the sponsors at Juicebox podcast.com. And right there in your podcast player. But for today you're looking for dexcom.com Ford slash juice box and my omnipod.com Ford slash juice box. So people want to know about tattoos, IDs, you know, watch bands, people now have like, you know, Apple watches and there's they make these little snap on things on the bands that people put stuff on there. a QR code bracelets, do you guys scan QR codes? Like what what's the good thing to do here? Or should I just put something on my wrist that says I have diabetes and tattooed right?
Ginger Locke 33:03
The main thing you want to communicate is that their blood glucose level should be checked, right? And so just saying diabetes even not even getting into the type, just saying that the patient is diabetic means we will. And honestly, even if someone's just has altered mental status, we check the blood glucose level. It's a screening tool, it's a very low risk high benefit screening tool to just take a little tiny bit of blood it's very inexpensive test to know and so even patients where we have very low suspicion that the blood glucose level is off.
We'll do your take that as readily as we would take someone's temperature
Scott Benner 33:40
for example on a glucometer and you test somebody's blood sugar. It's it's one of the basic tools.
Ginger Locke 33:44
It is a very basic vital sign. Yes. Okay. But to your question, I think it's a good one of you know, maybe how do you get that medic to check the blood glucose earlier in the call instead of I think of a call I had once where there was this older gentleman and he was having unilateral neuro deficits that kind of droopy on one side and we were so certain that it was a stroke. But then finally very late into the call we got a blood glucose levels very, very low. He was hypoglycemia and apparently hypoglycemia can cause unilateral neuro deficits which is bizarre to me. I don't know how that would happen. But it can and so we we miss understood what was going on with him till pretty late in the call. But the way to communicate that information to medics would be to me a necklace or a bracelet that is the universal way all the fancy tech stuff is nice and probably more aesthetically pleasing to the typical person that has diabetes is want to be walking around with those bracelets and necklaces on. But it's just it's quicker. When we see a necklace or bracelet that's got the little engraving on it that says
Scott Benner 34:58
yes, just say it's a bracelet sandwich Girl, you're looking at me now you're probably having such an easy time imagining that. But say I'm a girl and I'm wearing a bracelet that has charms on it. I can't just throw one charm on that's for diagnostic, you're not gonna sit and pick through my
Ginger Locke 35:10
I will never notice that. Right, right. And actually same with tattoos. So this was a conversation I had with other paramedics about do you ask them? Do you look at people's tattoos? And they said the general response was, yes, we noticed people have tattoos, we would not be looking at the content of what the actual image is until later in the call with a stable patient as a conversation starter. But it would never be I'm scanning this for data that can help me take care of this person. Right. So you're looking at it in a very with a different filter. So do you I mean, if it was tattooed right across the chest? That's what
Scott Benner 35:47
I was gonna say, right? Yeah,
Ginger Locke 35:49
it's pretty obvious. But if it were something subtle or small, it could very easily be missed. It's just
Scott Benner 35:54
right are acronyms in a sleeve of tattoos? You know, you're not picking through. But if someone had no tattoos, and tattooed around their wrist where you were looking for the bracelet, it's a type one diabetic, that's as good as a bracelet, you would think, right?
Ginger Locke 36:06
I don't think it's as good as a bracelet.
Scott Benner 36:08
Wow, because you're looking for the bracelet.
Ginger Locke 36:10
Because I'm looking at tattoos and thinking that's a tattoo. And I don't, there's no data in that for me, other than this is just a person that has a tattoo. Okay, but it I'm not looking at it for. I mean, sure, I may see it. And it may be helpful. But a bracelet is it's, you know, those really ugly bracelets that have the terrible chain and the rectangle, and they're just so uniform. And so kind of institutional looking. Those are the ones I'm used to seeing. Do you know the ones
Scott Benner 36:39
I do? See, what you're saying is the classic medical ID is what you're looking for, because that's just, it's what you're trained to do. It's what happens more over than not. And you're also in a heightened situation, at that moment to
Ginger Locke 36:55
correct. So you're, you're working on a little less cognitive bandwidth and somebody who's relaxed, and you may get there, it just wouldn't be as quick you. So you'll get there after you've done a couple of things and you're kind of your physiology is calming down and your field of vision expands a little bit, then you'll start noticing those little things. I've talked to people about their tattoos a million times, but it's when everything has stabilized afterwards.
Scott Benner 37:20
So if mike tyson got a face tattoo that said, type one diabetes, and you rolled into the room, and he looked low, you might just look at him and go, I don't see that and keep going, I get that I really do. And there's this extra thing that doesn't belong on the body. And that draws attention. It looks like all of the other things that sit do that job. And so that makes your brain stop and go that's a medical ID.
Ginger Locke 37:43
Yeah, right. It's about picking a lot of what we do is pattern recognition, because we're moving so quickly and thinking so quickly. And there was a study done for radiologists to find. They were told to find basically cancer on all these CT scans right in their black and white images. They're told to find cancer to screen these CT scans quickly for Do you see anything it looks like a mass chest CTS and because masses are cancer usually shows up as white on a CT, they missed. There are all these little black tiny, they place a tiny black gorilla and all the CTS and they did not see the little thin outline of a little black gorilla on a CT scan. Because they weren't looking for that they were looking for White. Okay, and so it's just what your body your brain kind of selectively notices and and the way a medic thinks is not to go hunting through tattoos, they're looking for other stuff.
Scott Benner 38:46
So I have a tattoo on my shoulder or my forearm and I'm wearing sleeves and nobody's finding that. Not until later from your
Ginger Locke 38:53
you know, you point to your forum. I think about that where we might put a blood pressure cuff or start an IV I mean, those arms are better than legs. If you're Yeah,
Scott Benner 39:03
you're not gonna get away not you're definitely not taking my pants off during this situation.
Ginger Locke 39:08
Sometimes Actually, we do make patients all the way naked. Just go hunting for what do you think? Yeah, injuries and stuff like that. But
Scott Benner 39:16
But okay, but but I hear what you're saying. How about in the car? seat belt? How about those things that go on the seat belts are stickers on the window? Do they kind of fall in this? How do I how do I brand my car say I've got a 17 year old driving with Type One Diabetes? How do I make it so that when you come to the door, you know, this person has diabetes?
Ginger Locke 39:34
I think even if it's on the car, I don't know that that person that is that person's car. Right? So we're often the way our mindset is we're thinking I want to keep all the possibilities open. So yes, I have this piece of data that says somebody put that sticker on there, but I don't know it's specific to this patient. So I don't know for sure that conclusively that that patient has diabetes.
Scott Benner 40:00
When we're buying when we are branding things is the caduceus the most like thing that makes you think medicine. It's that set the snake thing with the rod. I like that you said it like that. Yes, it is.
Ginger Locke 40:12
Yeah, yeah, that's the one in red. Oh, am I so
Scott Benner 40:14
old that I know words for things people don't use anymore? Is what I just started one.
Ginger Locke 40:19
Well, I was just kind of is, is is a good word I forgotten
Scott Benner 40:23
now I'm wondering why I know it. So, okay, so I mean, it's just like this add to that you can do as much as you want to hopefully trigger that emergency person's thought to like, oh, diabetes, but until they go through their process and do their things, there, they're not going to know for sure. Without that, that jewelry around the neck
Ginger Locke 40:46
around the wrist, or something in a wallet of someone
will help as well. So we
typically will look through a wallet looking for prescription, you know, medication lists, or names of, you know, some people have that they've had surgeries, certain type of implants and stuff in their body, they'll have little cards in their wallet that will find
Scott Benner 41:06
what about a lockscreen image? What about I push the button once the lock screen pops up? But it says Great,
Ginger Locke 41:10
well, that actually, this is pretty genius.
Scott Benner 41:14
Okay,
Ginger Locke 41:15
that's, that's pretty smart, because we will go to the phone pretty quickly. And I've watched at the hospital social workers really just the phone is the lifeline to getting to the family and trying to figure out who people are and kind of doing all that detective work.
Scott Benner 41:29
Okay. All right. Well, there you go. Finally, the cell phone, not ruining lives saving. I don't know if anybody's seen the there's that Netflix documentary about social media right now, that tells you everything about your phone that you already know is wrong, and how it's trying to kill you that you choose to ignore it because you love it. And it's not, it's not killing you immediately. So you're just like, I love my phone. Please stop saying bad stuff about it. Okay, let's see, well, while people are waiting for you to get there. Mm hmm. What do you think people fail to do in that time when they're panicking, like what could they be doing? Does that make sense? Is there something to talk about,
Ginger Locke 42:11
rather than saying what they've failed to do, I could just kind of list off some useful things to do. clearing a pathway between the road and where the patient is. So if they're in a back room, right, moving things out of the way just to get a stretcher through or even be able to walk through with bags, clearing that pathway. As far as sick and unresponsive patients that many have religious may have heard of what's called the recovery position, right? This is laying on the side that allows and if they were to have any vomitus or spit to kind of drain out of their mouth with gravity towards the floor, rather than back into their their airway. coming outside to meet the fire truck or ambulance is very helpful as well. Sometimes, homes aren't very well marked, or an apartment complex, it's may be hard to figure out exactly where you are as quickly. It could save, you know, a minute or two. Right? If you were to come out and be what's called a flagger where you kind of wave down the the
responding. It's a good
Scott Benner 43:14
idea. There really is no lights on on the outside of your house, stuff like that.
Ginger Locke 43:18
Yeah, turning lights on. That's that's a great way, especially at night when the lights are on. I'm like, Oh, I know. What's that house? Yeah. Because ever all the other houses look asleep at 330.
Scott Benner 43:24
In the morning, this house is lit up like I bet you they're the ones that called us.
Ginger Locke 43:30
That's a good one. Yeah. And then just then assembling medication lists, putting all the meds in a little baggie that we could take with us. Just kind of assembling some key stuff that if we needed to leave quickly, that stuff is all together.
Scott Benner 43:43
I guess too. If you're you're likely going to take this person with you. If they have some personal stuff that they use to manage their type one, they're going to want to make sure that gets in the rig with them and or somebody goes with them too, if possible. Do you like to take a family member if you can?
Ginger Locke 43:59
We do so COVID times is messed up all taken all the family members and things like that. But yes, let's talk non pandemic times. It's great to take a family member, especially with patients who are unresponsive because they're there all the info there. The patient's history. So we talked about when we do assessments, there's a history and a physical exam. And when a patient's not talking, you have zero history, and you only have your physical exam to rely upon. So they become the surrogate historian. Okay,
Scott Benner 44:27
yeah, no, that makes sense. Hey, when I call 911, can I say I need an EMT? Not just a paramedic? Will they take me seriously if I do that? Well, well, they'd be like, Hey, who are you buddy? I know you've seen ER and everything but you know.
Ginger Locke 44:43
So you said in reverse again.
Scott Benner 44:48
Alright, can I okay. So,
Ginger Locke 44:50
here is when you call 911. They will have already a pre planned response, right that is appropriate for whatever it is. Your job is to report what's going on where you are as best as you can, right as a patient breathing as a, are they breathing? strangely? Are they bleeding? Do they have a pulse? Are they talking? Those are the types of questions, very simplistic questions. And then the response will be kind of triage through dispatch about what resources should be sent.
Scott Benner 45:22
So I shouldn't get all obviously I definitely shouldn't. Because I'd end up asking for the wrong thing. I'd be like, I need the guy that went to more school and then I say it backwards. They'd be like, Oh, he only wants this. They send over for band aids and a nice cages on his first bag. Alright, so yeah, don't don't think this situation because obviously you're gonna do it wrong. And and be very clear about what's going on in that assessment when you're talking to 911. All right, that makes more sense.
Ginger Locke 45:51
And the first question that's usually asked is not what's going on, but where are you?
Scott Benner 45:57
Okay.
Ginger Locke 45:58
Like, are usually your location
knocked what's your we think they answer with what's your emergency? But it's not they want to know where you are? And then once they start hearing What's wrong, then they'll start sending people to that location? Gotcha. Because it mean, no one can do anything until we know where you are. Everything's on pause. Well, we know that
Scott Benner 46:21
you're in a medical crisis. I'm as if I'm the responder, my first crisis for me is getting to you. And then figuring out what's like you said, going through those checklists and getting to let's not let you die before we can figure out the bigger problem, and then stabilize you and get you to the hospital if that's necessary. Mm hmm. How many people? Have you treated with the diabetes situation and left behind versus take them with you? How often do people have to go to the hospitals that
Ginger Locke 46:51
for the hypoglycemic patients that are awake and talking and breathing when we get there? It's rare that we would transport them because what they need is food.
Scott Benner 47:01
They need to have it there.
Ginger Locke 47:03
Yeah. We will discuss you know, what may have caused the hypoglycemia? Was it too much insulin? Was it that you have an underlying infection that you didn't even realize? Or you know, and that maybe there's something more going on today? So it's not just a simple we fix your blood glucose level and lead? It's okay, let's explore why you became hypoglycemic. And are we all confident today, you just took your insulin and forgot to eat? Okay, that's the story.
Scott Benner 47:27
All right. No reason to pay for the, for the, for the taxi ride and going to the hospital and all that other stuff, because it's over. It's one of those medical things that once it's over, it's over, right. I know, my daughter had a seizure once when she was first diagnosed. And we, it was a Sunday afternoon. And we just gotten back from somewhere and put her in a crib. And she was she was napping after a car ride. And she just started grunting. And you know, it was clear she was having a seizure. We're trying to figure out how to use the glucagon. She'd only had diabetes for a short time, we didn't know what we're doing. We got our son who I think at the time was like seven, we got him to call 911. And we were messing with him the next day. I know there were a couple police officers in the house and and then you know, the emergency services were right behind them. And once we got her stabilized, we went to the hospital. And I think we were there for five minutes before my wife looked at me and when we didn't need to come here. And I was like, No, we didn't, did we and then by then it was too late. They had our insurance card already. And we already took the ride. So we just went over and and it was fascinating how little actually happened at the hospital where they were just like, well, she looks good now. So yeah, you don't want to do that. Again, it was sort of like that.
Ginger Locke 48:36
Well, that's a big trend in EMF not to go too far down the MS. Tangent, but I do want to say that emf is evolving and that the more education that paramedics are getting, the more independent they can be in making those decisions about where's the right what's where's the right paid place for the patient. Right. We used to be there's kind of a saying you call we haul, right? You just call us we're going to the hospital because we can't think for ourselves now. With more education really good physician oversight, we can have longer discussion about what's going on and create a plan that's right for you today. And not just this prescriptive, like everybody goes to the ER thing got it.
Scott Benner 49:13
Hey, um, a lot of people asked this question when someone has a low blood sugar you figured out they have a low blood sugar and they need food. Is it common to over carbohydrate them like to jam them up and make them super high because the people who are normally pretty cognizant about keeping their blood sugar stable in a lower range who've just had what they consider to be a you know, an emergency situation? They are not looking for you to make their blood sugar 450 but are you are you
Unknown Speaker 49:40
Why?
Ginger Locke 49:42
I love your question. I love the way you asked it. Yes, we are thrilled that you're no longer hypoglycemic. But, so if we're going to air we're going to err on the side of you maintaining consciousness and not becoming hypoglycemic. So sometimes Yes, that means we overshoot it,
Scott Benner 49:59
but you're not going to show up Go, hey, try these three Skittles and wait 15 minutes. So let's see what's happens you're gonna write,
Ginger Locke 50:03
you're gonna usually it's like poor, I, you know, can bring some orange juice, put some sugar in it, you know, it's like, it gets ridiculous. But we also give intravenous dextrose. Okay, right. So for patients that can't eat can't swallow.
Scott Benner 50:22
I know, it's something that
Ginger Locke 50:23
you haven't talked about yet, which is you've talked about glucagon, you've talked about oral kind of sugar. But then there's also intravenous, what we call d 50. It's 50%, water, 50% sugar, it's a lot of talking about carb load. So we used to just give like the whole thing. Now we've started kind of giving half of it, and then wait and see how that does not we do we are cognizant of the fact of trying not to overshoot them so so much, because that's, that's rough on you guys. Yeah,
Scott Benner 50:51
it's terrible. And then I wonder, too, with all the new technology that people with diabetes are wearing. It's a lot of people have continuous glucose monitors. So an ability to see their blood sugar in real time and how it's moving. Do you will you employ those once you're aware, and things have calmed down a little bit where you say, hey, let me see your blood sugar on that you would, okay.
Ginger Locke 51:12
And we're gonna double check it with our educational course. Yeah.
Scott Benner 51:15
But I mean, in easy way to say that, like this dextrose has gotten you to like 125. And it seems pretty stable. We don't have to push the rest of this. Yep, I got it. Okay.
Ginger Locke 51:25
And going along with the clinical presentation, too. So it's like, with the number looks good. And you are looking better.
Scott Benner 51:31
Right. So yeah, so the stuff that you would normally do visual check over. It's not just these numbers. Okay.
Unknown Speaker 51:37
Right. Do you
Scott Benner 51:38
have, like at one, obviously, I think you do. But when you're teaching your course, what do you tell people about assessing diabetes?
Ginger Locke 51:49
Um, we tell tell the many things. It's a whole module. But, you know, some of the teaching points are that this may be the first day that they've realized they have diabetes that they may not have known. Often it results in some emergency to for them to even become aware. Right. And so that's, that's an important thing for paramedics, I think, to understand that. People can be having a diabetic emergency and not even know they have diabetes. Wow.
Scott Benner 52:21
Yeah. I never thought of that. Like they're everybody's first time is somebody who is Yeah, everybody has a first time and not everybody ends up in the hospital, passed out their first time, they might just have some of the symptoms of high blood sugars. Yeah, it's funny, I think so much about the problems we that people have when they're being diagnosed because doctors offices, it's, it's almost disturbing to hear you talk about how obvious it is to do a finger stick to check on somebody's general health because they don't do that doctors offices. So a lot of kids get treated for the flu or other stuff like that for a long time, then end up in DK because no one took the time to just, you know, check their blood sugar very quickly.
Ginger Locke 53:02
You know, what's interesting about that is I I've thought about that same thing, because I've got two kids. And it bugged me that they weren't they didn't know my kids blood glucose level at any point in their life until I think maybe they check there's a there's a routine, routine screening age, I think they finally do check. I don't remember for eight or what, but it did bug me.
Scott Benner 53:23
Yeah, it's a huge problem. There's a lot of different organizations that try to help you there's these letter writing campaigns that go to like pediatricians offices and all these things, because a lot of kids you know, there are people who die every year from undiagnosed type one diabetes. And really, you know, when you look back on it, you realize that for whatever a test trip costs $1, maybe, you know that somebody just kept treating the flu, the flu, the flu, the flu and never looked that next step is it's disturbing. And that's why I felt I found it really comforting and interesting that you were like, Oh, we would just do that all the time. That's a great way to
Ginger Locke 53:54
find out routine. It is. I mean, it's not only our paramedics educated to do that is very routine, we work under kind of standards of care or protocols that are written and it is a very standard thing that any altered mental status patient, right, even if they're just a little confused, little grumpy, sleepy, lethargic, and so not just unresponsive, but altered mental status, that is a very routine test. And, you know, you said it's inexpensive, it's also low risk, there's very little risk. It's not it is very hard to hurt someone with a lens set.
Scott Benner 54:31
Right, right. Yeah, you're gonna be okay. That's
Unknown Speaker 54:36
the high yield low risk test to make sense.
Scott Benner 54:38
So when people have a higher blood sugar, so you get there and you assess them and they're not DK but their blood sugar's 500. Do you help them? Like do you want them to have insulin? Or do you leave it to them? Or do you just say, hey, look, you don't have enough insulin? What if you get them What if you have to transport them do you carry you don't have to carry insulin with you.
Ginger Locke 55:00
It's a great question. We generally in the outer hospital setting, paramedics are not using insulin No. And it's because it's a very strong drug that does other things besides move glucose into the cell, it also affects other electrolytes and things like that. So abrupt changes, someone's really hypoglycemic and they take a ton of insulin that can do a lot of other things to their body, besides just fixing their blood glucose level. As I said earlier, and you guys who are listening know it's a these are very critical care, very fragile, sick patients. And so insulin is not a very common out of hospital. medication. Yes, yes. I can think of a few maybe remote places where it's used, but nope, not on the trucks in. In Central Texas,
Scott Benner 55:44
would you turn to the verse and say, Look, you have insulin here? You should probably take it as your doctor has instructed? Or do you don't mean like, you're obviously not going to give it to them? I guess? Because you don't know any other way.
Ginger Locke 55:56
I wouldn't even know I don't even know all the scales and all that stuff. I don't know how to do it. Yeah, I would be because of kind of my lack of knowledge about, you know how much insulin it takes to get someone's blood glucose level? To me. 500 is the number use is a pretty scary one. And I would be afraid it's not just simple hyperglycemia? I'd be worried is there more going on. And I would not be comfortable if they if they? So usually, if someone's quality msmes are sick, they don't feel well. Right. So to also see a blood glucose level of 500. It's like, okay, I want to make sure you get screened for many things at the hospital that I don't I feel a little out of out of my
Scott Benner 56:38
zone on that the word purview kept coming into my head, like that's outside of your purview. What?
Ginger Locke 56:42
A little bit, just because it's like 500, or you're pretty sick? And if, depending on your clinical presentation, right? If you look really sick, yeah. And there may be more,
Scott Benner 56:53
I guess, you have one problem you're dealing with, you don't need to add a secondary problem before you get somebody to help, right. But let's just interesting, like, you really are there for an emergency situation. So if somebody called you in that scenario, you got there and said, Look, you know, this is what your blood sugar is, it looks like you probably need to be checked for a number of different things. I can take you to the hospital if you want, or you should make your way to your own physician, or I guess there's a lot of different. It's interesting, your job is very specific. Yeah, we
Ginger Locke 57:22
we talk about paramedics, our healthcare navigators, so they're not just responding to emergencies. They're responding to people that aren't sure what to do next, with wherever, however, they found their condition to be and so maybe they're new, newly diagnosed, and they're not very good at taking their insulin, if it's daytime, and we can call their doctor and talk through all of that, then sure, but if it's the middle of the night and
Scott Benner 57:46
can't get a hold of people, then maybe then the hospital becomes the way
Ginger Locke 57:49
Yeah, and you you know, maybe they have a headache to go along with it. Well, headache can be a lot of things that I can't test for, like meningitis or strokes, right. So there's so many things in that hospital setting that we can't test for that we do end up taking a lot of people to the hospital for additional testing, when, you know, we can't really get in touch with their primary care physician.
Scott Benner 58:10
Do people try to use you improperly? Meaning Do you ever get to people and this is away from diabetes, I'm wondering this, and they clearly need a hospital but don't want to go to the hospital, you have no power over that. Right? If I refuse to go I just that's it.
Ginger Locke 58:25
Correct. If you don't want to go to the hospital, I'm not kidnapping you and taking you anywhere you don't want to go as long as you have mental capacity, right? So as long as you aren't incredibly intoxicated, or unresponsive, or something's in a way that you like you're not making your judgments impaired.
Scott Benner 58:43
So you can make medical judgments about their ability to make judgments for themselves.
Ginger Locke 58:48
So if I say we do it a directively with tests like Do you know what day it is? Right? Do you can you explain to me what's wrong with you today, and that you're preferring to stay home? And you understand that you might become worse and die here in your home? Or you if they can explain it back to me then.
Scott Benner 59:05
Then that side everybody's got their own freedom. But now if I say I don't want to go to the hospital, then I pass out are you allowed to go ups? Oh, well, I've been put them in the truck
Ginger Locke 59:13
is called it's that it's called implied consent. And the idea is that a reasonable person would want to go to the hospital if they had known they were about to become unresponsive, right?
Scott Benner 59:22
Oh, that all makes sense to me. Okay. Is there anything I didn't ask you or that we didn't talk about that I should have to answer these questions for people, which by the way, started out with our medical tattoos, okay, and then turned into all these great questions from everyone.
Unknown Speaker 59:40
Um,
Ginger Locke 59:45
I think you know, you're asking how does how do you signal to somebody come into your home that someone in the house has diabetes? I think the probably the top places are a bracelet in your wallet, the refrigerator Another place we go look on the front of the refrigerator, people will put lists of medications and stuff. Yeah.
Scott Benner 1:00:07
So my last question, which a lot of people ask, because of the timing of when I put this out into the community, and when everybody started asking the questions, there had been something in the news recently, where a gentleman had a very low blood sugar. And the, I guess the people who showed up his house, were just certain he had odede. And would not listen to the other people in the House about it. What do I like? What do I do? If if like, really like, Is there something you can think of that would snap you out of that mentality? If you were thinking this is drugs? This is drugs, and I knew for certain it wasn't like, what do I do to get you to stop thinking that way? Because timings of real issue at that point.
Ginger Locke 1:00:44
Yeah, I love the question. Because you're talking about cognitive pitfalls. It's not that these people are jerks, right? The medics that come to your home, they got into ms because they want to help people. And they're not just jerks. But they can if they've run, you know, maybe they're in a community with an opioid epidemic. And they're, you know, that's 2020 calls back to back to back to back, they kind of get their brain gets stuck, as you said, So what can you do to get them unstuck? There's this really great book called how doctors think, and it might be something you know, and your listeners are interested how doctors think is really neat, because it talks about how clinical decisions are made. And it's recommended to ask of your doctor. What else could this be?
Scott Benner 1:01:30
Okay, that's that's phrasing that gets them to start thinking a different way.
Ginger Locke 1:01:34
It's like, okay, right now you're thinking overdose. But what else could this be? And it just opens up their brain to
the possibility and a reminder of the
fact that other conditions can look just like this. Ah, so you're
Scott Benner 1:01:48
tricking them into doing their job that they are somehow stuck in can't figure out how to do I love language? I really do. I think sometimes I get done an episode of this show. And I'll listen back when I'm editing and think, like, I'm proud of myself how I got someone to something without telling them to go to it or, or fooling them into understanding it, but just sort of asking a question that makes them then think about something different, and then see where it leads them. And that's really what you're saying, you're somebody gets stuck on this idea. This guy, he odd, odd, odd drunk or whatever. And you start, you just kind of break that you break that, that pattern he stuck in, or he or she or stuck in, and then you you get them thinking about something different. That's kind of brilliant, and simple, isn't it?
Ginger Locke 1:02:36
Another pitfall is that we forget, it can sometimes be two things. And so it could be opiates in this case and diabetes the patient could be having experiencing both, right? And that's probably one of the harder things because we love the binary, it's this or that. And
Scott Benner 1:02:55
it's like the most human thing. Pick one who wins either or black or white. Be both. Can I not be high? And my blood sugar be low? No, he's a good guy. It's his blood sugar.
Ginger Locke 1:03:07
Yeah, yeah, no, no, I hear that. Once we once we find the cause that there's something called the I think it's called the second fracture phenomenon where, let's say you, your arm hurts, and you've been in some type of car wreck and they find a fracture in the arm. They're like we've done testing, we found the cause, well, sometimes there's a second fracture that gets missed on the X ray, that they just don't see because they think they found the cause. So same for
Scott Benner 1:03:33
this. No, it's almost like anecdotal evidence, like you feel like you've got the answer. So you stop wondering, gotcha. This is excellent. And now it's making me if I can make me wonder if I can get Jerome groopman, the author of How doctors think they come on the show. Because that's, I think, this that this specific thought translates into people's personal doctor's visits. Oh, yeah. You know, when you get into the room, and you realize, like, you've got this whole thing figured out, and they don't see it that way. And then you just sit there feeling defeated. And instead of another one,
Ginger Locke 1:04:02
as you're saying that another one I've used with my own doctor, is I'll say, How do we know it's not x? Right? So I have asthma sometimes. And I'll say to my doctor, how do I how do we know it's not pneumonia? Or how do we know this isn't?
whatever other respiratory disease? Yeah, and
Scott Benner 1:04:21
you're not asking so much for him to tell you how he doesn't know you're asking him so he'll think it through again.
Ginger Locke 1:04:27
Think of all the tests that might need to be done or not done.
Scott Benner 1:04:30
Yeah. Damn, ginger, you're pretty smart.
Ginger Locke 1:04:32
This sneaky.
Scott Benner 1:04:35
By the way, you live in the part of the country that I often tell my wife, we should run away and go live there. But I guess other people think that too. And you're probably all very sick of us coming there. So I won't say it out loud.
Ginger Locke 1:04:45
But well, you're very welcome to come.
Scott Benner 1:04:48
Thank you. I'm looking for lower humidity. Not so much snow. Is this the place or no,
Ginger Locke 1:04:52
there is pretty low humidity and definitely no snow. I'm
Scott Benner 1:04:55
on my wife's. Alright, just give me your address. And I'll just I'm gonna pack up right now and go Because I am tired of the snow, and I am tired of sweating just because it's June. So I'm done with it. Now, I don't mind a dry heat. I just don't want to be wet. While it's happening, you understand? Hey, tell everybody about your podcast.
Ginger Locke 1:05:14
Sure. It's called medic mindset. And what's neat is it started as a podcast for paramedic students, but the paramedic started listening. And then I got some medical directors who are emergency medicine, physicians listening. And so suddenly, emergency medicine kind of residents or med students started listening. So it's, it's expanded to, to reach beyond kind of its original intention. And it's, it's, I really spot one episode a month, something I really enjoy just talking to paramedics or people that work in emergency medicine about how they think through problems, errors they've made, why we you know, kind of the cognitive theory about why they may have made that error.
Scott Benner 1:05:54
That's very cool. Isn't it interesting how you start something like that, and then it grows, and it finds other avenues to help people. And like I told you at the very beginning, I started this podcast because I thought my blog was kind of dwindling, because people stop reading. And it's got millions of downloads now. I love that crazy, isn't it? Like I just I love that it helps people and it was just a very unexpected treat, I guess at how well it worked out. Um, so I'm really glad for you. And I'm gonna I'll put a link in the show notes. And and hopefully there's some people listening to this that that might come over and check you out too.
Ginger Locke 1:06:28
Nice. Yeah. Thank you so much. You're welcome. Thank
Scott Benner 1:06:30
you for being By the way, as we're as we're wrapping up here, thank you for being how you are, because I just was at my son's baseball game one day. And I decided, like, I'm going to get somebody on to talk about this who, who's got a podcast that talks about this stuff all the time. And so I'm have my headphones in, and I'm sitting in a chair under some shade, because like I said it was human. And I'm like, like, oh, here's one I tried listening a couple of people in there, you know, but I got to you and you were measured and thoughtful. And you had a nice clean microphone, I could understand you and then I started reading like reviews. And then I just started listening to an episode and I was like I would like it if this person was on my show. So you want out I didn't just like I didn't throw a dart at podcasts about this I really listened and I think you're doing a really great job not that what I think means much But
Ginger Locke 1:07:20
no, I appreciate that. It actually means a ton because
your podcasts yourself so you know kind of what you value in and talking to you what this has done. I was hoping to get to hear more about your daughter and your journey. So what this has done is made me now I want to go back and and hear your previous episodes.
Scott Benner 1:07:37
Oh, cool. Yeah, I do everything so that people will listen, everything's just a carrot on a stick to get you to download my show. I need listeners dammit. Keep listening. Tell people. No. But But seriously, I appreciate that. I'd be happy to tell you more about it. But I know we're up on time. And I you have children who I think at one point I heard outside going Hey, when's this over? So go live your life. And thank you very much. And I really I can't thank you enough. This was wonderful.
Ginger Locke 1:08:05
Thanks, guys. I appreciate you
Scott Benner 1:08:06
having me on. Oh, absolutely. Hey, huge thank you to ginger for coming on the show. And thanks so much to Dexcom and Omni pod for sponsoring this episode of the Juicebox Podcast. You can go to my Omni pod.com Ford slash juice box to get a free no obligation demo of the Omni pod tubeless insulin pump. And to learn more and get started with the Dexcom g six go to dexcom.com Ford slash juice box. And please don't forget to visit touched by type one.org there are links to all of the sponsors in the show notes of your podcast player and at Juicebox podcast.com.
Would you like to hear more from Ginger? Check out medic mindset wherever podcasts are available. Or go to medic mindset.com her shows available on Apple podcast Spotify everywhere that you listen to this show. You can listen to ginger and medic mindset

Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#386 Podfather
The Pod Father
John Brooks is the father of a type 1 diabetic and the guy who developed the Omnipod.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Alexa - Google Play/Android - iHeart Radio - Radio Public or their favorite podcast app.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:08
Hello friends and welcome to Episode 386 of the Juicebox Podcast. Today, I bring to you a conversation with john Brooks, one of the men who sitting on an airplane over 20 years ago, conceived of and dreamt about, for the very first time, a tubeless insulin pump. Eventually that pump became the Omni pot. And this is the story of how it came to be. John's the father of someone who has type one diabetes, and
Unknown Speaker 0:39
he tried to figure out how to help
Scott Benner 0:40
a long time ago when his son was diagnosed. This is what came of it. It's kind of crazy, right? While you're listening, please remember that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise, please always consult a physician before making any changes to your health care plan, or becoming bold with insulin. John's actually been involved in a lot of things around type one diabetes, we'll talk about all of it. But my initial reason for having him on was to learn about the birth of the Omni pod. An interesting idea, isn't it? Just something didn't exist? And then it did.
Hey, if you're looking for a great way to support people living with Type One Diabetes, while you support the podcast, go to T one d exchange.org. forward slash juicebox. And join their registry, you'll answer a few simple questions about you or your child who has type one diabetes. And those answers will help support innovation in the type one world. It's that simple. It's completely HIPAA compliant, absolutely anonymous, you can opt out at any time. And it takes less than 10 minutes to complete right there from your phone, or your computer. T one d exchange.org. forward slash juice box. This episode is also sponsored by touched by type one. Good a touched by type one.org. To learn about an organization that is doing an incredible amount of good for people living with Type One Diabetes. Touch by type one is also putting out there good stuff on Facebook and Instagram. As a matter of fact, I believe the founder of touched by type line just had a beautiful little baby. So if you're interested in seeing cute little babies definitely hit up their social media touch by type one.org. Do you have a great doctor or need one? Check out juice box docs.com. It's a great list of doctors who have been suggested by the listeners of this podcast. The doctors that get it when you want to make adjustments to your insulin, but don't want to just do you know what everybody else does. juicebox docs.com leave a name. Take a name. If you're looking for those diabetes pro tip episodes to share with a friend. It's easy to get them to download an app I guess and say hey, started Episode 210 that's where those diabetes protests begin. Or you can just send them to diabetes pro tip.com. And please help me welcome a brand new sponsor to the weekly shows. g vote glucagon. In the next few episodes, you'll begin hearing about yoke. Arden has already got it at home. We've got the hypo pen, and it's the bomb diggity. The absolute minute I heard there was a new glucagon that did not have to be mixed. I wanted to know more. You can learn more at GE Vogue glucagon.com forward slash juicebox ge vocus GVOK eat glucagon classic way gl ewca. And that might have been wrong. glucagon. Dear God, are we gonna get involved in spelling glucagon right now? All right. GVOKEGL Uc, ag o n.com. forward slash juicebox. Or you could just you know, use your own brain instead of mine and just type it out. g vote glucagon.com forward slash juicebox. Welcome to the show, g Vogue. T one t exchange.org. forward slash juicebox. And of course, touched by type one.org. Check them out when you have the time. I appreciate you doing this very much. I've often wondered about you, not knowing who you are. And I thought this is an interesting time to get your, your thoughts. I mean, if I'm not wrong, right, it's not 20 years since you started the company, right?
John Brooks 4:55
Yeah, it started instantly. In fact, it's funny I was just on the phone like 10 minutes ago with, you know, my co founder and partner at prism, Dwayne Mason's. So we were just literally talking about that 20 years ago, 20 years ago in May 2000.
Unknown Speaker 5:11
Yeah. And now
Scott Benner 5:12
everything is getting ready to. I mean, I don't know how to think of it, they're gonna take the thing you guys made and supercharge it, right. Like, it's, it's getting ready to take a leap, don't you think?
John Brooks 5:22
Yeah, well, you know, I think, you know, if you think of the world that, you know, we started in, it was a device, right, a glucometer. You know, that? Well, a glucometer, you know, was then gonna drive an insulin pump. And now you look at it, you know, it's the whole closed loop, it's the automated insulin delivery capability. But I think what's most important is the fact that it's less about the device, it's really the data, and it's the use of that data to drive better decisions, better clinical outcomes. And I think, you know, with COVID, and the way healthcare has changed, you know, people want to be able to kind of get health care in their terms, you know, they don't want to feel like they have a job to manage your diabetes, but you know, the more of the burden we can take off of them, they want in today's environment, you know, people are more prone, they don't want to go to the doctor's office, they don't want to go to the clinic, they don't want to go to the hospital, you know, that they want to be able to, you know, get help and coaching and support for managing their diabetes, but on their terms, and, you know, I think that's the beauty, whether it's insulin or others, I mean, you know, really leveraging the data, the analytics, the ability to basically determine, you know, trends to be able to look at time and range to be able to look at, you know, where there are any hiccups, or, you know, risks of hypoglycemia. So, you know, it's kind of the evolution of healthcare that, you know, if there was a silver lining to COVID, its accelerated, you know, all this virtual care, remote care, connected care, you know, much faster than, you know, it would have happened on its own, it was pretty, pretty slow. And now it's, you know, changing dramatically.
Scott Benner 7:08
So in the beginning, really, the, it's about, it's a tool, and the tool is the whole, it's the whole story. And now really, the tool is just the way you take the data and and make the decision. And then you don't have to go back to the doctor who would look at whatever data you had, whether they were finger sticks, or log books or CGM graphs, as time goes on, and say, Look, I think you should turn this knob here make this small adjustment. Now the data kind of understands that for you, I guess.
John Brooks 7:34
It's Yeah, I mean, you know, it's pretty much I don't want to say autopilot, because we're not quite there yet. But the idea is that, you know, the algorithms, you know, the systems get to know you, they get to understand, you know, kind of what, you know, what you do, a lot of people tend to do similar things day after day, whether it's their eating or whatever. So at the end of the day, you know, the devices are going to become smarter and smarter and more predictive. And they'll try to determine not only what the right insulin dosing is, but, you know, based on your prior history, you know, based on what they've been able to track, you know, they can almost anticipate, here's what's going to happen, and, you know, kind of get ahead of the curve. So, you know, I think it's the power of AI, it's the power of analytics. And then to your point, you know, you know, in the early days, I remember at jocelynn, you know, you'd have doctors having to look at, you know, printouts from all the different flavors of bgms, there was, you know, a few folks on CGM, you know, you had some ability to download data off of a pump, but none of it was connected, none of was integrated, none of it was aligned, you know, there was no even understanding of the dates on all the devices were the same. And obviously, everything got shifted every twice a year when there was daylight savings time. So, again, I think we've come a long ways and, you know, more to go because, you know, the sad part is, despite a lot of great technology advances, you know, we still do not have enough people with diabetes, especially people on insulin, you know, meeting their objectives, you know, getting their time and range. I mean, you know, and again, I think it's an appreciation that, you know, despite the fact we're making advances, you know, there's more to you know, managing diabetes and just tracking blood sugars, you know, standing now more about stress, understanding more about sleep habits, understanding more about, you know, the food, we eat, nutrition, and even the whole behavioral mental health aspects of diabetes. So, so the good news is, you know, I think we're getting smarter. I think we're getting there. But you know, like anything else, it just doesn't happen overnight. Yeah.
Scott Benner 9:50
Well, let's kind of walk down memory lane for a second. So tell me a little bit how you How did you come to this and like you were saying before, like, I guess that kind of Concept wasn't as much about the pot at first as it was about, just take me to the beginning, like, what were you doing when this happened? Yeah.
John Brooks 10:06
So, um, if I kind of walk back 28 years ago, or then three year old son was diagnosed with Type One Diabetes, okay. And certainly, you know, no real, immediate family history, you know, I didn't quite understand how that came about. And we were living in Colorado at the time, I was working for Pfizer, on their device business. And, you know, I decided that, you know, I need to try to understand, you know, diabetes, both type one and then eventually type two. So, you know, as my career and life advanced, you know, diabetes was always an important component. And, you know, when I, you know, when Pfizer ultimately divested themselves from all the device businesses, they were in, I came back to Boston, I was a co founder of a venture capital firm, called prism, venture partners. And, you know, that's really what I said, in the early days, you know, you know, we were looking at, I was looking at, you know, companies that we're trying to work on, you know, non invasive glucometers, you know, people are trying to work on, you know, how to determine glucose, you know, in a very effective way. And, you know, and then, you know, as I said, you know, a little more than 20 years ago, you know, my partner and I were on a flight coming back from the west coast, and I was describing, you know, the challenges with, you know, trying to figure out insulin insulin delivery, and, you know, the problem with the existing, you know, pumps as they were back then, you know, with the tubing and the priming and the all the issues, and, you know, we kind of brainstorm that entire five hour flight, you know, and thought about, you know, how do we come up with a, you know, small, disposable insulin delivery system and the disposability happened to come out of a nother deal that we had done leveraging technology out of Sarnoff Corporation, which is where the RCA color TV was invented, if you will, and they had an interesting technology for a disposable hearing aid. And, you know, that's another whole story, I won't get down there. But, you know, we had the idea that disposability could be a very disruptive innovation, the idea is that every three days, someone puts on a new pod, you know, we knew we could, you know, hopefully do that in a very cost effective way, eliminate all the problems with the two meeting and the priming. And so you know, that that's kind of where the idea came from. And, you know, we got off the plane, the next day, we called up our patent attorney and said, Hey, we have this idea for a disposable insulin delivery system. And he said, Hey, no one's ever thought of that. And, you know, we got a whole bunch of IP, and then we went to our, you know, fellow partners in prison and said, Hey, we want some seed money, to kind of flesh out this idea of get it off the ground. And, you know, we did that. And, you know, we hired some people that had worked for us beforehand, we set up shop up in Beverly, Massachusetts, had a couple people and pretty much told them, you know, in the early days, just think about all the ways you can do this, think about all the ways to create an IP position, you know, and then little by little, we, you know, had more ideas, we had more IP, we had more prototypes. And then, you know, we went ahead and started to, you know, put together a management team, you know, build on the engineering team, and, you know, little by little, we brought other investors in, and, you know, here it is what, you know, 20 years later, you know, very successful in a multi billion dollar market cap company that, you know, continues to drive innovation, but that, that was kind of the germination of it. And then, you know, as I said, you know, and most of my career since then, you know, continues to be very heavily involved in diabetes. I had the opportunity, I guess, was probably about eight almost nine years ago to run the Joslin Diabetes Center as CEO. So, you know, somewhat unusual to have a fellow that I'm a UMass Amherst, graduate, undergraduate, and accounting, finance and systems. So, you know, you can see I learned enough over the years to be dangerous to be able to run a leading academic and medical research Education Center. But again, you know, it was part of, as I said, 28 years ago, I was bound and determined to try to understand, you know, how did my son get diabetes? And, you know, is there an opportunity to think about a cure and then, you know, as I get further involved, you know, came to appreciate that, you know, certainly type one is a challenge, but, you know, the whole epidemic, you know, I used to call it a pandemic of type two diabetes. with, you know, close to 400 and 60 million people around the world. So, anyhow, I could go on and on. But no,
Unknown Speaker 15:05
it's amazing how it came about.
Scott Benner 15:07
I'm wondering how, how long after you, you you take that plane ride? Are you holding a prototype?
John Brooks 15:14
It's a good question. Um, it was probably, yeah, I want to say probably nine months to a year, I mean, because, again, we spent a lot of time I mean, you know, we probably had some drawings and ideas, but, you know, we wanted to really think about the intellectual property to make sure we had a good patent position, you know, we wanted to make sure that, you know, we had a clear understanding that whatever we did, you know, we needed to have a, you know, kind of a novel way to engineer it, because, you know, most pumps have a motor. And, you know, you're thinking, if we have a disposable device, that, you know, we said, Hey, this thing's gonna have to, you know, cost less than, you know, I think it was, I don't know, maybe 15 $20. You know, and we said, well, you know, if you put a pump in there, you know, that's not going to do it. And then, you know, we thought about how to, you know, basically deliver very precise amounts of insulin. And in fact, kind of interesting enough, you know, we went back to sawn off and said, Hey, here's our problem. And they actually come up with the idea of a heated wire, which basically, is the mechanism that enables when you heat the wire it, you know, stretches and shrinks, and that ended up being kind of the mechanism to deliver the insulin very precisely, and in a very cost effective manner. So lots of, you know, as I said, I'm sure we have prototypes and ideas along the way, but, you know, it was more important to make sure that not only did we have a great design, did we have a design that was really gonna, you know, work, especially for kids and others. You know, we used to call it hassle free. So we didn't want priming, we didn't want to being, you know, we wanted to have a very easy way for the canula to get placed. So you know, it was iteration and it took, you know, it took a while, and then you got to figure out, you know, how to really make sure it works, you figure out what the regulatory requirements are? How do you make sure how we get the insulin in? How do we make sure that, you know, we can communicate, so, you know, lots of lots of steps along the way. So it doesn't happen overnight, and I took a really long process it were
Scott Benner 17:27
there points along the way, where you thought, we'll just get this to a certain point and sell it to somebody else. Did you ever think you were gonna be the company that made the pumps and sold them?
John Brooks 17:37
Well, I, you know, I think we did, you know, you know, we thought, Hey, this is a very, you know, novel idea. And, you know, we felt good about, you know, as we did some early interaction with, you know, customers and focus groups. And we had, I think, from the very beginning, you know, thought about the fact that this was the type of product that would lend itself to high speed automation. I mean, we actually thought, you know, at the time, we had set shop in trying to think where we were Bedford, I think, at the time, and after we left Beverly, where we started, and, you know, we had the idea, hey, we're gonna have a light sound factory, all these pumps are going to put to be put together by robots. Right, you know, and, you know, and then, you know, in some ways you go full circle, I mean, a lot of what takes place today, both in this great new factory that insulin built up in Acton, you know, a lot of automation, you know, lots of ways to produce, you know, massive numbers of pumps that are high quality. But you know, the answer your question, you know, I think we always stopped that, look, you got to build a great company, and maybe along the way, is someone likely to look at it. I mean, you know, what a Medtronic would somebody else say, Hey, this is interesting, but, you know, at the end of the day, I think we said, let's, let's do this, and I remember, you know, some of the greatest moments, you know, when I was a jostling member, we had a lot of Jocelyn had the Joslin camp for boys out in Oxford baths, and it was right next to the camp for for girls, but you know, seeing all the kids, you know, with their pods on swimming in the pond, I mean, that was pretty neat. Because before that is you know, you know, you're gonna disconnect your pump, you're gonna take it off, you know, you can't get it in water if you're using a traditional, you know, to pump and all so, you know, so I think we were always motivated by the fact that hey, this is a better way to help not just kids but families and people that want to get insulin and you know that they want to do it in a way that you know, it's discreet, it works for them. And they don't have to worry about all the hassle that you know, some of the other two pumps, you know, have gotten better but still exists.
Scott Benner 19:57
You know, my daughter has been wearing it on the pod every for 13 years, so, I'm completely aware of the just the benefits of just having your basal insulin while you're in that pond, you know, so amazing as before,
John Brooks 20:10
you know, kids would take the pumps off, and you know, it's a hot summer day, and maybe they even put them under the towel. But you know, the pumps are getting warm, and you know, maybe they're not wearing them for a certain amount of time. I mean, at the end of the day, that's just not good therapy. Right. Right
Scott Benner 20:25
now, it's 100%, I actually, I, I've been through the new manufacturing facility, I've taken that it's amazing, right? It's unbelievable, just astonishing what they accomplished. And, and watching it happen. And like you said, like, you know, things are kind of moving around automatically. And it's, it's not, and I don't think the precision is, is considered like, I want to try to understand without getting too like geeky and technical, you're telling me that inside of that pod, there's not a pump sending the insulin through the kanuma? It's,
John Brooks 20:57
yeah, so it's basically a mechanism that emulates a pump, but it's not a traditional pump with a motor and all. So, you know, so it's a different approach. And, you know, and I'd say, that's really the other, you know, key thing about, you know, being able to produce the number of pods that are needed, you know, where, you know, replacing them every three days. And so, you know, I think the other important thing was to, you know, put a lot of focus on dimensions, tolerances, the tooling, I mean, you know, that this is a product that, you know, that the tolerances are critical, the, making sure you're working with the right vendors, the vendors deliver the right product, and, you know, because we did have, you know, in the early days, you know, there was always a little bit of a concern about, you know, could we, you know, batch the batch consistency, you know, in the early days, we used to joke, we were shipping dollar bills with every pump, you know, because we didn't have the volume, we didn't have the scale, we didn't have the full economic benefits. So, but, you know, that's part of the learning curve. And then when we, you know, that they went to a generation to, you know, which was smaller, more precise, and more, you know, kind of cost effective, you know, that there were some hiccups in the early days, when, you know, you know, things don't quite go the way you expect, then, you know, you just kind of work through them, and hopefully, you know, convince your loyal users that, you know, Hey, sorry, and, yeah, we'll send you some replacements Hang in there. But, you know, the good thing is, I think that's all behind the company now. And I think now they're focused on, you know, kind of what I'd say is there, you know, Gen five product, they've got dash, they've got horizon. I mean, there really, as I said at the beginning, you know, recognizing that it's no longer just about delivering insulin, but it's the context of you know, doing it in a way that understands how that individual was living there live understanding, you know, kind of what their you know, smart CGM and other devices are saying and, you know, optimizing, you know, what their requirements are, so they're staying in range, they're avoiding hypose and hyper Roisin in their care team can continue to kind of fine tune, you know what they're doing. Did you
Scott Benner 23:23
are you still involved or did you eventually sell your share? Or how did how does that
John Brooks 23:27
Yeah, so when I went to the Joslin, you know, I just made a conscious decision. I think it was certainly the right one. You know, maybe not economically, but I i divested all my shares I you know, I just because we were doing some things and, you know, if you're the CEO of a not for profit with the prestige of Jocelyn, I just didn't want to have any perceived conflicts and also, right. So, you know, I'm happy to say today, I'm still an owner, but, you know, I pretty much you know, divested everything for the five years that I was running Joslin, I say, okay,
Scott Benner 24:03
Oh, alright, that's what we wanted the president to do, that he didn't do is that we were saying that that whole, like, you just sort of take yourself not to be political, but you.
John Brooks 24:11
Look, it's the right thing to do. I mean, you know, if we were doing some work, maybe some of the doctors at Joslin, which they were were doing different, you know, studies or, you know, clinical trials. Yeah, you could argue, well, I don't have anything to do with that. But it's appearances and it's really good governance. And frankly, you know, I think it's just having a good moral ethical compass. So, you know, was I going to influence results? No, but you never want to have even the suggestion of impropriety. And I just said, Look, this is the right thing to do. Right? That's excellent.
Scott Benner 24:45
Oh, that's very cool. So you're still you're still involved that and you're so you're an owner at this point still?
John Brooks 24:50
Well, I'm a shareholder share with you know, a small one. Other people yeah, there's
Scott Benner 24:55
you're saying somebody else is listening. This right now going? I have way more than john does.
Unknown Speaker 24:59
Yeah.
John Brooks 25:01
I'm sure every major, you know, you know, public equity fund out there, you know, mutual funds, but now I'm happy to, you know, be involved that in, you know, full disclosure, I have a stock holdings and other you know, diabetes companies because, you know, you know whether it's on the CGM side or it, you know, looking at pumps in and I work with, you know, a lot of young companies that are working on, you know, what I call the next generation solutions, whether it's new new insulins, whether it's a new type of CGM, there's some companies working on, you know, new pumps, the company's working on defeating the auto immune system, companies working on you know, better real time insulin type tration, and people with type two, so, about 80% of what I do, you know, these days is still, you know, helping, especially young companies, and I'm either doing it as the chairman of the board, board member, advisor, consultant, you know, trying to make sure that, you know, what I've learned over the years, and, you know, how can I help them turn themselves into a successful company that is going to further help people, you know, with type one or type two to, you know, live better, healthier, safer lives? That's cool.
Unknown Speaker 26:18
How old's your son now?
John Brooks 26:20
My son is going to actually turn 31. Next month, so just a few weeks away, he works for this company called livongo. I know Yeah, sure. heard of them. He was literally one of the very first people there. In fact, he was with the predecessor company called EOS health. So he's based out in Chicago has been with them, you know, I guess it's been eight years. And, you know, he manages their sales effort in the Midwest. So I guess he's had another, you know, I think, opportunity, he has type one. But, you know, he devotes a lot of his time to, you know, help lavon go get, you know, solutions for self insured employer employees who need help with diabetes, and now they're moving into hypertension, weight management behavior, et cetera, et cetera. And, you know, they went public, and now they're, you know, being acquired by teladoc. So, he's keeping busy, but he's pretty excited that he made a good career choice when he graduated from college, I have
Scott Benner 27:26
to ask you, I'm not sure where you're gonna go with this, but does he wear an army fine.
John Brooks 27:31
So he doesn't, you know, it's interesting,
Unknown Speaker 27:34
all this effort that you put into it.
John Brooks 27:37
But you know, at the end of the day, and I'm sure you might even know, with your daughter, you know, what, you know, it's their live, it's their decision. And, you know, and again, he, he's always been a fan. He's talked about it, but you know, just one of those things where, you know, I don't know why it just didn't fit his schedule, or didn't have the time. So at the end of the day, he may, but you know, today, he's not on it, but it's not a sign that he doesn't believe in, it's just, you
Scott Benner 28:07
know, no, I don't think that hey, listen, on the pod has been a sponsor of this podcast for since the beginning for many, many years. And I always tell people, the same thing, get a demo pod, try it for you, or it's not, it's you know, there are other insulin pumps, you could you could do MDI, you know, get an in pen, there's 1000 things you could do. Yeah,
John Brooks 28:28
the real, the real key is to, you know, use a use technology in a way that works for you. You know, and obviously, you know, whether it's a you know, CGM with a pump, and you know, the idea of this, I think people realize, you know, that, you know, all of a sudden, they're, their lives are better. They're, you know, they're in range. They don't have the glycaemic excursions and, you know, and it fits into their lifestyle. So I think that's really the key, we get up. You know, I do some work with the ADA. And, you know, we had a discussion recently with insolate. Just, you know, kind of getting to know each other up. Bob gubbay is the new chief medical officer, Chief Scientific Officer for the ADA, and he was on the call, I had hired him at Joslin, so he, he's a great person, but the whole idea is essentially just, you know, I think an appreciation that, you know, people that have been on MDI, you know, maybe just thought luck pumps are too complicated. They look like they're, you know, not going to work for me. And, you know, obviously, you know, I think once to your point, they try them. Also, they realize they're pretty straightforward. And, you know, and I think, you know, companies are sensitive to making sure that, you know, they're affordable and, you know, that they work for people. And again, I think the payers, you know, the insurance, I think, you know, understand that they're cost effective. I mean it wasn't too many years ago where, you know, you had to jump through hoops to justify Someone get a CGM or even a pump, you know, but, you know, the good news is the data is there and the values there and, you know, the world's, you know, continuing to evolve.
Scott Benner 30:10
What was the most difficult if there's one difficult part of getting the AMI pod to market? Was it the, the function of it and the mechanics of it? Or was it the FDA? Or is it insurance? Like, I guess?
John Brooks 30:26
It's a good question, you know, part of it, you know, I would say is just, you know, a disposable pump, you know, took a little while for people to get their heads around that I remember, we had some people saying, that's a stupidest idea I've ever heard of, I think the regulatory path, you know, we went through it, but I think, you know, I'm, you know, I spent years you know, kind of, uh, you know, working at Pfizer, you know, really a lot of device companies, you know, I do a lot of biotech and other things, but, you know, still know, the device base. But you know, my partner Duane knew that. So, you know, I think the key is, we weren't all that concerned about the regulatory, a big part of it was reimbursement. I mean, you know, you have to go kind of payer by payer across the country, you know, we kind of started in New England, and, you know, kept going west, to get payers to agree, you know, because it's a different approach. I mean, everybody else, you have this upfront investment for the pump, right. And then you have all the disposables. And in our case, you know, we were kind of turning that upside down, you know, it's really a subscription model effectively, and trying to get, you know, payers to understand that, how did it fit into their reimbursement, you know, even the federal government, you know, would say, you know, if you're on Medicare, you could only get, you know, one pump every four years, well, if you're getting a new pump every three days, and, you know, just things like that, I mean, sometimes the way the reimbursement was set up, but just, it didn't understand that, hey, this was a very different form factor, economic value proposition and, you know, you had to get people comfortable with and, and then they had to understand, you know, at the end of the day, you know, if you looked at it over four years, you know, versus the cost of a traditional pump, you know, they're pretty comparable, but, you know, when you're first starting off, you know, people there will, how does this work? And that's not the way we do it, and, you know, so that there was just a lot of, you know, pioneering and, you know, I think the other part of was just, you know, understanding the manufacturing, you know, despite the idea that we thought it would make sense to have this great lights out factory. You know, we realized that, you know, we needed a different solution, in fact, you know, ended up getting involved with Flextronics, you know, and, you know, leverage their expertise at high speed automation, and, you know, ended up setting up some, the supply chain, you know, generally in China, because, you know, we wanted to, you know, make sure our economics worked. And now, it's ironic, it's kind of coming full circle, back to the US, but so, you know, getting that manufacturing and getting the cost of goods sold was something that we always, you know, spend a lot of time on, because you don't, you know, you don't have a good business, if you're, you know, losing money on every shipment, but you've got to have the volumes, you have to have the, you know, sufficient economics to support, you know, getting the cost per unit down. And so that took some time.
Scott Benner 33:34
Who's gonna say, even understanding, hearing you talk about having to go state by state and explain to payers like, this is how it's going to work. And, yeah, I know, this isn't what you usually do. But this is this. I've had those conversations for my daughter, and back in the day, you'd have to get on the phone. Every time you reordered and say no, no, listen, listen, I know we just got a pump. That's not when then you'd have to re explain it to somebody was fascinating how many times I've done that.
John Brooks 34:00
Yeah, no, and you know, the if you think on the CGM side, I mean, you know, I remember in the early days, you know, payers reluctant to allow someone to have a CGM a reimburse them for it, you know, because if their numbers are in pretty good shape, you know, they say, well, you don't need a CGM. Or maybe you don't need a pump. And then the whole idea was, well, you almost had to have people deliberately, you know, mess up their diabetes management for 30 days to show that while you're not in good control, therefore you should get on I mean, if you think of the absurdity of that, yeah, but you know, that was part of it. And, you know, we used to have a lot of our great doctors that Jocelyn I mean, spending more time on the phone with insurers, you know, and even silly things like you know, why does someone with type one Why do you need to check your blood sugar's whether BGM you know, eight times a day what just do a two dads What are you doing? I mean, just absurdity.
Scott Benner 34:57
Ya know, the lack of understanding it permeate pretty much.
John Brooks 35:02
You know, type one versus type two. I mean, you know, a lot of people just still don't fully understand, you know that. Yeah, it's diabetes. But you know, it's a very different mechanism. It's not like if you have type one, avoid sugar, you're going to be great.
Scott Benner 35:16
It's I just was speaking with a person last night Whose child is more newly diagnosed. And this podcast, john, which you probably don't know anything about, I take great pride in it. It explains to people, among other things, how to use insulin, and my daughter is a one C with the dex comment on the pod is between five two and six, two for over six years. Now, she has a great diet restriction. She's doing terrific. I talked about what we do here, it seems to get to people in a way that they can understand it and replicate it for themselves. So I'm talking to this person, and she's like, I don't understand, why does my endocrinologist not understand? Like, why am I talking to you? And not her? And I said, I don't know. I don't I don't know what to tell you about that. But it just, it's what you it's what it made me think when you were talking through it, that most people would hear this and think, well, how could an insurance company not understand what diabetes is? or How could you know? And the answer is, because people don't, you know,
John Brooks 36:12
I mean, they, you know, and again, nothing against the people there. But, you know, anytime you bring something new or a different business model, different approach, you know, it doesn't kind of fit the traditional, you know, scheme, and you got to educate them, and you got to do the analysis, and, you know, uh, you know, they just tend to be a little bit change resistant, right?
Scott Benner 36:35
Yeah, you fall into something that you're comfortable with. And it works, whether you're a company or a person, and you stop being stop having reasons to wonder about other ways to do things. So exactly, you come along with this little pod, and you're like, Hey, listen, this is the way to go. And
John Brooks 36:49
that's like, what do you mean it after three days and throw it away? Like, why are you throwing it away? Right? That's designed that way. That's what it's for. Exactly.
Scott Benner 36:58
It really is. So if you if you can't say or you shouldn't, I'm not sure. But I've forever want to understand, while you know, you get your pot out, you fill it up it Prime's take off the needle cap, you put it on, and you say Go ahead, insert it, and then there's this clicking that is sometimes four times it clicks, sometimes it's five, sometimes it's six, and then, you know, blink of an eye, the candle is in, in my estimation, it's always been that something fires. A needle that's wrapped in a candle and the needle comes out leaves the candle behind, but is it not functionally firing? Is it tension? How does it do? Are you can you tell me how it does that?
John Brooks 37:40
Yeah, you know, I don't know what it does today, it's probably different than it was. But, uh, but I think your points accurate. And the whole idea was to get rid of needle phobia, to be able to have a very simple way to your point to deploy a Candela, you know, with a needle that would place it properly, and then, you know, disengage itself. So all you had was the candle lit to deliver the insulin. So yeah, I mean, I mean, I don't want to speculate, because I'm not sure how it works today. You know, the idea was to basically, you know, deliver it in a way that, you know, it would get into the skin at the right level, you know, and, you know, not caused any bruising or hypertrophy. I mean, there was a lot of work that went into the, you know, the needle design and the, in the shape and the insertion, pressure force, whatever you want to call it. So, but yeah, I'm probably, you know, it's been a while since I've looked inside one, it prompts me, I probably have an old one around here, I should look into
Scott Benner 38:38
I'm now wondering about the the day in the office where somebody was, like, I put it on me and push the button, and let's see what happens. That's how many how many people do you think in total? Were there in the beginning?
John Brooks 38:52
Well, in the very beginning, you know, there were two of us on an airplane. Right. But then, you know, we ended up as I said, we we had a team, we were up in the Cummings facility in Beverly mass, you know, after we have put our partners that put some seed money in, you know, we hired a guy that, you know, really brilliant in terms of, you know, just looking at the entire intellectual property landscape, you know, were there any other patents? Was anyone else doing anything? You know, and how would we, you know, think about creating the product? How would we think about, you know, what type of plastic what type of, you know, materials, you know, we thought a lot about, as I said, quote, unquote, the pumping mechanism, we thought a lot about the canula and the insertion mechanism, and, you know, what the battery life is and how to make sure that, you know, those accuracies, so in the early days, you know, was a bunch of really bright people, probably more engineering, you know, you know, folks had new devices, folks and new IP folks that understood we had to be able to make this thing very cost effectively and You know, you're kind of designing it and building it on the fly. And, and then, you know, we reached the point where, you know, I think we felt we had a good plan, we had a good business plan, we hired a fellow as our CFO who eventually became the CEO Dwayne to Cisco. And then, you know, we, as the company advanced, you know, we brought more money in, we brought in other venture partners, our our team continued to support it. And then, you know, we ended up getting, you know, new space, we left Beverly in, you know, we started to hire more, you know, a larger team, you know, in terms of, you know, recognizing that, you know, what do you need to have in, in, in addition, engineering, you know, you got to have people that are, you know, working on the supply chain, you got to have people that are working on, you know, understanding the whole regulatory process quality process, you know, starting to think about reimbursement starting to think about, you know, packaging. So, you know, you start building a team, and, you know, that took place over you know, a number of years, we go from kind of a, an idea that we had to you know, starting to think about, you know, what it should look like and again, just simple things, like, you know, what type of plastic and what type of plastic you're going to mold and what's the shape? And how much stuff can you fit into it and still have it work, but not be too big. And, you know, just lots of, you know, iterations that you know, you get a team and then you start getting people thinking about, how do you market it? What are we going to call it all that stuff, right? You know, in the early days, we used to call the op,
Scott Benner 41:42
it must be crazy to be a startup in a space that is, like, you know, pharma and device manufacturers, like bigger companies like Indy, you're sort of just these, your two guys coming off a plane and putting together things, by the way, the company still has a really good vibe, you know, throughout it, you can tell what the, as you're explaining what the roots of it are, it doesn't surprise me. Because I think it's grown in that direction.
John Brooks 42:07
And it's pretty neat. I mean, every now and then, in fact, at the last Ada meeting, not the virtual one, but, you know, My son was with me, and, you know, we were kind of walking the floor and, you know, went by the booths. And, you know, it's kind of one of those funny things where, you know, a couple of people start putting the dots together, wait a minute, you're the father, You're the son, I mean, yeah, you know, all sudden, they realized that, you know, we were kind of the, you know, that the, you know, My son was the inspiration and, you know, I was one of the co founders, every I kind of needed it, and again, you know, still having that, you know, you could call, you know, kind of that entrepreneurial spirit and, you know, really thinking, you know, what, I always like to think of disruptive innovation. And, and again, you know, I spent, especially back in those days, you know, most of my career was in the device world, I, you know, had ran a couple of businesses for Pfizer, and one of them was actually a company that had infusion pumps, and, you know, so, you know, we certainly knew a lot about, you know, delivering, you know, whether it's insulin or other drugs knew a lot about, you know, device manufacturing, regulatory, you know, so, anyhow, you leverage all that. And, you know, at the end of the day, you hire bright, smart, capable people who, frankly, thrive in a small company environment. I mean, you know, in a small company, I mean, you know, forget about your title, everybody's working hard. Everybody's working late, everyone has a passion for, you know, doing what we're doing, because we're going to improve the lives of people with diabetes really have honestly, hey,
Scott Benner 43:42
listen, is this to ham fisted? Or maybe this happens all the time. But do people call you the pod father? I mean, I've never heard anyone call me that. Well, then I'm doing it right now. Because that seems like an obvious pun. I mean, honestly, and, and, and what a, what a, what a, what an absolute parenting story, it is to like, you're like, let me do this thing for you. And you do it and you build this entire thing for it at the end, like, that's nice, but I'm not gonna use
John Brooks 44:12
it. And again, you know, he may very well you know, decide at some point he wants to do it. Yeah. And again, you know, he's a, he's doing great things in the world of, you know, helping employers and payers and all help their patients with diabetes. And now hypertension, weight management, as I said, it's really nice soon, you know, to be, you know, part of Tella Doc, which takes it even to a bigger stage.
Scott Benner 44:37
I'm having. I honestly, the experience that we've had with my daughter, doing telemedicine over the last number of months, I think has been an incredible improvement over what we had been doing prior to that, honestly, yes,
John Brooks 44:50
I agree. I mean, if you think of it, I mean, you know, and I did some piloting a Jocelyn. I mean, this is many years ago, and, you know, it was hard to get Add, you know, great clinicians, but you know, they were just used to, you know, meeting people in their, in their office, if you think of diabetes, I mean, it's the best, you know, way to treat people, because what do you do physically, you don't really need to do anything. There's no procedures, you're, you know, helping people and the diabetes nurse educators and the dietitians. And so but, you know, before we had to do it with COVID, you know, it's just people are convinced that you have to do it that way, right? Now. And in some ways, you know, it was just the, you know, people were resigned to the fact that I'm going to spend an hour to drive in the Boston, I got to spend 4050 bucks to park, I'm going to sit in the waiting room and wait, because this is a, you know, global leader and all the clinicians or bright and busy and, you know, that's the price you get to pay. And, you know, now if you said, hey, let's go back to that, you know, people there Nope, not gonna do it.
Scott Benner 45:57
I don't think that anything's been more gratifying in the last three months and sending an email to somebody and saying, hey, my daughter has hypothyroidism, too. And saying, Hey, I think Arden's a little hyper right now. And she fat and she emails back a script, we get a blood drawn, the next day, they move the tiersen down a level, and it's it's done in 24 hours almost. And before, like you said, get an appointment come in, take a day off from school, like all this other stuff to maybe get an answer in a month, if you're lucky. Really,
John Brooks 46:26
it's a it's a change. And again, I think it says we're saying I mean, I think diabetes lends itself to you know, having smart devices, analytics, AI and the ability to basically let the care team, you know, monitor from afar, how people are doing and make sure they get the right coaching, the right encouragement, you know, but but the idea is essentially, make the lives of people with diabetes easier, and take the burden off of them and, you know, give them an opportunity to basically live a, you know, healthy life and, you know, avoid, you know, the, you know, what, what used to happen, you know, was people developing complications, and, you know, not that they don't exist, but you know, I think we're doing a much better job of, you know, making sure we get ahead of the curve and not waiting for someone to have, you know, eye problems or kidney problems or vascular problems. I mean, the whole idea is, you know, a keep people in range and keep the excursions in, you know, don't let things get to the point where, you know, the the problems start arising.
Scott Benner 47:34
Yeah, you have to be proactive for certain I have two last questions for I thought I was only gonna have one, but now I have to because of your time at Jocelyn, how do you? Or do is it obvious to somebody like you that there's an issue with clinicians not understanding diabetes, as well as the people who have diabetes? And how do you speed up their understanding so that they can help newer people?
John Brooks 47:58
Yeah, no, it's it's a great question. And look, you know, whether it's Jocelyn or other place, Sherman just very talented individuals. But, you know, you know, especially a place like Joslin, you know, part of the Harvard complex, I mean, you know, academic medicine, you know, people are brilliant, but you know, there tends to be a lot of clinical inertia, you know, they want to see data, they want to see papers, they want to see peer reviewed journal articles before they fully get on board. And the other part of it is, you know, I think, you know, they're busy people. And, and, you know, as much as they're going to keep up with all the new developments, all the new information, you know, it just, it takes a little while and, you know, but but I think today, you know, with a lot of, you know, capabilities built into the electronic health records, you know, there's ways for, you know, clinicians to be able to, you know, get a better handle on how this individual is doing, what are the other potential comorbidities or factors that are going on? And then, you know, which is the right approach? And, you know, if you have type one, you know, what type of devices and, you know, do I still think about putting you on some sort of, you know, Sdlt, to inhibitor, I mean, so, but, but, but the issue is, I think it was just, you know, busy people and, you know, just trying to deal with all the stuff they had to deal with, and then after they get done seeing patients, make sure they put all of their information into the, you know, billing systems, so the bills could go out on time. And so, you know, I think it was just easy for people to kind of get into a, you know, I don't have time to think I just got to react. And so, you know, now I think it's easier with, you know, as we said, with kind of the whole virtual care, you know, I think it's just easier to be able to focus on for an individual, you know, what, what is it that we should talk about during this time we haven't, you know, that the doctors don't have to spend time kind of reviewing or trying to make sense on the fly out of CGM plots, and, you know, now that the information is there, it's more a question of helping, you know, determined for that person with diabetes, you know, what's the best way to, you know, help you even further improve? And, you know, to be there, you know, if people are still struggling, you know, because it's, you know, there's still challenges on the board of the college diabetes network Chairman there, and, you know, we spend a lot of time if you think of it, college students, you know, dealing with diabetes in this environment, you know, virtual hybrid classes, and, you know, the whole, you know, sided diabetes around depression, and, you know, behavioral health and also, you know, so in some ways, you know, life is getting easier, but life is getting more complicated, right, right
Scott Benner 50:48
now, it's interesting, I just have, I have such a personal experience over time, where it's gonna sound crazy, but I could sit down with you in an hour and explain diabetes to in a way where you would just understand it. And you'd, you'd be able to put it into practice, I've practiced for a decade or more writing about it and talking about it and, and just when you see someone struggling, who has great care, what really is considered great care. And then they come along, I mean, think about it, really Jimin, they come on and listen to our podcast, and then all of a sudden, they're like, Oh, I understand now. And then they're often there. Okay. It feels like there's a disconnect somewhere in between that, you know, what I mean?
John Brooks 51:26
Sometimes, you know, maybe, maybe the key is, you know, you know, you got to make sure you're connecting with people at their level, maybe some people I mean, you know, especially in type two, I mean, a lot of people are told by their, maybe it's your primary care doctor. And again, I'm not trying to malign anyone, but you have diabetes, and here's what you need to do. And I'm going to put you on Metformin. Well, you know, at the end of the day, I mean, I used to hear from many people, well, I don't really know what it means when I have diabetes. I mean, they don't understand things. And maybe they say, well, I'll avoid sugar. But you know, I can have pasta rice, that's healthy, right? I mean, no understanding, you know, kind of how our bodies work. I mean, when I was a kid, you know, many, many years ago, you know, we actually had something in school called nutrition class, and health classes, you actually had some idea how our bodies work, I don't think we're teaching that to kids anymore. So the idea is a lot of people just, even though if you're in it, it's kind of like, Well, why don't you understand it? Some people just don't fully understand like, Well, you know, what do you mean, my pancreas isn't gonna produce insulin or, you know, it's not producing enough insulin or, you know, I'm watching my blood sugar's but, you know, I'm in competitive sports, or I'm stressed out or, you know, when people start realizing there's all these other factors that affect your your glucose, I mean, you can eat the same meal every day, do the same thing. But if you're stressed out one day, or you didn't sleep well, or something, you know, you're going to have different results. A lot of people don't fully appreciate. Well, why is that?
Scott Benner 52:57
Yeah, I think that when, when I start talking to people, privately, which I do sometimes, just as I don't know, I think it makes me better at being on the podcast to have one on one conversations with people that aren't recorded sometimes. But when I start off by 10, I'm looking at to get your basal insulin, right, because nothing's gonna work. If that's not right. And then you really need to Pre-Bolus to understand how your insulin works. When I get to the third thing and say, You need to understand the glycemic load and the glycemic index foods, I don't think that's what they think they're going to hear next. And when you tell somebody that, you know, 10 carbs of one food in 10 carbs or another food are going to impact you differently. I completely agree with you, it fries their mind. They're like, no, they told me that not the
John Brooks 53:36
cause. And, you know, and again, we were learning a lot about, you know, again, you know, what else is affecting, you know, gastric emptying, you know, which foods tend to get into the bloodstream faster. I mean, again, there's a lot of complexity that, you know, not that we want to make it even more confusing for people. But the hope is that, you know, over time, you know, devices are going to start incorporating in, if you think of all the wearables, people are starting to pick up on heart rate variability, they're starting to pick up on sleep, and at some point in time, maybe those additional inputs, you know, might further cause the algorithms to be even smarter. Yeah. So all of a sudden, you know, we're having a better way to help people with diabetes, you know, understand that, yep. Blood Sugar is fine. But that's not the only ingredient that's kind of driving, you know, what's going on.
Scott Benner 54:26
Yeah, maybe one day the, the pump will know that, hey, I had pizza. So the cheese is slowing down the digestion. But now the cheese is gone. And everything's going through me quicker and not impacting me the same.
John Brooks 54:37
Yeah. And again, a lot of pumps are going to say, you know, hey, I remember the last time you had insulin and here's, here's what happened. And you know, instead of you having to figure out a square wave bolus, whatever, you know, the system is going to basically say, Yeah, I remember that. You know, let me make sure that I'm adjusting your insulin or if you're an athlete, I remember you know, when my son Played high school sports or you know, we've had a lot of kids that Jocelyn, you know, playing competitive sports and you know, the the issue is, you know, your blood sugar's you know, you may be fine during the game and then eight hours after game time you're crashing and you know, understand why why do that's, you know how do you get muscles reload? So anyhow, it's complicated but we're chipping away at, you know, getting it there and maybe in the background we've got people working on, you know, either, you know, beta cell regeneration protecting the immune system, I mean, you know, there's lots of other good things going on that I'm on top of as well. So maybe someday, we'll make all this moot.
Scott Benner 55:39
That's my last question is, what do you see coming that is exciting to you, because I just had a Dr. Jeffrey Millman on the other day from Wash U. And he was talking about stem cells and how they're getting cells. Now the sense glucose make insulin not seen as you're bound by your body as a farm. You know, that's, it's all amazing. Like, yeah, no,
John Brooks 55:59
it is, but you know, and it's happening, you know, in different parts of the world, you know, that there's people working on, you know, defeating the autoimmune process people working on, you know, basically protecting the beta cells, there are people working on regenerating the beta cells or people working on in capitalization, there are people working on, you know, new treatments. I mean, you look at some of the stuff, you know, the nice salsman, you know, at mgh with ECG, and you know, so lots of advancements, people are making headway, you know, you look at, you know, semma, which was a Doug Melton company, now part of vertex and all sudden, you get a very big pharmaceutical company working on, you know, kind of, you know, beta cell and capitalization, you know, you get other kinds of companies that are in that space. And little by little, you know, we're kind of cracking, you know, wider regulatories T cells go awry. And, you know, how do you do that? So, yeah, I mean, we could talk for another couple hours on, on, things that I see. And, you know, I'm usually involved because, you know, I just get motivated by that. And again, companies sometimes seek me out, because they know, I know enough to be dangerous, and maybe I can help them either get financed or advanced, right,
Scott Benner 57:15
understand how to get through the whole process. And that's got to be such a huge part of it. It's just having somebody with you, that can help guide you around the pitfalls, right. That's got to be
John Brooks 57:24
Yeah, I mean, you know, I've been, you know, doing this for a while, and, you know, seeing the good bad, the ugly, but, you know, the hope is that, you know, at the end of the day, you know, a lot of these companies to challenges, you know, getting the financing and having a value proposition that's compelling to investors, and, you know, making sure that they thought through the timelines around, you know, regulatory issues, quality issues, reimbursement issues. And in today's day and age, it's the old Wayne Gretzky line. You know, you don't want to develop something, you know, to solve today's problem. It's, where's that puck gonna be five years from now to
Scott Benner 58:01
skate? Where the puck rolling, right?
John Brooks 58:03
Yeah, where's that competitive landscape gonna be? Who else is out there? And how to make sure that you're, you know, kind of leapfrogging the competition, not just incrementally saying, Hey, I got a better mousetrap. And, you know, if you're already kind of behind the times, so I tell people when they're using their insulin, that everything you do now is for later, and everything that is happening now is from something that you did in the past. And I think that thinking like that, in general is a great idea. Well,
Scott Benner 58:29
john, thank you. I don't want to take up any more your time, but I do want to leave you with something. Because I, I don't know that I fully wrap my head around this sentiment that gets given to me a lot until you were talking about your son. But people thank me, my daughter does not come on this podcast, right. She's 16. She doesn't care about a podcast. And and people tell me all the time, how grateful they are that her situation led to their success. And now I'm realizing as I'm sitting here is that, that this podcast really is born out of my concern for my daughter, and she's wearing an insulin pump that was born out of your concern for your son. So it's very kind of chilling, honestly.
John Brooks 59:09
Well, I would, I'm sure he'd be interested. So at some point in time, you want to do a podcast with my son, I think you're gonna find you know, he's even sharper than I am. So I'm gonna do
Scott Benner 59:19
that. Yeah, No, I haven't. Yeah.
John Brooks 59:22
Yeah. I mean, he, I mean, if you think of it, I mean, you know, he, he's, you know, understands this disease, because he Elizabeth every day, and, you know, working for a company that you know, now is extremely successful. And, you know, what had some interesting experiences along the ways. So, you know, so yeah, you might want to get him on a podcast, I think you'd find it pretty entertaining. Well, it'll be easier for me to find him than it was for me to find you. Because, you know, you just would go around saying to people, like, you
Scott Benner 59:48
know, the guy that made the pot What's his name? And said, finally, somebody one of my friends had on the pods like, it's john. And I was like, Oh, is that him? And she goes, Yeah, I said, I think I know someone at t Wendy exchange. I'll be fine. Cuz like, I'll figure it out, which is another great organization that you you sit on the board of Is that right?
John Brooks 1:00:05
Yeah, yep. T Wendy exchange college diabetes network. You know, so you know, places diabetes related. You know, I'd like to think I can be helpful in some way.
Scott Benner 1:00:16
Well, I'll know I'm doing well, when you want to invest in me. Chad, thanks so very much. I really appreciate it. My pleasure. All right. Take care. Have a good day here.
Unknown Speaker 1:00:24
Yep. Bye. Bye.
Scott Benner 1:00:27
Hey, huge thanks to the pod father, john Brooks. Can you imagine it if people by the way, if you know john, start calling in the pod father, I'd like to see that pick up if you guys can make that happen. Thank you. Anyway, john, thanks so much for coming on the show. And for sharing your amazing and very unique experience dreaming up an insulin pump. Thanks also to the T one D exchange T one d exchange.org. forward slash juice box. Join that registry today support Diabetes Research, support the podcast and touched by type one touched by type one.org. Thank you to those sponsors. And of course, welcome g Vogue glucagon to the family of sponsors here at the Juicebox Podcast. Learn more about that pre mixed prefilled, glucagon or the hypo pen at GE Vogue glucagon.com. forward slash juice box. There are links in your show notes. And at Juicebox podcast.com. To all of the wonderful And may I say delightful sponsors of the Juicebox Podcast. Check them out if you would. Thank you. Hey, last thing, the Facebook page for the podcast is blowing up. I mean, that is what the kids would say. Right? It's it's blown up. Be like you know what they said about their phones and stuff. I'm I'm very old. I don't know what people say. But that's not the point is on Facebook. There's a public group. It's called bold with insulin. And there's a private group Juicebox Podcast, type one diabetes, that private group up to 6000 users just about, huh? Is that bananas, 6000 people and they're just helping each other out. It's amazing. It's the kindest place you'll ever find on Facebook hand to wherever you want to hold your hand up to when you're swearing on things. I mean, it I've never seen a nicer, kinder, more thoughtful, less egotistical, more lovely and delightful group of people helping each other with Type One Diabetes than I have right there in that group. I am as proud of how that group functions, as I am about anything else connected to this podcast. It's really, it's quite something. And the public group has like 10,000 people following it. I'm really stunned. I am not really a Facebook person, but turned out to be quite a little resource and I'm super happy about it. Alright, I hope you have a great day. I hope you've enjoyed this conversation with john learning more about how the Omni pod came to be. I really did and what else feels like I have nothing left to say. So that is that
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
# 385 Gvoke HypoPen
Gvoke is a premixed, prefilled, premeasured liquid glucagon that now comes in a HypoPen!
Ken Johnson is Senior Vice President, Clinical Development, Regulatory, Quality Assurance & Medical Affairs at Xeris. Ken is here to talk about the Gvoke HypoPen. Xeris makes Gvoke. The premixed, prefilled, premeasured liquid glucagon for treatment of very low blood sugar in adults and kids with type 1 diabetes ages two and above.
Jenny Smith is also here to help me answer questions about glucagon.
Learn more about Gvoke here
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Alexa - Google Play/Android - iHeart Radio - Radio Public or their favorite podcast app.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott (1s): This episode of the Juicebox podcast is brought to you by GE Voke. The world's only liquid stable Glucagon G Volk is available in our, a prefilled syringe and in an incredibly convenient to carry it an easy to use HypoPen. As a matter of fact, I have a trainer of the HypoPen right here. Let me show you how easy does to use cap comes off. I find some skin press down
1 (28s): And it's done that.
Scott (30s): Yeah. Easy to administer glucagon. It's the easiest thing I've ever seen when it comes to Glucagon hands down. We're going to talk all about it today. How the G vote Glucagon came to be or what it is, and this brand new HypoPen, which is incredibly convenient to carry. And as you just heard, super simple to administer, anybody could do this in my opinion, before I start the show, let me say thank you. Because every question and this episode came directly from listeners to the podcast. So I really appreciate the effort and the thought that you guys put into those questions. And I hope you get your answers. I think you're going to today's episode is going to be a little different than most I'm interviewing to people today about Jeeva Glucagon first.
Scott (1m 16s): I'm not even first. Now here's the surprise. Let me just give you the surprise. Jenny is on this episode. Jenny Smith is here and I'm also speaking with Ken Johnson. Now Ken is a senior vice president of Clinical. Wow. This is quite a title at here. Ken Senior vice president Clinical Development Regulatory Quality Assurance that? Medical Affairs at Xeris pharmaceutical's Xeris makes Gvoke. Ken's got to answer all of your questions and Jenny is going to answer something to me.
1 (1m 45s): You guys,
Scott (1m 46s): You love Jenny. I love Johnny. How can we not love Jenny that's who else are you going to love? Ken Ken who buy the way has the secret talent. The man could play the piano, but not have to wait all the way to the end, to find out about that. Please remember that Nothing you hear on the Juicebox Podcast should be considered advice Medical or otherwise always consult a physician before making any changes to your health care plan or becoming Bold with Insulin
Scott (2m 38s): And there are two ways that you can request it through your doctor, either online or in person. If you have commercial insurance, you can request a prescription for Gvoke HypoPen right from the comfort of your home and have it delivered to your door fulfilled through PillPack by Amazon pharmacy. Just go to
Scott (3m 19s): We're going to start with Jenny Smith and then do a little Ken and then back too, a little Jenn. And Ken you got to get a nice rhythm going a little Jenny a little Ken is going to go just like that. I think you're going to enjoy it at the risk of repeating myself, because I say it in the episode, this is a leap for people who use Insulin making Glucagon liquid stable. It just This. If you don't understand why listen closely Jenny I already talked to Ken Johnson from Xeris pharmaceuticals about the Gvoke Glucagon and he's gonna be on the Show.
Scott (4m 7s): And just a minute, we talked a little bit just about what they were, you know, what they're trying to accomplish. I told him if the end of our conversation, that I'm incredibly excited about that company, like the ability to stabilize Glucagon in a liquid form, I think has other far reaching possibilities that I'm really excited about. But while I was talking to him, I got a it's a it's a, and can you tell if you can see this or not, but it's called their HypoPen and this is just a trainer, so it's not, it's not real, but you just pop off the cap and go like this and that's it. And it's over yet. And I was like, huh, well, that seems simple.
Scott (4m 47s): And I'm going to get one of those for Arden
Jenny Smith, CDE (4m 50s): Beyond simple. It's not scary
Scott (4m 52s): Exactly. Because you know, till this point in my life with type one, diabetes, glucagon has been a little bit of an, a, like a science experiment, but it was going to be an in a pressure situation. It's almost like someone saying to you here, do this while your driving a car, and there's a bear in the backseat, you know, you kind of felt like that to me the whole time. And, and they have their pre, they have their premixed syringes for emergencies to, which is just, you know, it's you just, it's in and push and you're done right yet. But, but still, and I'm, I'm going to ask you first, before I tell you what we do.
Scott (5m 35s): Do you carry Glucagon with you when you leave the house?
Jenny Smith, CDE (5m 40s): I don't carry Glucagon with me. If I'm just leaving the house for like going to the grocery store or going across the street to the park. No, don't I absolutely don't when we leave to go on even like a short weekend, two are in-laws or I go on, you know, to speak somewhere and whatnot. Yes. I, it with me now in that same case, though, if I'm carrying it with me in my pocket at a conference, somebody got to know what's in my pocket.
Scott (6m 9s): There's a lady on the floor. Hey, there's a science kit in your pants. What do you think? That's? What should we do? Where in the same boat, we don't carry it around like that either. If we're going to go too far away, or if it's going to be, if you're going to do at the beach or a trip, it comes with us. So here's my question. Would you carry this with you?
Jenny Smith, CDE (6m 28s): I would, because one, that's really easy to keep in my purse. And I mean, I've also, you know, knowing that I've got a son who'll be in second grade or something like this are easier to carry, I think, and from the standpoint of even teaching him visibly, there's no needle. I can easily say, Hey, pull this cap off, you know, stick it in my thigh, push it until it turns red and it clicks and it's done. I mean, that's it.
Scott (6m 58s): And it has these audio responses. I don't know if you can here the sec. So there's too, there's the push. And then the second one tells you your done. And I was like, huh, this I would put in Arden's bag. Like I really would. It's not going to scare somebody. And not only that, but if somebody opened this up a person who had no idea what they were doing, it's going to, you know, the packaging tells you what to do. And there's nothing about what I said to Ken when I was talking to him was I took this out of the mail, this trainer, and I handed it to my wife. And I said, I don't wanna tell you anything about it. See if you can make it work. And she did it right away, but it didn't take any like thought to do it's easy.
Ken Johnson (7m 39s): Hey Scott, this is Ken Johnson I'm with zeros pharmaceuticals. And I have a number of responsibilities that the company, including how we develop our drugs in the clinic and get them approved by the FDA. We also have medical team that supports ah, people with diabetes. And there are clinicians in the marketplace. And I also have a quality assurance team that makes sure that the drug's as we make them package them and ship them to pharmacy's and ultimately people and their homes meet the higher quality standards required for a prescription product. So all of those combined have been my responsibility at Xeris pharmaceuticals. For the past three years, I've been in this type of role for pharmaceutical development for a better part of 25 years.
Ken Johnson (8m 25s): I started out, I was trained as a pharmacist. I did research at the university of Colorado, whereas also involved in clinical research as a result of that clinical research. And I found my way into the pharmaceutical industry sector and had been there ever since. So that's a little bit about me. I'm I'm in Chicago where our headquarters are based and really happy to be with you today.
Scott (8m 47s): Thank you very much for doing this. I have a question about how you pull a team together for something like this. Does Paul know of you and com for you, or how does that work? Like how do you end up at Xeris?
Ken Johnson (9m 1s): Great question. So Polytech, our CEO, as someone who I met at the early part of my career. So 20 plus years ago, we were at a company based in Chicago called Searle pharmaceuticals. Paul was in charge of a number of commercial activities there and ultimately taking over some of the regional activities around the world, ah, for a number of our products. And I was his medical support. So a, you know, these things start early and have sort of an indelible effect. If these partnerships work and these collaborations work, you sort of maintain these relationships throughout your professional arc. We haven't always worked together, but oftentimes we'd been together out a couple other companies since that time. And most recently is he took the home at Cirrus who wanted to bring it together.
Ken Johnson (9m 44s): A group of folks that you felt could take us to the next level, get Gvoke HypoPen to market. And with that, he found me as well, a few others, we had this collective past together. So it's a little bit analogous to getting the band back together again. And we've, we've done that. And because of our past a familiarity success together, a what I think is an ease of collaboration, we do enjoy working together and I'm sure I'll do it again someday. Yeah.
Scott (10m 13s): How do you feel like The from the starting point to where you guys are right now, do you feel like that was on schedule went quicker than you anticipated? How much of that has to do with the, the, the, the, you know, the G Voke itself and how well it does, what it's, you know, what you're trying to, what you're trying to do.
Ken Johnson (10m 34s): Yeah. I think we encountered a situation where things were a little bit stalled or, or there's a few things that we had to take heat of that had been discovered before we arrived to make sure that we had, you know, a product that could meet all of the standards of the FDA. You could pass all the Clinical assessments. And so it really good foundation Scott, but it needed them and sort of to be rebooted to use that term it, and that meant conducting additional clinical studies further characterizing the product, making sure that we could put it into a prefilled syringe that's RPFs configuration or the HypoPen in the auto injector that was just released earlier this month. Right.
Ken Johnson (11m 15s): So that whole process of building, making testing, and then releasing brought together the team that you see today, you know, in fairness, there were about 12, 15 people at zero S when Paul took over and, you know, it's taken a lot of resources, people energy now in 200 plus employees later, you know, were on market with an approved product.
Scott (11m 40s): And for me to be sitting here holding this, this trainer pen, I guess it's a, it's a long time to get this into, get to this form and make sure it does what it says. So I think I want to understand what does it do because you've obviously come into a space where everyone has that red box and they genuinely think of it as something, you know, that they just have. They don't think much about it. I've been in that situation. My whole life. I get my daughter supplies, my daughter's supplies show up. They're there. I watch it until the expiration date and then I throw it away and I get another one. And I don't know that it's something that many people think about other than I know in the case of an emergency, you know, I've got this liquid in this powder and the syringe, and I'm supposed to mix them together and redraw them and use them.
Scott (12m 28s): And here's how, and ya know, and that kind of thing. And I have to train my school nurse to do it and, you know, My and her, grandma's got to know. So when she comes over, that's, that's, that's the narrative around that my whole life and for, for many, many people. So how do you improve on what's been going on for so long? Like what makes you feel like this is a great business and we should be doing that?
Ken Johnson (12m 52s): Well, I think, you know, just listening to your story and kind of the anxiety and complications that come with administering Glucagon for many, many years now, you know, going on in several decades of having the same configuration, it is a important pancreatic hormone Glucagon has very well known affects in terms of its ability to raise blood sugar. I think, you know, most days we're concerned about lowering blood sugar and insulin is critical, but, you know, think of this as the, the, the break where the accelerator, the, no, that the challenge is always been, it's a powder that requires reconstitution or, or, or put into a solution immediately at a time of use.
Ken Johnson (13m 37s): You can't do it early because it starts to break down very quickly. Most of the potency has lost or within 24 hours after mixing the powder for all these decades, that red box that you describe has been the single and only configuration available to people with diabetes are folks who would experience very low blood sugar. So our chief scientific officer took that on as a mission, you know, had his own personal experience and people in his life who said, you know, is it possible to overcome all those complicating, a multistep requirements of the lateralized Poudre in that vile? And he said, yeah, I think I can fix that. So it was his mission to make it a liquid, ready to use room, temperature, stable product, and to do that, we had to overcome the limitations of water and water is what you would use in the traditional kids to make it as a solution.
Ken Johnson (14m 29s): So we've taken water and replaced it with other a well known a solutions. Ours is called
Ken Johnson (15m 24s): And so you have basically a, a built in system to raise your blood glucose. And as such, we, you know, we wanted to just make the process of administering very approachable, very intuitive and not intimidating. And so we think we've accomplished that, but that was all only facilitated once we had a liquid version.
Scott (15m 44s): All right. After someone uses Gvoke what happens after is, are there side effects or are there things that happen afterwards? Am I going to feel nauseous? Do I have to go to the hospital? That's also, what's your dog's name, Bailey like that?
Ken Johnson (16m 0s): The question is, so I guess, I guess we'll have to give her a credit today. So a couple of things, I mean, you know, the effect that you do want is to raise a blood glucose, and that happens very quickly as we start to see changes in the blood glucose concentration within the first five minutes of administering the product is raised to what we consider a safe level of blood glucose very quickly on average, about 14, 15 minutes. And then the duration of action is probably about 90 minutes or so. So you have this ability to sort of bring yourself back up and then have it come back down, right? So it's a, it's a temporary fix two. What was a scary as hell? What can happen?
Ken Johnson (16m 40s): Glucagon has some other effects has some effects directly on the gastrointestinal tract. And so it at about 30% of the subjects that are trials has some nausea and about 10% handsome vomiting. So those are 10 or 15%, and those are kind of the hallmark features of what Glucagon does not matter what too, to anyone that sensitive to those GI side effects, importantly, they are transient. They are mild 80% of the people in our study and characterize them as mild. They went away and in our case, no one actually stopped being in our study because they had that, that known side effect that you would see that Scott with the old movie got, and you would see it with our Glucagon a you'll see it with future Glucagon so that we haven't mitigated.
Ken Johnson (17m 30s): It's probably dose-related. I think, you know, there will be a Day I hope someday where if we, you know, use different doses for different purposes, that we can mitigate some of that nausea, vomiting, but for the rescue one milligram setting of use your gonna have, in some cases, nausea and vomiting, then those side effects are
Scott (17m 50s): Side effects of Glucagon do not have a specific brand. It's just what happens during the process of bringing that low blood sugar up so quickly through Glucagon.
Ken Johnson (18m 0s): Yeah. And it may not even be read to get your rights. That's, that's the correct way to describe it in event, not even be related to the blood glucose, going back up as much as it is. There is a known, in fact that Glucagon to slow down the action of your GI tract so much. So that is completely different from what we're talking about today, but a radiologist will actually use this drug to stop someone's GI tract from moving, if they need to do procedures and other things. So now this is one of those situations where a bad thing for some person is a good thing for another, but it is important to let people know that there is some mild nausea in about 30% of people who use it for, for rescue.
Scott (18m 41s): Can you help me understand the different ways that I can administer as you vote when, you know, when you guys first came out and I became aware of You, my daughter switched too it, and she has the, the prefilled syringe, but now I'm holding. Like I said, This this dummy pen. That to me feels like I'm like what people would consider an epi pen and to be, I, I, I just push it down on my leg and hold it there for a second and, or a couple of seconds in, and I pulled away. Why do you have different versions? And can you tell me the difference between them?
Ken Johnson (19m 16s): Sure. The Glucagon it's the same for both a Gvoke PFS are people terrains in G Voke, HypoPen in the auto injector, you're holding a, in your hand. And so there's no difference. And that the active ingredient, the solution, the concentration is identical. It was a simpler and more straightforward manufacturing process to come to market with the prefilled syringe. It's less mechanical requirements because you, as a person, are the person helping you is actually going to do the injection much like you would self-inject or Jeff Insulin. Right? So it's a small subcutaneous injection, the necessary requirements to then put that into a device that fires itself, the auto injector, umm, it's more complicated, more engineering.
Ken Johnson (20m 7s): And we wanted to make sure we had sufficient quantity. So we come to market like we did the Smith and not having a sense of shortages or, or, or running out to be able to supply to market adequately. So, umm, there's a really, really high specification for performance of that auto injector because you're no longer responsible for pressing the plunger and the mechanics inside the auto injector. Our and so the FDA has carefully scrutinized the performance of this device and it has to work 99.99, 9% of the time. So that's a manufacturing spec and it came out of the experience that we've all had with epinephrin and HypoPen we want to make darn sure that if someone's going to pull that red cap off and press that yellow plunger, that if a fire's and so that took us a little more time.
Ken Johnson (20m 57s): Both were approved last September and in 2019, we could bring a prefilled syringe to market immediately and then to deal with all the issues that I just laid out. We just need a little more time and happy to release that now in July,
Scott (21m 12s): That's exciting. It really, it really is terrific. As I'm sitting here holding it, I mean the, the leap and leap really is the only word from what I'm accustomed to, to this it's it's like they're not even the same species in a, to B to be honest, it's a, it's a great, a great advancement. So I mean, whoever that guy is, you figured out how to make that, that liquid stable stuff is, is brilliant. Hey, have you ever used the Glucagon Isn't working on everything she's like, so the reason I asked is because while, while we were talking about this, he said, you know, we, we were talking about people administering it at themselves and I'm trying to think, I wish really trying to picture like, where's the tipping point where you're, it's gotta be, you know, it's not going to be one of those like, Oh, I got a little low, I need to eat something.
Scott (22m 10s): Obviously that's that's first, but there's probably a moment where you, I'm guessing, you know, imagine you're on a CGM and you see, you have double arrows down in your 50 a and you think, you know, you do the math real quick and you think, Oh my God, I gave myself too much. Insulin I can't catch this, do this like this. Right. Yeah. That made a lot of sense to me. I I've definitely been in situations where I thought, I don't know if I'm going to stop this with food and you know, and that's for Arden, but I really thinking about adults living by themselves. Okay. Can I have a question that I heard you say a second ago you were talking about self-injection and I think that there are many people who might assume that Glucagon has only for when you are having a seizure or an unconscious, but how would I self inject if I'm having a seizure or unconscious?
Scott (23m 4s): So obviously that's not the only time to use it with when are the times I'm supposed to be using this or, or I'm able to.
Ken Johnson (23m 11s): Yeah, I think that that's a great discussion. Thanks for raising that point. So I think, you know, there are a number of settings. Everybody has their own personal experience with what they deem very low blood sugar. I think you, in some of your colleagues have taught me this phrase, the, I don't know, low. Right? And so when that happens, it could be because you are looking at your numbers, it could be because you start to feel differently. And you know, some of the sort of classic signs and symptoms are, you are shaking. You're dizzy, you confused, maybe you haven't changed your personality or, or more combative, you know, trouble answering questions. Those sorts of things are all kind of hallmark sciences I'm going low.
Ken Johnson (23m 52s): So when that starts to happen, of course, the first rule of thumb is try to correct it with food or drink, right in your favorites. A source of glucose for many, many decades now has been referred to you as the 15, 15 rule, you know, take those 15 grams and the 15 minutes and see if it's work, if you're improving. So that's one situation maybe that isn't working and it's a stubborn lo and you know, you're starting to now wonder what's next. So that would be a time to consider administering Glucagon. And I think most people would not have reached some state of incapacitation where if they were familiar and able to a administered the auto injector where the prefilled syringe, they can, there are other settings where people are unwilling or unable to swallow or to have enough, you know, stuff available.
Ken Johnson (24m 43s): Maybe there a place where they don't even have access to a source of glucose. That would be another situation. If you feel like your passing out and there's somebody with you, obviously you'd want them to be able to administer it so that the community discussion, he should know the other people in your life, be familiar with where, with the gun it is and how to administer it. As you pointed out this HypoPen auto injector, it's a super intuitive and the instructions are printed, write on the pouch. And so I think if somebody found you and you said, you know what to use it, you know, it's going to be very straightforward process. We have tested that and found that in simulation exercises where someone is going through simulation or of an emergency in a very low blood sugar, they were able to administer correctly 99% of the time, follow the directions and do the two step process that you just talked about.
Scott (25m 34s): When the, when the trainer arrived at my house, I took it out of the packaging, took the instructions away from it. I handed it to my wife and said, I told her what it was. And I said, don't even think about it, try to use it. And it didn't take her 10 seconds to figure out what to do with it. And nobody here has ever used, you know, an epi pen or anything like that. So we've never held her or seen anything like this before. And I made me feel like, I hope my insurance company will cover a bunch of them or spread them all over. Arden was a college experience when she leaves for school. For me, I'll just, I'll just put one everywhere. It just really was intuitive. Is the word for it. It's you can't look at it and hold it and like eat.
Scott (26m 16s): There's no other thing to do with it. I don't know if that makes sense or not. You know what I mean? Like it feels like there's just one way to accomplish something and it, and it shows you that while you're holding it, like you said, it's in the instructions, but I'm seeing when you have the physical things in your hand, it's not like there's seven levers and you've got to decide which one it is. It only does one thing. And then, you know, if it does it well then perfect.
Ken Johnson (26m 37s): You know, I think, you know, that was part of the design, the understanding there's a whole area of science, human factors, research the services. How do we approach? So to solve a problem. And, you know, there's very, very intentional features built into that auto injector. The colors are intentional, the little window that you have that shows the liquid Glucagon, you know, in there. And it disappears. It turns red when the dos has been delivered, that's intentional. The clicks that you hear, those are intentional to let you know the sort of audio queue that the cycle it has been completed. We also have safety built in when you finish the injection and withdraw the plunger from the bare skin, it locks out.
Ken Johnson (27m 19s): And so you cannot have a needle stick because there is a needle inside the device, but it's, you know, never appears during the process of the injection. And when you're finished is locked out. So you can't have an accidental needle stick. Can I ask
Scott (27m 32s): Where can, can you just inject it? I mean, anywhere, like where has it, where did you, where were you able to get the FDA approval? And how do I remember that when I'm going low? Like, you know, or is it just anywhere I can get it into me is good.
Ken Johnson (27m 47s): And we, we concentrated on three areas, thigh, abdomen, and your upper arm. So we figured out, in most cases, one of those is going to be readily accessible. If you do have to have bare skin, because we want to make sure, you know, this is a 27 gauge needle. We want to make sure that there's nothing sort of inhibiting its path as it goes into the skin. But you know, we, in our assessment, Scott, most people opted for the abdomen. I think it was probably an easy to just pull your shirt up. And most people have an adequate real estate there. So, you know,
Scott (28m 20s): If I'm going to say I'm okay, I don't, I might all need Glucagon, but I'm a, but I definitely have a place to inject it. So,
Ken Johnson (28m 27s): So, so any, any of those three sites and it didn't matter, you know, the results, the clinical changes that we saw were the same, regardless of psych.
Scott (28m 35s): Well, that's even, that's very exciting because like I said, for people who know about older products, it's a, we were always taught, you know, deepest part of the buttocks, you know, like it's a, it's a big needle, you know, it's a, it's not an exciting, not an exciting endeavor for certain. So even that's a huge leap is my insurance got to pay for this. How do I, I mean, that, that's part of your purview, right? When you were talking earlier about what it is, you're a, you've done in the past. And so you, I'm assuming you have some background on this. You can talk about it a little bit. Yeah, I do.
Ken Johnson (29m 10s): If you know, and you never want to have a drug approved, but then not have any access for people. And so, you know, that's an important contribution that the company had to make in terms of going to insurance companies, going to pharmaceutical benefits management companies, you know, very close to the time of our approval last September and have these discussions about why it would be so critical to be able to offer this new a much easier, much more approachable version of Glucagon and the one they have been covering. So there wasn't any restriction on your Read KIS. And so we ask, can you give us the same treatment? And I'm happy to report as we sit here today for a commercially insured individuals, if you have unrestricted coverage at 87% of plans in the United States.
Ken Johnson (29m 54s): So almost 90%, wow. That, you know, why isn't it a hundred, there's no product that ever has a hundred. So there's always some small portion where there's going to be additional requirements. So that would mean that you would probably still have a copay and everybody's plans are different. These can be very, but you won't get one of these not covered types of messages. And the 87% of covered lives in the United States for commercial insurance. If you look at Medicare, probably the next biggest segment for people with diabetes, who should have Glucagon is about 80%. And then we're still working our way through the Medicaid requirements and were about four to 30% on Medicaid.
Ken Johnson (30m 37s): So if you know, for most folks, your not gonna have any significant access issues in terms of affordability, we are right now, if you go to glucagon.com, you can get all the details on a copay assistance program. And the net effect of that Scott is you would have a $0 out of pocket for the HypoPen for the, for the present time. So we're, we're starting out the launch of the product, offering that additional support, which means if you say had a $30 copay and you qualify it for the program, the company would subsidize at $30. He is essentially received it for free.
Scott (31m 15s): That's excellent. A great what was the,
Ken Johnson (31m 17s): The webinars Gvoke glucagon.com. It's GV. Okay. Now I've had a few people say, gosh, how do you pronounce that? But a GV. Okay, look again on.com.
Scott (31m 29s): Glucagon.com. I got it. And I'll put it in the show notes so people can find it too. So if someone's using a different Glucagon right now, and they've heard you on Thank I'm would like to try this, do they wait to their next appointment, go to their doctor and say, I want to switch my Glucagon are, or what are the pathways to making the change?
Ken Johnson (31m 49s): Yeah, I think any of those might work. I think traditionally, when we need something new, we would contact her in health care provider and se there's a new Glucagon and it's called Gvoke HypoPen. Can you send me a prescription for that? Can I get a film, our experience with clinicians if they are pretty well aware now, but this is a configuration that's on the market. We've been working hard with a professional society's and through their channels to make sure that they know that as a personal Diabetes requested that they would, you know, no of it and not be afraid to read the prescription because have the access issues. Now you have also been cleared that makes it very easy for them. So it's not very cumbersome if you don't want to pursue it that way and just make a call to the doctor's office, usually does not require a visit.
Ken Johnson (32m 34s): Scott it's just a, you know, a new script is an issue from the electronic system. You can pick it up. That's your favorite pharmacy. You can also go to the website and we've set up some services. They're a little bit more analogous to kind of ordering online and you can enter some personal information or information about your doctor. And we have support services available now through pill pack and Amazon company that will work with your doctor in deliver it to your home at no cost.
Scott (33m 5s): I'm not sure I heard you, right. Is it PillPack?
Ken Johnson (33m 8s): Yeah. So the Jenny that helps assist in sort of the transactional part of this is PillPack. It's an animal Amazon company. A but the easiest thing to do is to go to
Scott (33m 50s): Right? So if someone listening just feels that economically they can't do this, they should be able to and contacting you is the way to go.
Ken Johnson (34m 1s): It is. And I think Listen, there are, there could always be some leg and whether or not the coverage policy has caught up and maybe their getting a strange answer about how much their out-of-pocket would be and things like that. We have a whole assistance program in place to help navigate that. We know how frustrating that is, you know, we wanted to make Glucagon easy to use, and now we want to make getting a prescription filled, easy to do. So, you know, we have very, a nice set of services that are linked to the website. There's also a phone number at the website. And in case it's easier just to call and talk to a real human, but you know, that takes you through a whole tiered process of, you know, is it going to be covered?
Ken Johnson (34m 42s): You know, what pharmacies have it and so on and then write down to even, so the patient assistance programs for folks who can't afford their medication,
Scott (34m 53s): The concept of having to mix Glucagon stopped us from using Glucagon when Arden was legitimately having a seizure. I just don't know that. I mean, you know, technology's better now, obviously, and that's great, but I don't see, I can't imagine going backwards on this one, like this to me seems like the best it's available. Right. I was wondering, do you hear from people about mixing and what did they, what are the responses? Do you think that that having to mix the Glucagon stops people from even considering it as an option? Sometimes
Ken Johnson (35m 33s): I think given that that was all of that, there was all that was available
Jenny Smith, CDE (35m 39s): For such a long time. I mean, you know, again, thankfully my parents never had to deal with that. They never had to mix it. They never had two. It was always there. He always knew where it was in the house, but I, I would say that it's certainly a deterrent to use because it's, there are just the extra steps, again, as you brought up in your situation, it's like having to think through those steps when you got your loved one, either having a seizure or you've discovered them completely like not with it at all out, can't talk to them, whatever your brain is thinking in terms of helping them.
Jenny Smith, CDE (36m 24s): Yes. But all the steps of mixing, making sure it was mixed right now, you've got in the needle on that. I mean, this is scary looking needle, compare it to a syringe needle for Insulin. It is, it's a bigger needle, right? So, you know, imagine putting that into your two year old or even your 12 year old child and knowing that you're doing it the right way. And I can say that it would be a it's a deterrent, although I dunno, in the case of not having anything else as an option, you figure it out, but it's certainly going to be,
Scott (36m 58s): Well, I have a friend who recently had a teenage son, a have a seizure and she got the red box out. She got it mixed. And when she went to draw it back out, like in the, what your describing, running upstairs, people yelling, she broke the needle off in that crazy. So they had to go to a secondary option, but they were getting ready to use it. And she, she was trying to traverse there's and mixed Glucagon at the same time she was running to where it was happening, you know? And I think, I just think that that's the point, is that anything that simplifies that is genius and putting it in, you know, what can be described to people who don't know any different?
Scott (37m 44s): Is it as an epi pen style? Like just this thing in your hand that you just push down and hold this, turns it into something people can carry with them.
Jenny Smith, CDE (37m 52s): Absolutely. I even think two from a school type setting, even the comfort level of, let's say for some reason, you know, technology is down your not able to contact the parent. You don't know exactly what to do. I mean, from the standpoint of safety and feeling okay, and teachers or the Peros or whoever's helping at school, this is a hundred percent easier.
Scott (38m 17s): I think this takes away from that thing that a lot of people who aren't, who know, who have kids know, you go to school and you're like, I need somebody to be a Glucagon advocate from my kid. And everybody's like, no, thank you. You know? Like, like they really do too, like teachers, or like, I don't want to be on the hook for this, but, but this is like, again, I think this takes away the possibility that they can make a misstep in the middle, like drunk when Arden was a little, her, her directions were drawn up half the vile. You should have saw the fear that put on someone's face. Well, how do I measure half of the vile? I'm like, I don't know. I bought it. And they're like, what? I'm like, Oh, here we go. This is fine. After I get either the prefilled syringe or the HypoPen, how long do they last until they need to be replaced?
Ken Johnson (39m 4s): Yeah, that was part of our design criteria. We didn't just want to make a liquid ready to use if you wanted to make sure it could last a long time because you know, hopefully once or twice a year event and most, and even if it's a never event, you know, let's do not have to replace it too often. So right now, from the time of manufacture to the end of life or a potency, a sufficient for a re restarting, the blood glucose it's two years, but it's a very long shelf life. You know, we, again, you know, that was part of the design process and certification process and approval with the FDA that we have a two year from time to a manufacturer expiration.
Ken Johnson (39m 46s): So that'd be printed on that other product. You'll know when it expires a number of pharmacies. Now you can have reminder programs. So, you know, it's time to get at all.
Scott (39m 54s): Can I have to tell you? And I genuinely mean this. I've spoken to a lot of people who work for peop you know, manufacturers of different drugs and devices, and that's the first time anyone's ever said anything to me that almost knocked me off of my chair. I just took two years. Is it's amazing. And not what I expected you to say. That's because what I was going to say is, you know, we got the prefilled syringe, and I had a question about that actually, before I go down my story, we got the prefilled syringe and it comes in sort of a pillow bag is my best description of it. And my first thought was, huh, there's a needle in there. And this is sort of a bag. And then when I reached out to the people who are listening to the podcast, that was actually a question they had was, you know, why does the like, explain to me why the, the needle is safe in this bag?
Scott (40m 41s): And I guess, I guess thinking couldn't it be deployed, but to answer that for me first, obviously you didn't make something and not think, Oh, I wonder, you know, I'm assuming it's been tested, but explain to me how you came to the, the packaging for the prefilled syringe.
Ken Johnson (40m 56s): Yeah. It serves to a number of purposes. The packaging is a sealed foil pouch. Its done a very, a controlled environment. The prefilled syringe that if you describe Scott actually has a noodle shield on it and also has a backstop to keep the plunger from being deployed. So why a pouch? I think you started with that question. So first of all, the instructions are printed on the pouch and we want to make sure because you know, the real estate on a, on a prefilled syringe where the real estate and the auto injector is not sufficient to describe how to use it. It would be six point font and we wouldn't be able to read it. We have these very clear pictures and words printed right on a pouch that could tell anyone how to use it.
Ken Johnson (41m 42s): In fact, we tested that we have people who are untrained in the administration of the prefilled syringe and the auto injector and they successfully administered it. You know, like I said before, 99% of the time. So the second is that foil and the gas that we pack it in inside there. Cause you notice its like a pillow because its actually has a pressurized it's in there helps with and moisture because those are the enemies of any drunk. It doesn't matter if it's Glucagon or anything else sort of protecting it from light and moisture helps contribute to that two year shelf life. So we, we can't stress enough that you should keep it in these pouches until the time you use what people are.
Ken Johnson (42m 25s): You know, people may say, well, it's, here's how I know what to do. What's inside the pouch. So that's why we've provided videos. That's how it could be provided the demonstration units. Like the, when you have, you know, they'll be available in the clinics. Doctors have been requesting those demonstration units. So if there should be no mystery about what's inside the pouch, but we do acid if he started in that until the time of use and it's, you know, so multifold purposes for having that pouch
Scott (42m 52s): Is it all makes sense. It just, and had, I probably thought about it longer, you know, what it really is is that it was just different and so than what I was accustomed to. So when I saw it different felt wrong and now you explain it to me and like, Oh, well different seems like more well thought out in a new and better. So a that's excellent. Can I give you
Ken Johnson (43m 11s): If you want to anecdote as we were testing that power and sort of the size of it and how big the print was and everything else, we've had a number of Diabetes educators as a part of our forum for focus groups. And there was some that wanted it even bigger because they wanted to write all kinds of instructions and the margins and the doctor's phone number and you know, reminders about other things and stuff. That's like at some point we had to say, no, you know, we can't add to it, this giant pouch, it's gotta be small enough and portable enough. So, so, you know, there, there were a few rounds of the things that, you know, let us to the current configuration,
Scott (43m 41s): If they did, they have it up to the size where you could put three holes in it and people get carried around in their binders.
Ken Johnson (43m 47s): They're, you know, so, so know is all intentional and a contributes to the, the long shelf life. It contributes to the successfully administering it and at the time of emergency and it also protects the product
Scott (44m 1s): Going back to the beginning of this thought for me, what I was getting ready to say, when I asked you how long does the product last before it needs to be replaced? What I was gonna say as I think I'm going to get to move on to the HypoPen afterwards, because I can see how, you know, it's just, it would just make, I think this would be easy to show my daughter and say, look, if you really feel like you're in trouble, do this. And it wouldn't feel like, you know, a rigmarole I guess, and, and, and maybe off putting in any way. And so I thought I'll switch, but now I realize I've gotta wait two years. I switched. So a, I M
Ken Johnson (44m 34s): You bet you brought up another issue and that is keep people, staged them at different parts of their daily life. Right? If you keep the prefilled syringe and the nightstand at home, you might have the auto injector at school or with the coaches or wherever. So, I mean, you know, mix and match again. There's no difference that in the Glucagon is contained any of their device for the product.
Scott (44m 55s): No, no, no. I, I, and I, I guess I was half kidding, but I do know that, you know, there are different Podcasts if our kids ever grow back to school, she'll need one for school in, in a couple of other places. And it just, you know, I can't, I can't say it enough, it's the, it's easy to have you on the show and talk about it. Because like I said, this is a leap and this is going to make people's lives. I think easier if they should ever have an emergency and need to use it. And I think the comfort they're going to get from it, just having it around Is is going to be different. I, you know, I really don't mean to pile on somebody, but that, that red box is not comforting. It's off putting, and this, this thing I'm holding this pen here is comforting. So there's a lot to that.
Scott (45m 35s): There's a lot to the psychological, the psychological side of all this. And I appreciate that. That was considered,
Ken Johnson (45m 42s): You know, we've talked with folks sort of who lived through all of this and seeing the changes in technology and new delivery. Insulin certainly advanced and the bringing forward CGM pumps are, you know, all these things have been stepwise improvements. Glucagon just, wasn't tackled. And, and, and now that we have, you know, we want to keep making improvements and exploring other other uses for it and beyond the, the, the currently approved one. And so the companies, you know, vested in making the most of a liquid ready to use Glucagon. And so, you know, stay tuned for more. Now
Scott (46m 20s): That as I was jumping on this call, I got a message from somebody. It was so funny. They don't know the timing of my schedule, but they just were like, if you, if you haven't spoken to the people at chief Oak, yeah. Can you please ask, is there a water and Insulin and if there's water and insulin can, can, Insulin be made more stable with their technology. And I was like, I dunno, I'll find out. So I, maybe my bigger question is, are there other things your stabilizing over there, or, or you just the Glucagon company, or is there more,
Ken Johnson (46m 54s): You know, we are more than a, Glucagon a company. So at our core, we want to take the technology to make liquid ready, to use easily injectable, very stable products and all of the areas where it makes sense. We have talked about it Insulin and it's a, it is a project and it's not anything that's a, you know, advanced in terms of it's Clinical Development. But we do recognize that there are limitations on the storage conditions for Insulin or other things that it can be mixed with cost problems. So maybe we can start to combine it with other effective, low blood glucose agents and make a better combination. So, umm, the, the short answer is yes, we can apply our technology to a broad range of drugs, proteins, monoclonal, antibodies, vaccines.
Ken Johnson (47m 42s): And so, you know, that's, our mission is to take all of the concern and the difficulties of administering and storing and drug out of the equation. And so that's, that's kind of the, the future state of zero S and, and how we'll apply ourselves. But you know, us now as the blue thing, as a company first and foremost, and a, you know, and we'll use that as a starting point and grow from there,
Scott (48m 5s): Your technology applies to a lot of other things. So they're, there are probably many things that we can't talk about that are being considered there. And I'm asking that question as a wink and a nod to all the people who asked me questions that are not covered by your FDA approval. So I can't ask you here, but they'll all understand where they hear this and be excited that you're working on other things I think is that fair?
Ken Johnson (48m 28s): Oh, that's definitely fair. And our company website to a separate from a DeVos glucagon.com describes some of our pipeline and the things that are still in an experimental phase. And you'll see that it's, Glucagon, it's a drug called die as a pan for seizures in other programs. So we're, you know, we're, we're really interested in applying this technology broadly and solving problems for patients and their providers,
Scott (48m 55s): If it's possible that I'll ever be able to get G Voke in a vial for home use to just keep and administer as I need
Ken Johnson (49m 4s): What we would like to pursue that. Yes, I think, you know, there are a number of applications of Glucagon that are different than our are approved used today. It's a one milligram, you deliver the whole dose, a in the setting of restoring very low blood sugar, but there are other settings where maybe the smaller dose would be useful. And, and so there or other settings, whether it's exercise, whether it's hypoglycemia, unawareness, other things were, there are a series of, you know, Clinical Development projects that we've sponsored. We've collaborated with one side as well as a part of a dual hormone delivery with Insulin and Glucagon as part of a closed loop system.
Ken Johnson (49m 45s): So in a, none of these are approved, none of them are a possible with the current configuration. We would need a vile of Glucagon as you describe the Scott. So it'd be very similar to how you would administer Insulin. He would have personalized doses for the situation that your trying to manage. So that's gonna take us some time, but we are investing in those efforts, you know, just ask everybody to stay tuned for more.
Scott (50m 10s): All right, well, I'll say this from my heart and many people may or may not understand this. And I guess if you've been around Diabetes long enough, if it makes sense, but it may not seem super exciting that someone figured out a way to make Glucagon liquid stable, but is super exciting and that it opens many doorways and possibilities for the future. Everyone who has someone that they love with type one diabetes or has type one diabetes, should be incredibly jacked up and excited that you guys figured this out. And I know that it, it's hard to wrap your head around why this is that exciting, but it is. And I'm, I'm very much looking forward to what happens next. So I really appreciate you coming on and explaining all of this.
Scott (50m 52s): And I thank you for your time, unless you want to play some piano. I think we're good.
Ken Johnson (50m 57s): My pleasure. Scott I enjoyed it and hopefully we can do it again sometime. And my best to Bailey you left the room,
Scott (51m 8s): Dammit, cameo bark. So you'll have to cut that part. So I thought I could get a little park at the end and we'd be finished anyway. Thanks so much. Enjoy the rest of your day. Really appreciate your time. All right. Appreciate it by huge. Thanks to G vote for sponsoring this episode and for giving me the opportunity to just speak with Ken and a huge thank you to Jenny Smith for being such a good friend and coming on the show to talk about Gvoke. If you'd like to find out more about you Vogue, there are links right here in the show notes of your podcast player@juiceboxpodcast.com or you can just type the words
Scott (52m 1s): I have a little bonus stuff here at the end for you. If you'd like to keep listening, I actually spoke to Ken the day before we recorded this just for a few minutes, so we could get to know each other. And he told me about his piano playing. So I brought it up at the beginning of this recording while we were getting the audio set up. So it was recorded, but not really a part of the episode, but I left it here. Cause it's interesting. What kind of music do you apply? So,
Ken Johnson (52m 28s): Oh, I'm like what they prefer to, I guess, as a professional journeymen, sidemen I'll play whatever, whatever comes on my way, I read music, you know, I play from classical to jazz, to tribute acts, including pink Floyd and van Morrison and a REIT, the Franklin and two classic wedding bans. You know, the most cliche kind of lounge music. You can imagine it doesn't really matter a musical theater,
Scott (52m 55s): The multiple instruments or not.
Ken Johnson (52m 58s): I'm a piano player, keyboard player.
Scott (52m 59s): That's really, that's an amazing skill to have. That is very cool. And it's great that you get to do it too.
Ken Johnson (53m 5s): Yeah. So Chicago, you know, traditionally has been famous for lots and lots of live music. And of course, many famous bands have come outta here, but we're a complete shutdown now. It's just awful.
Scott (53m 18s): And online really doesn't replicate it. There's been, I think one or two people who have done it well, you know, and it's, you know, you have to, you can see how much money you have to have a, in a crazy example is that, I don't know if you saw, you may not like this kind of music, but maybe you do. You mentioned pink. Floyd Metallica did an old song acoustically remotely. So all four guys were in a different place, but it sounds like it was recorded in a studio. So you have to assume that each one of them has a professional recording studio in their home, you know, but that worked out, but,
Ken Johnson (53m 51s): And that's exactly how they do it. And what we are led to understand as consumers is they record all those tracks independent of each other, and then somebody who mixes them because you can't, you can't use zoom to have simultaneous music because whoever's talking to the loudest takes over the channel. And so there's, there's no mixing up on zoom. It's a, it's a big problem.
Scott (54m 12s): You know, all that equipment and the willingness to spend a couple of million dollars to mix a song together to release it. And they had that money and they did it. And everyone else is just like you said, fumbling through trying to do in a resume for those of you who are not familiar with a podcast and don't know who Jenny Smith Is I thought I'd take a second to let you know Jenny is a frequent guest of the show. She's helped me put together series within the Podcast like defining Diabetes, ask Scott and Jenny. And of course, the very popular Diabetes pro tip episodes and of all of the people I could have had on those episodes with me. Here's why I picked Jenny. Jennifer Smith has had type one diabetes for over 30 years since she was a child.
Scott (54m 53s): She holds a bachelor's degree in human nutrition and biology from the university of Wisconsin. She is a registered and licensed dietician, a certified diabetes educator, and a certified trainer on most makes and models of insulin pumps and continuous glucose monitoring systems. I love Jenny. She is a friend. And when I decided to do this episode, I asked her if she could help out a little bit and she was very gracious and said, yes, Jenny works, has integrated Diabetes so you can check her out. If you do, like@integrateddiabetes.com.
Please support the sponsors when you’re able and it makes sense for you. This episode was sponsored by Gvoke.
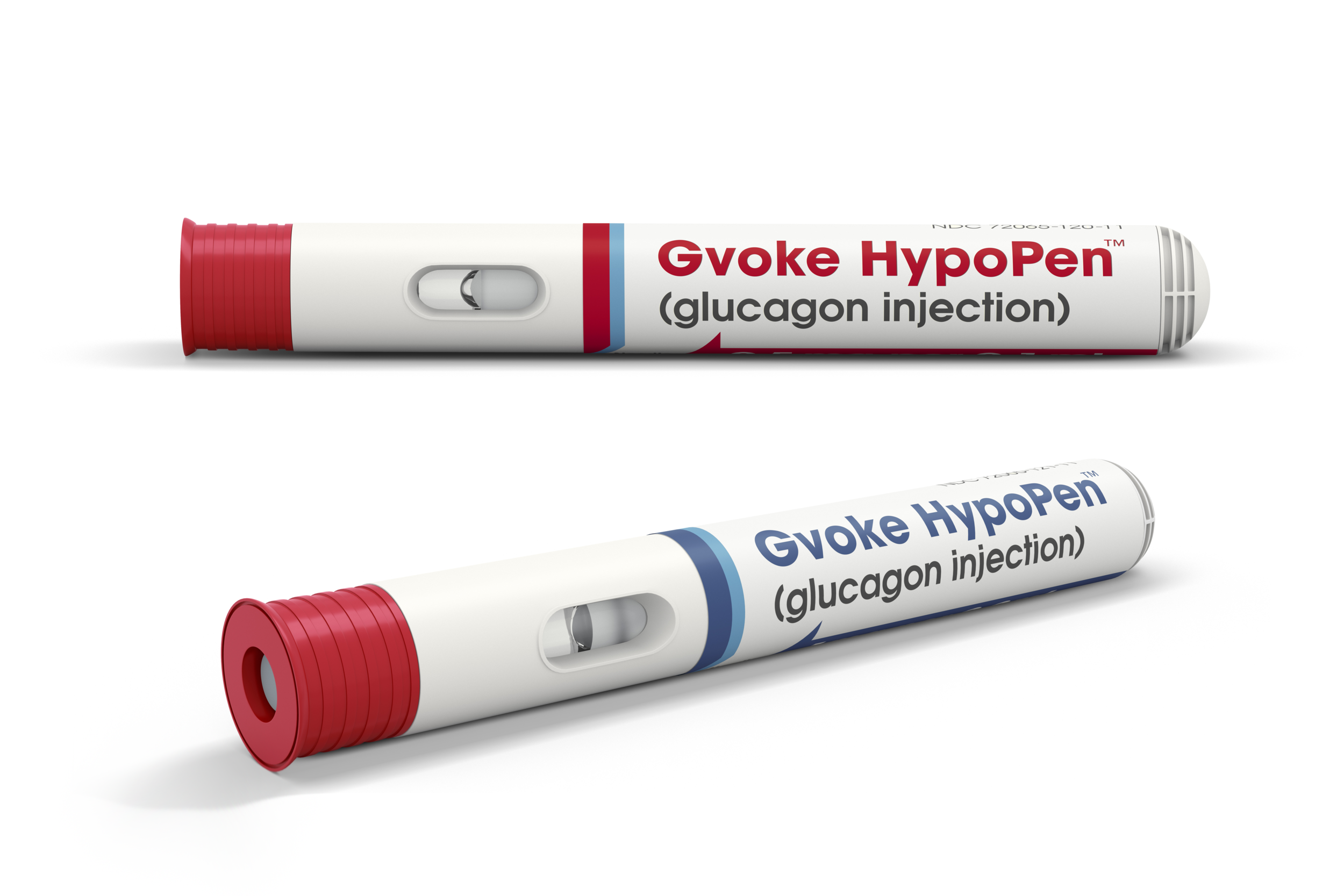
LEARN MORE about the HypoPen and other Gvoke products HERE
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!




























































