Living Between the (Diabetes) Lines
Three questions that every person living with diabetes asks themselves...
How high is too high? How low is too low? How do I find the balance between long-term complications and having a seizure.
Each of us has been given a range to aspire to. When Arden was first diagnosed, the doctor told us that we should be trying to keep her blood glucose value between 110 and 200 - "let's try to keep her A1C under 8.5", they said.
And so that became my goal.
Then one day they told us that we should lower the high range value to 190, at our next visit we agreed to try 185. The low range number was never touched. I understood what was happening even though it was never articulated to me, our BG goals were adjusting based on the vibe that our Endo got from us at each visit. She was evaluating our ability to handle spikes, lows, meals and overnights. I was being lovingly manipulated.
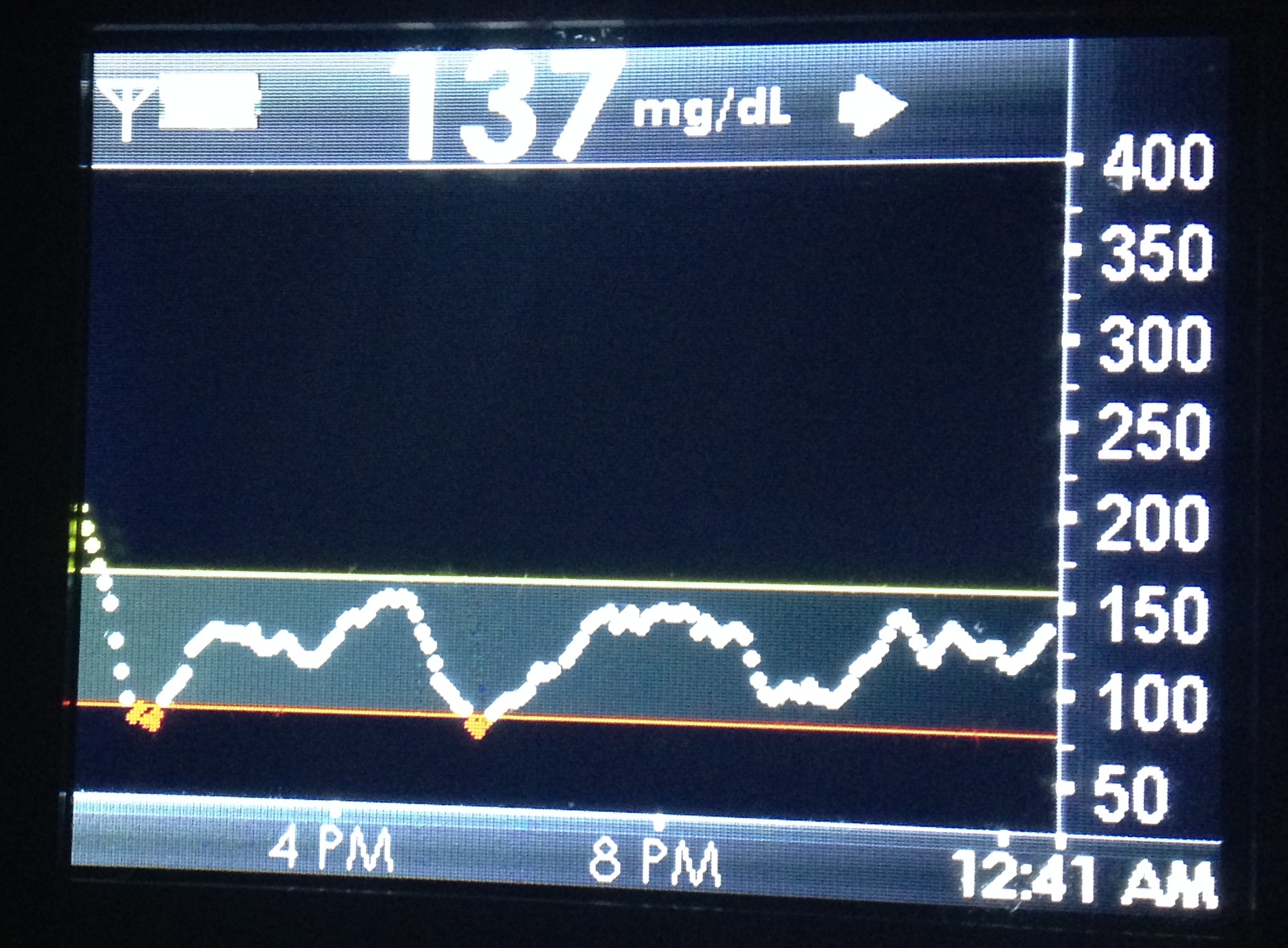
Then one day we discovered CGM technology and that little screen gave me something that I never had before, a visual representation of our goal. Now there was a line that I was trying not to cross. In the past when our goal was 190, 210 didn't seem like a huge miss and on the low end... even though we were trying for 120, 100 seemed so perfect that we didn't mind being a little low; besides many people, who don't have diabetes, regularly have a BG of 85 - of course they don't have man-made insulin in their system that doesn't know when to stop removing sugar from their blood.
I was living between the lines but I think the lines were holding me back...
I say holding me back because Arden's BGs were, for the most part, existing between them. I'm not talking about unforeseen spikes or unexpected lows. Highs and lows happen, you correct and move on, but you don't let them impact your impression of the graph. A few blips don't discount the rest of the day. Look at how the BGs are when you are blousing correctly, counting carbs accurately, when your basal rate is properly set. In those hours I was content if the graph line was mostly stable and in between 180 and 120.
It took me quite some time to figure this fact out, but the comfort that I felt when we achieved BGs that were between those lines, was holding me back from trying to do better. I had been lulled into a state of acceptance.
The lines were also providing a false sense of security. Even though they were arbitrarily set by a person that I only see four times a year, I was treating them like gospel. Finally I wondered, "if I can successfully keep a BG under 180 why could't I keep it under 170? Hell, why couldn't I shoot for 140?".
So I moved the line and do you know what happened?
I kept her BG under 160. Then I got brave and moved her low threshold to 100. Today, Arden's low alert sounds at 85 and her high is set at 160, but this summer I'm going to move that to 150.
All of this doesn't work if you punish yourself for going outside of the lines. I am telling you, do not do this if you can't handle seeing the graph climb above, or below those lines - don't add stress to your already stressful day. Before you attempt to move the lines you must find peace with being on the other side of them, you have to come to grips with the idea that nothing in life is controllable to that degree. Here's how I found my peace with that truth.
I was happy if Arden's BG was 180 all day because someone told me that number was okay. Her BG still spiked, it still got low but for most hours of each day her BG was 180. Today, most hours of the day come with a BG of around 140. She still has spikes and still gets low but most hours are spent in our new range. It took me a while, but now I can see, there is no difference in how I manage or what I do; the only thing that has changed is my expectations and the way that I react to them.
When I expected 180, I got 180. When I expect 140, I get 140. I'm learning to except 90... one day I'll learn to expect it.
When you're ready, move those lines... the ones on your CGM or in your log book, and the ones in your mind and heart. Expect what you want, except what you achieve and never stop moving the lines that life sets. Define your own reality.
Don't forget to read my disclaimer, I am not a medical professional and I am not dispensing advice... just telling stories on the Internets, the WWW, the information highway - you get what I'm saying. Please also don't forget that high and low ranges are never one-size-fits all. While Arden feels fine when her BG is 85, you or your child may not.
Helping Children With Diabetes Gain Independence
Part 5: Taking It One Moment at a Time
The word independence literally means, “Freedom from outside control or support.” But when we use it to describe a child who lives with type 1 diabetes, the word takes on a much deeper meaning.
I wanted to say, “Children struggle,” but in all honesty, all people struggle to be themselves every day. We are influenced by so many outside pressures that I often wonder if any of us are really being who we are. On any given day I can feel too short, too fat, too old or just not smart enough. I worry that my affections won’t be reciprocated, that I am not being a good parent, husband and son. In the past, my concern about loved ones’ reactions have stopped me from telling them how I truly feel. Yet if you asked me to describe myself and the level of independence that I felt during that time in my life, I would have told you that I was not bothered by what other people thought of me, that I didn’t feel the pressure – but of course I did.
As I sit here and write to you, I realize that I felt all of those things when I was younger and I wasn’t wearing an insulin pump or a continuous glucose monitor. I didn’t have to stop and check my blood glucose all day, people never felt obliged to tell me what to eat and I never once thought that I may pass out from not paying attention to my moment-to-moment health. Young Scott was living a pretty easy life, and yet he still felt the proverbial weight of the world.
So how the heck are we going to teach our children with diabetes to feel independent? I think the answer to that question is, one moment at a time.
I could have written a series of blog posts about helping children with diabetes gain independence through any number of experiences. I believe that people, young and old, have potential and that all they need is patient loving people to surround them with quiet strength and support. Sure, sometimes it feels good to be told that someone has your back, but often it feels better to just know. Then when life happens, alone or together, we have the inner strength to shoulder what’s coming our way. In time, with maturity and practice, we begin to believe in ourselves the way that our loved ones believe in us.
So does technology help to build independence for children with type 1 diabetes? Absolutely it does! Does it do it overnight or over the course of a single year? No. Independence is a form of maturity and the process towards becoming a fully realized person is a long one. That kind of firm base is built one experience at a time and not every step taken is a step in the correct direction. Each blood glucose check in public will build confidence. Every low blood glucose conquered is a step in the right direction. There will be moments that don’t go as planned, but don’t think of them as failures, think of them as perspective for the successes. You can’t appreciate success without knowing failure, at least not to the degree that it requires to build maturity, and none of this can happen if we are being sheltered. I know as well as you do that having a child with type 1 diabetes is different and at times scary. That’s why I added technology to our daily routine; so I could give Arden the personal space that she needs to grow while protecting, as best as the situation allows, her health and safety.
This post is part of a six part series that I originally wrote for the Suite D Blog, which is operated by Insulet. Insulet is the company responsible for Arden's insulin pump, the Omnipod. Please know that I was compensated for my writing in an amount that would be considered standard for freelance blogging. My family pays for Arden's Omnipods with insurance and out of pocket cash. My writing for Insulet has no impact on my opinions or the information that I share here or anywhere online.
Fool proof tips for handling Halloween with Diabetes
Every year, just before Halloween, I receive a few inquiries about writing a freelance piece about 'How to handle Halloween with Diabetes' and every year I politely decline to write about that topic. Why... because I think it adds unnecessarily, to the hysteria that exists online surrounding this non-issue. However today I'm feeling kinda giddy... So without any further ado, here are the tried and true ways that we handle Halloween in our house, you may want to write them down so you don't forget.
- We count carbs and cover them with insulin.
- Due to the nature of how some simple sugars react to the insulin, we test more frequently.
- Walking can decrease a BG so you'll need to carry some sugar... hey wait a second.
Seriously, that's all we do though having a DexCom CGM does help. Tell you what, just so you don't feel ripped off for clicking on this blog entry, here's the stuff I would have written if I excepted those writing jobs.
- Trust yourself, you know what you're doing.
- Practice moderation.
- Test a little extra.
- Get home with enough time to allow active insulin to finish before bed.
- Check on your little ghoul a few times after they go to bed to make sure there's no crazy drop in BG.
- Relax and eat your kid's candy so you don't have to deal with this crap tomorrow.
Okay, well, that's it, except to say this to my freelance suitors... aren't you glad you didn't pay for that!?
Happy Halloween and don't forget to log your BGs and exercise with The Big Blue Test!
Pound the (Omnipod) Alarm
Have you ever experienced an Omnipod alarm that wouldn't stop?
Have you gone online to find out how to save yourself from the incessant squeal and receive tips like: You can open the pod and take out the batteries, put it in the freezer, hit it with a hammer, or my favorite... I put it in the driveway and ran it over with my car.
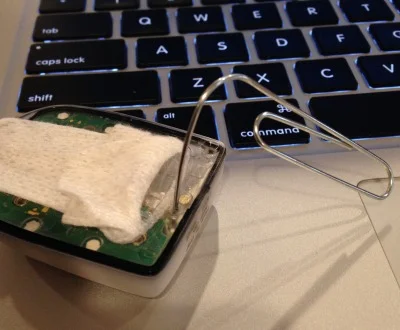
While I have to admit that a few of those tips sound like a great stress reliever, you don't really have to go to all of that trouble. All you need actually, is a paper clip. The new smaller OmniPod has a manual shut-off port (Just like the first generation did) for stopping that annoying alarm! If you'll refer to the diagram above that I borrowed from page 131 of the system documentation for the new Omnipod PDM Manual (Model UST400), you'll see where the port resides.
Just follow the instructions and don't forget to give the paper clip a firm push (It has to break through a thin layer of plastic) and the alarm will be no more. Best part? You won't slip with a kitchen knife as you try to crack the shell open and cut your finger off.
Be Bold and Pre-Bolus Insulin
This story begins in 2006 just moments after I asked Arden's nurse practitioner if she was "nuts".
NP: <blank stare>
Me: <incredulous gaze>
Only moments before our staring contest began Arden's NP became the first person to suggest that I give Arden her mealtime insulin before she started to eat. I can't be sure if she referred to the practice as pre-bolusing, probably not as we were MDI, but she definitely wanted me to inject before Arden ate.
"Are you nuts?"
I responded emphatically that I could never give Arden insulin before she ate. Arden was two years old and there was no way to be certain of how much food that she would finish. The NP repeated her very reasonable request but I could not wrap my head around this new idea. Pre-Bolusing, bah, Arden would be safer if I left her alone at the mall with money pinned to her shirt.
I was 100% correct on that day. There was absolutely no way to be sure of Arden's appetite. However the inability to guess how much she would eat wasn't the only reason I didn't want to inject before meals. Arden weighed maybe nineteen pounds at the time and Novolog had a way of peaking intensely in her body. She had already experienced a seizure from an insulin miscalculation that I made. That mistakes lesson was still very fresh in my mind and with that bad memory still looming over me, I just couldn't bring myself to administer insulin that wasn't already covered by food or a high BG.
Of course everything that the NP said made total sense. I wanted to give Arden's insulin a head start, I dreamt of a moment when her food would begin to expel it's carbohydrates just as the insulin was pulling her BG lower. I could picture that perfect image in my mind, a tug-of-war with food on one side and insulin on the other. Both combatants pulling furiously without once moving the rope that is Arden's blood glucose value - the dream of a steady mealtime BG. I wanted very much for that to be our reality and so I promised myself that I would make the adjustment when the time was right.
Fear and poor timing stopped me from taking the NP's advice all those years ago. Eventually the day came when I found my footing with the idea and gave up on being scared... that's the day Arden's A1c began to decrease.
We haven't looked back.
The beginning of our trip down the road to pre-bolus freedom was littered with pot holes. The first bump took some time to traverse, we first had to wait until Arden was old enough to give thoughtful consideration to her hunger. After that hurdle was cleared we took the first step, bolusing ten minutes before a meal. Those next ten minutes were the most tense of my day, I would test and worry so much after the bolus that I barely had time to finish cooking. Initial results were less than stunning so I moved the pre-bolus to fifteen minutes before a meal. The extra five minutes increased the impact of the insulin and lessened Arden's post meal spikes, but I still wasn't seeing a huge return on our efforts. I wanted to take the process to another level but I couldn't, in good conscience, give Arden insulin farther from the beginning of her meal. If only I could see the insulin work, I needed a crystal ball...
... or a DexCom CGM
Arden's CGM turned pre-bolusing into the most valuable weapon in our arsenal. It's one thing to have a good idea of how long it takes insulin to begin working in the body. But when you are able to not only witness the movement of the BG, but also the speed with which your glucose level is rising or falling... it's the difference between rumor and fact... between guessing and knowing with reasonable certainty. The day that my eyes were opened to the benefits of wearing a CGM, that was the day that everything changed.
Arden was 149 before dinner last week. I bolused for the elevated BG and pre-bolused for 50 carbs, it was a significant amount of insulin for her. Before DexCom I would have panicked and served the food in less then ten minutes. Now I take my time finishing dinner while Arden and Cole do their homework and leisurely prepare their plates as I wait for the CGM to tell me when to serve.
I put dinner on the table when the arrow on Arden's DexCom G4 turned south, waiting until her BG was below 110. The amount of time between Arden's bolus and her BG decline can vary most days depending on a number of factors. Glucose monitoring grants the flexibility to wait, providing a level playing field for the insulin and those scrappy carbs to wage their battle on.
At least now it's a fair fight.
Don't forget what the disclaimer says... Always consult your doctor before making changes to your health care. I am not a doctor.
More about the art: The art work displayed at the top of this post is an original piece from Mr. Mike Lawson. Mike is a tireless advocate for people with diabetes, a friend and extremely talented artist. You can find him working at TUdiabetes, on Twitter and through his fantastic YouTube channel.